To the Editor:
Papular acantholytic dyskeratosis (PAD) is a skin condition that typically presents as multiple, small whitish papular lesions that may coalesce into plaques; more rarely it is seen as solitary papules. Involvement of the vulva was first described by Chorzelski et al.1 in 1984; this form is most frequently observed on the labia majora of middle-aged women with no familial history of the disease. Cases of PAD of the penis, anal canal, and inguinal skin folds have also been reported.2–4 The condition is usually asymptomatic, although intense pruritus may develop. Histopathological changes include acantholysis with variable degrees of dyskeratosis, and direct and indirect immunofluorescence have been negative in almost all cases studied.5
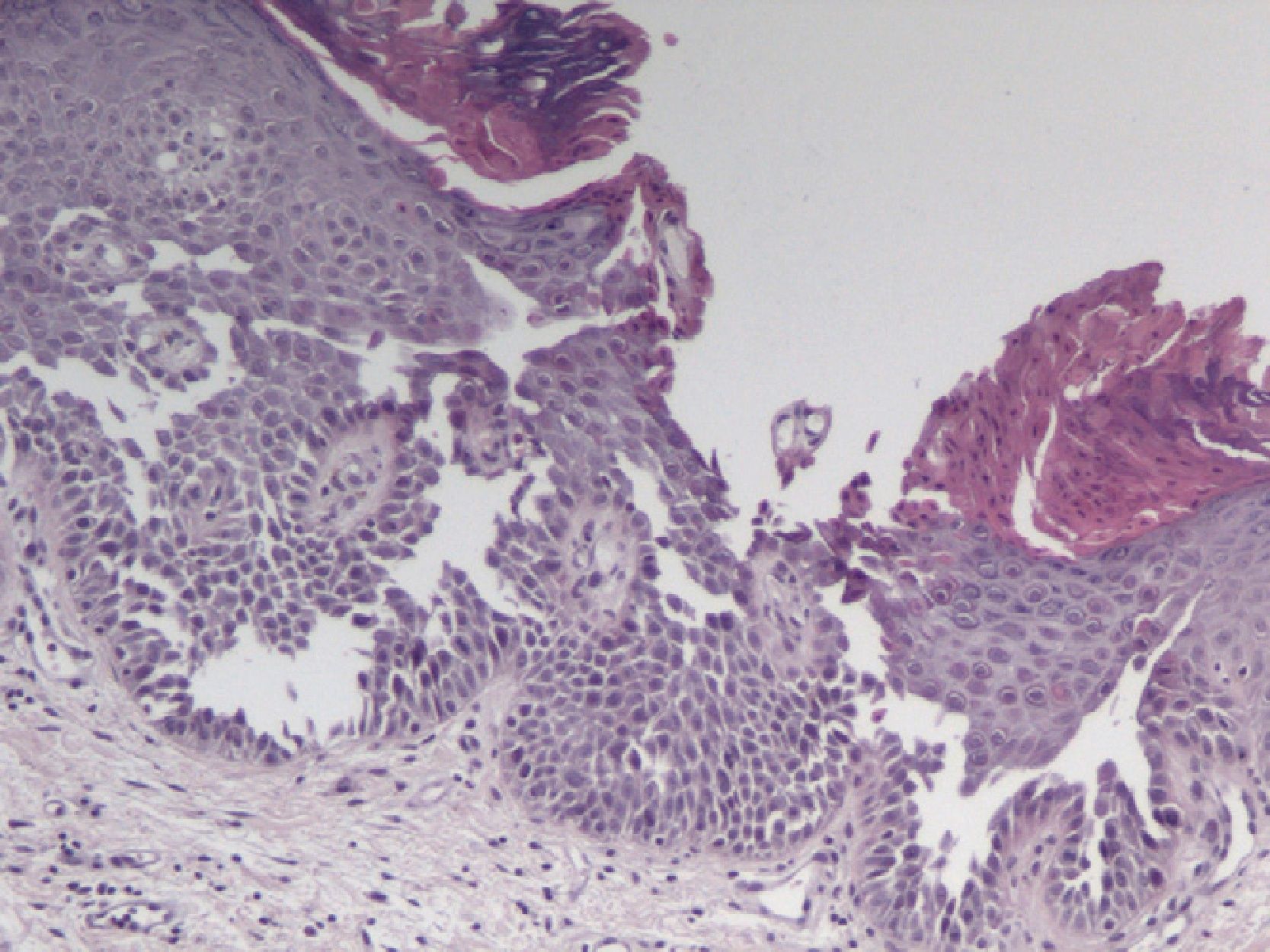
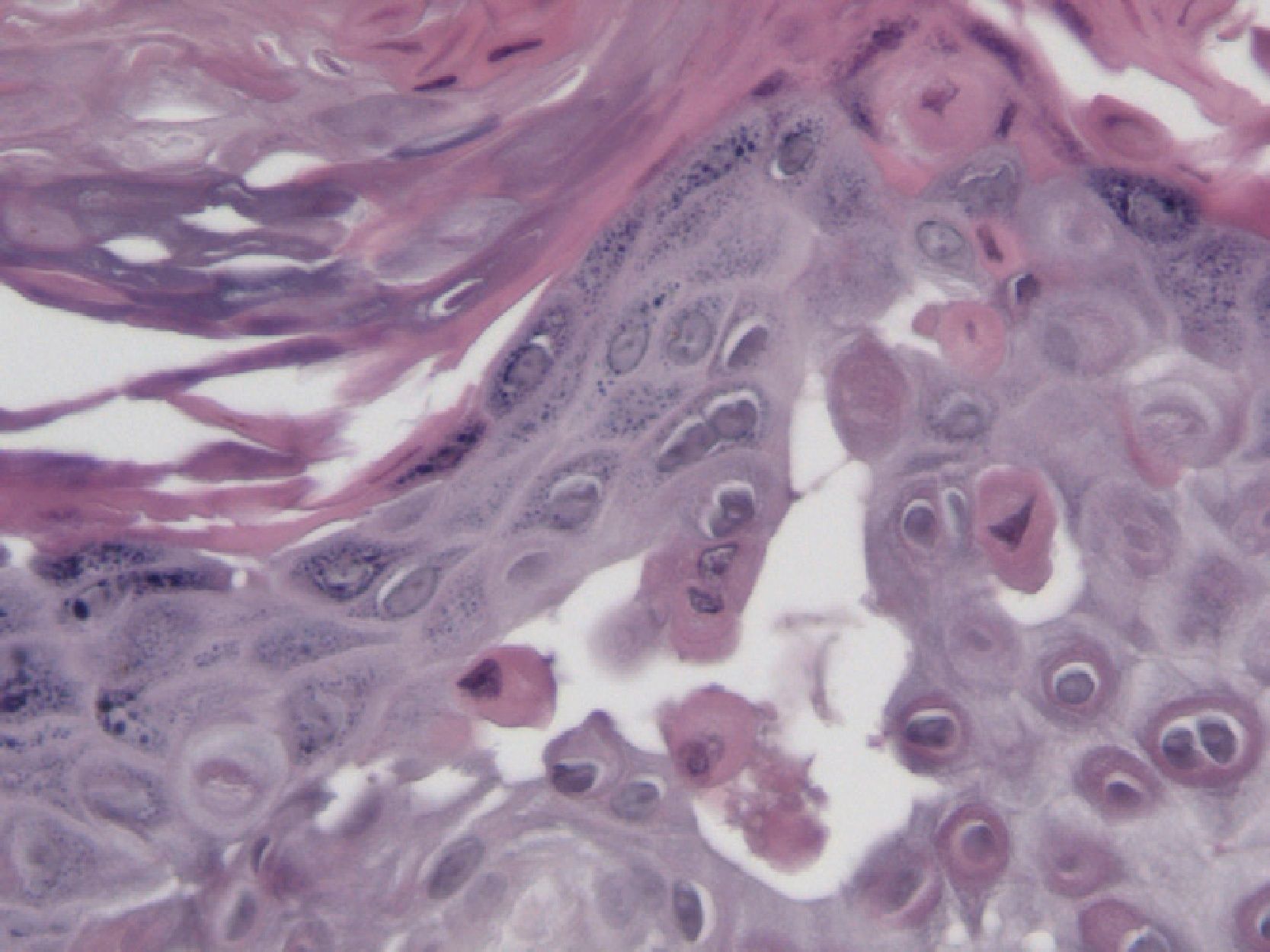
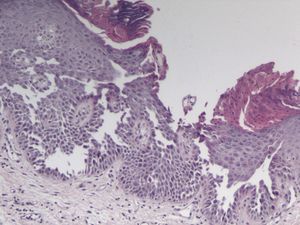
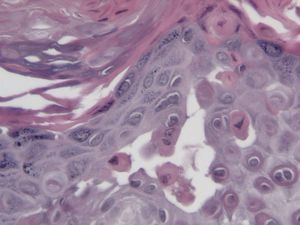
We present a 58-year-old woman with no past medical history or family history of interest. She was referred to the dermatology department for pruritic lesions that had developed 2 months earlier in the genital region. She did not report any contact allergies or at-risk sexual activities. Physical examination revealed multiple, shiny whitish papules of 2 to 3mm in diameter in a cobblestone pattern on the medial aspect of the thigh, on the labia majora, on the perineum, and in the perianal region (Fig. 1). There were no similar lesions on other areas of the skin or mucosas and no nail changes. Laboratory tests (routine blood tests; serology for hepatitis B and C viruses, human immunodeficiency virus, and antinuclear, antibasement membrane, and antidesmoglein 1 and 3 antibodies; and cultures for bacteria and fungi) were normal or negative. Biopsy findings included mild epidermal hyperplasia with hyperkeratosis, parakeratosis, acanthosis, focal acantholysis with suprabasal clefts (Fig. 2), and dyskeratosis with corps ronds and grains (Fig. 3); a mild perivascular mononuclear inflammatory infiltrate was present in the papillary dermis. Direct immunofluorescence with immunoglobulin (Ig) M, IgG, IgA, complement components C3 and C1q, and fibrinogen antisera was negative. With a diagnosis of PAD of the genitocrural region, treatment was started with topical clobetasol, which produced an improvement in the pruritus, though the lesions persisted.
The main differential diagnosis of PAD is with Hailey-Hailey disease and Darier disease, which are hereditary genodermatoses in which loss of function mutations of the ATP2C1 and ATP2A2 calcium pump genes, respectively, have been reported in peripheral blood DNA samples. Darier disease, with very similar histopathological findings to those observed in our patient, usually develops in adolescence and is characterized by verrucous papules and plaques in seborrheic regions, with punctate palmoplantar keratoderma, verrucous papules on the dorsum of the hands and the feet, and characteristic nail changes. Hailey-Hailey disease can also show histological similarities with reported cases of PAD but, in contrast to Darier disease, there is a predominance of acantholysis and the dyskeratosis is very mild or absent; the disease typically presents in young adults, with painful erosions in the skin folds. Transient acantholytic dermatosis (Grover disease) should also be included in the differential diagnosis because of its histopathological similarities with PAD, although it typically presents in adults as transient confluent pruritic papules on the trunk.
The individual responses of patients with PAD to treatment with corticosteroids, topical retinoids, cryotherapy, electrocoagulation, or surgery have been reported as variable.6 In a recent study, laser therapy achieved lasting symptomatic improvement.7
The issues we have discussed regarding the classification of PAD as a separate entity from Darier or Hailey-Hailey disease arise because there have been reports of cases of Darier and Hailey-Hailey disease localized to the genitocrural region that have been histologically similar to PAD.8,9 The fact that Hailey-Hailey disease can show a variable degree of penetration and can present at different ages leads to even greater confusion. Two recent publications have reported a mutation in ATP2C1 in 3 cases of PAD of the genitocrural area, suggesting that at least some cases of PAD could be localized variants of Hailey-Hailey disease.4,10 It was not possible to perform a genetic study in our patient.
In conclusion, we believe that PAD has not yet been fully defined, and that its final characterization will require genetic study to exclude localized Darier or Hailey-Hailey disease, as there may be clinical and histopathological overlap.
Please cite this article as: Montis-Palos MC, et al. Dermatosis acantolítica papular del área genitocrural: ¿forma localizada de Darier o Hailey-Hailey? Actas Dermosifiliogr. 2013;104:170–2.