The patient was 50-year-old woman with a history of hysterectomy for uterine leiomyomas (1997), collecting duct carcinoma treated by radical right nephrectomy (2005), and mucinous cystadenoma of the left ovary for which adnexectomy (2010) was performed. The most notable aspect of her family history was that her brother and sister had died of renal carcinoma.
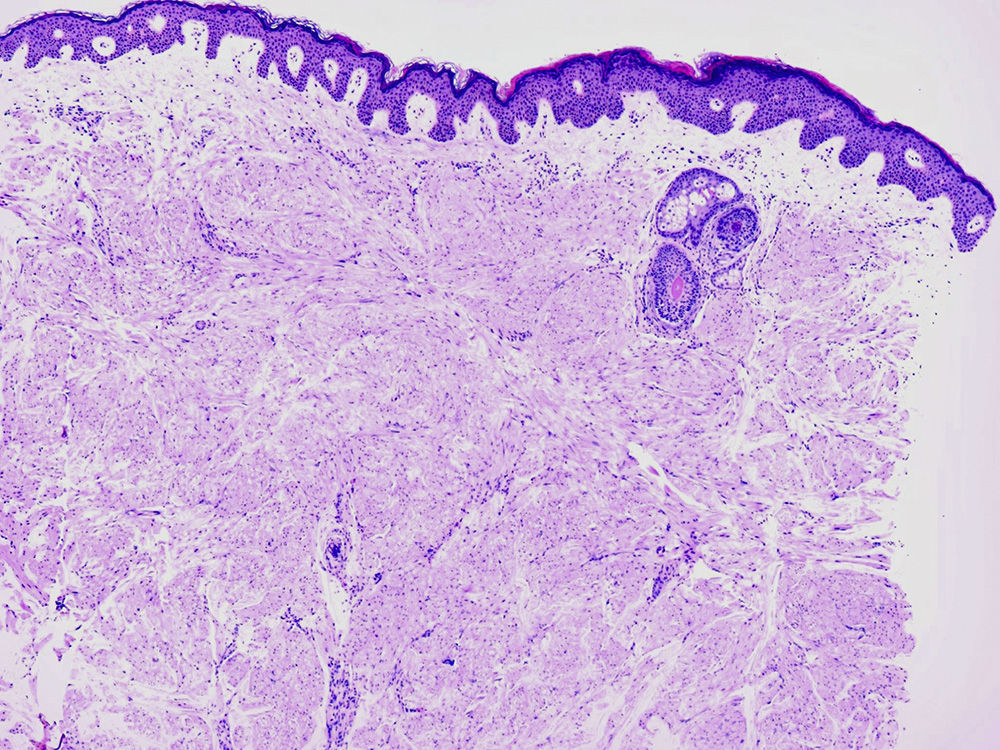
She consulted a dermatologist for multiple skin lesions on the trunk and proximal limbs, which had developed progressively after the diagnosis of renal cancer; the lesions were painful when touched or exposed to low temperatures (Fig. 1).
Physical ExaminationPhysical examination revealed some 15 to 20 erythematous nodular lesions located primarily on the trunk and proximal limbs.
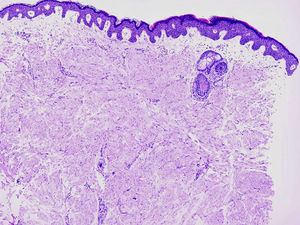
HistologyThe results of histological examination revealed unencapsulated tumoral lesions located in the dermis and composed of interlacing bundles of smooth muscle fibers. The cells had abundant eosinophilic cytoplasm and elongated nuclei with blunt ends (Fig. 2).
What Is Your Diagnosis?
DiagnosisHereditary leiomyomatosis and renal cell cancer (HLRCC).
Clinical CourseAfter years of monitoring, the renal cancer has shown no signs of local recurrence or distant metastasis. The skin lesions have continued to grow in both number and size over the years. The patient and her family were referred for genetic testing.
TreatmentThe most painful skin lesions were excised surgically.
CommentHLRCC is a rare disorder characterized by the presence of cutaneous and uterine leiomyomas in association with renal cell cancer.1 The renal cancer is typically unilateral (unlike other hereditary renal cancer syndromes such as Von Hippel Lindau or Birt-Hogg-Dubé) and tends to be particularly aggressive. The histological classification is usually type 2 papillary carcinoma, although cases have been reported of collecting duct carcinomas and tumors comprising clear cells, mixed clear and papillary cells, or tubular-papillary cells. It is rare for cutaneous piloleiomyomas or uterine leiomyomas to degenerate to malignant forms, although some cases have been reported and it has been observed that malignant transformation tends to occur at younger ages.1 Moreover, an association has been described between the mutation of the gene responsible and other malignancies, including breast, prostate, and hematologic cancers.
HLRCC should not be confused with Reed syndrome, a condition in which cutaneous and uterine leiomyomas are associated, but which does not involve kidney cancer.2
The 1q42.3-q43 gene has been has been implicated in the etiology of HLRCC. This gene has an autosomal dominant mode of inheritance and encodes fumarate hydratase, a Krebs cycle enzyme involved in the tumor suppressor system. In HLRCC, a mutation in 1q42.3-q43 leads to an accumulation of fumarate, which inhibits the activity of the enzyme that hydrolyzes hypoxia inducible factor (HIF), thereby raising HIF levels and, consequently, the transcription of genes relevant to carcinogenesis.3,4
The choice and prescription of the most appropriate treatment for cutaneous piloleiomyomas will always depend on the number, size, and location of the lesions and the symptoms reported.5 When a patient presents a large number of lesions only those producing the most discomfort should be treated and disfiguring surgical excision of large piloleiomyomas should be avoided. However, in the case of a patient with an isolated lesion or very few piloleiomyomas we would opt for surgical excision.
In this case, in view of the number, size, and location of the piloleiomyomas, we decided that surgical excision was most appropriate measure.
Awareness of the syndrome on the part of the dermatologist will facilitate early diagnosis, and diagnosis should be confirmed by genetic testing of both the patient and his or her family. This will also serve to reduce morbidity and mortality in affected individuals.6
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Millán-Cayetano JF, Segura-Palacios JM, de Troya-Martín M. Nódulos cutáneos dolorosos. Actas Dermosifiliogr. 2015;106:423–424.