The patient was a 47-year-old man with a history of prostate cancer diagnosed 5 years earlier with bone metastases in the right acetabulum (stage pT4N1M1). The patient had undergone a radical cystoprostatectomy with a Bricker-type ureteroileostomy. He received hormone therapy with luteinizing hormone-releasing hormone (LHRH) agonists and antiandrogens in addition to external beam radiation therapy. The patient reported the gradual development of pruritic lesions in the area around the stoma over the previous 6 months.
Physical ExaminationPhysical examination revealed multiple hard grayish-white domed papules 2 to 10mm in diameter that coalesced to form a peristomal pseudoverrucous mass (Fig. 1). The lesions were pruritic but not painful. The patient had no palpable lymph nodes in the groin area or any other site.
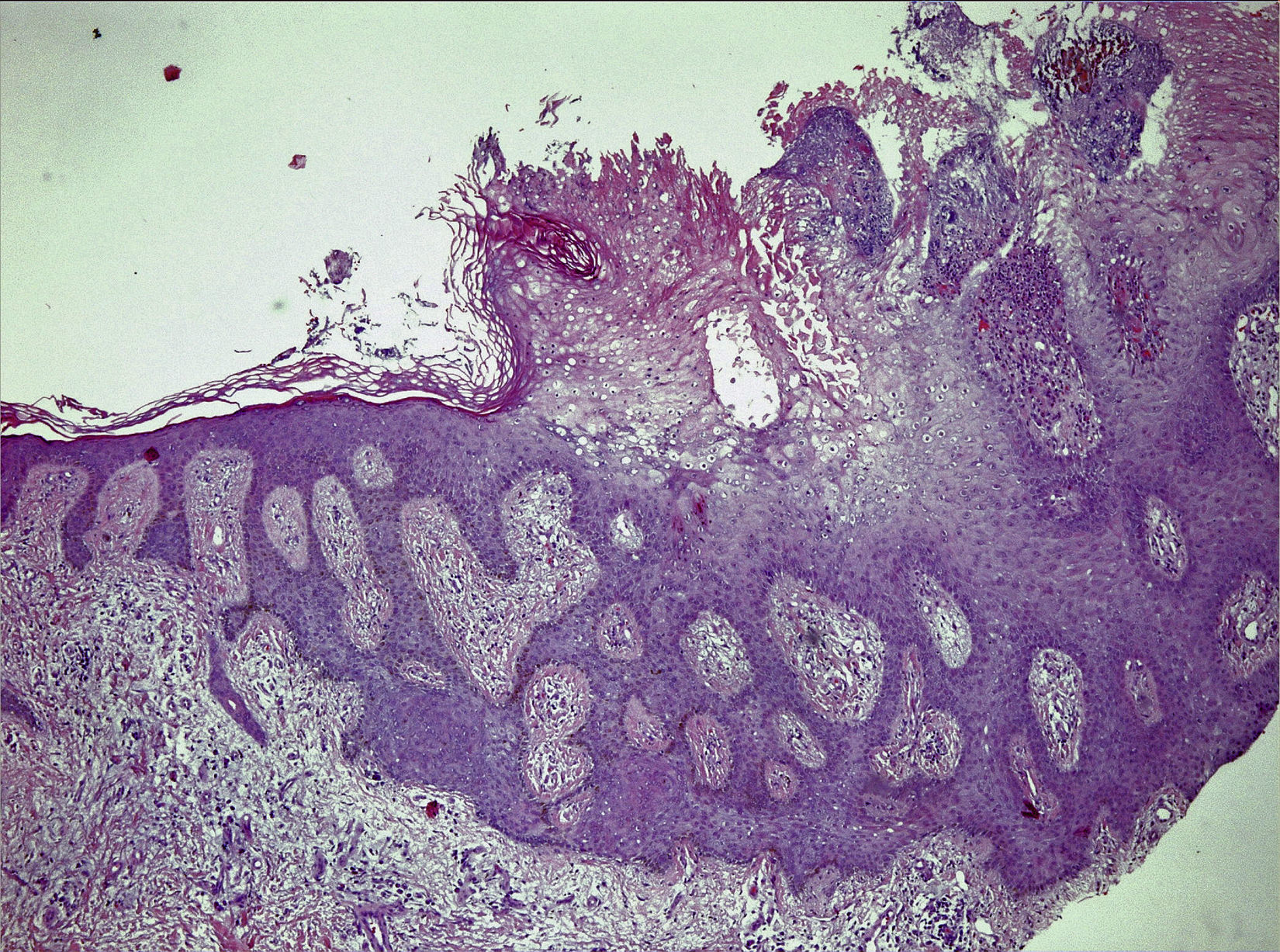
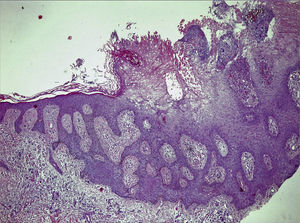
HistopathologyA skin biopsy was performed and histologic examination revealed pseudoepitheliomatous epithelial hyperplasia and chronic inflammatory infiltrate with no koilocytes, atypia, or mitotic figures (Fig. 2).
Additional TestsProteus vulgaris was isolated from urine culture.
What Is Your Diagnosis?
DiagnosisPseudoverrucous papules and nodules (PPN) or chronic papillomatous dermatitis.
Clinical Course and TreatmentTreatment was started with amoxicillin–clavulanic acid (875 and 125mg, respectively, every 8hours for 10 days); by the end of the treatment the lesions had improved slightly. The patient was also advised to adjust the drainage device and change the collection pouch and topical olive oil frequently. After 3 months, the lesions had virtually disappeared.
CommentPPN, or chronic papillomatous dermatitis, is a rare complication found mainly on the skin around stomas and the perianal area.1 Peristomal PPN is considered to be a special form of irritant contact dermatitis caused by the chronic local action of alkaline urine. Urine can accumulate on the skin surface if the ostomy pouch is not properly adjusted, favoring bacterial overgrowth. The bacteria degrade urea, causing an increase in urinary pH.2 PPN is clinically characterized by multiple erythematous-brownish or grayish-white papules and nodules generally located on the lower side of the stoma. The lesions can appear on peristomal skin and also in the perianal area as a result of severe intractable diarrhea of any cause.1–4 PPN has also been reported in patients with Hirschsprung disease who have undergone colonic re-anastomosis and in children and adults with urinary incontinence.5,6 Diagnosis is established clinically and histologically. Differential diagnosis includes the main dermatoses located around stoma sites (secondary neoplasms, metastases, incrustations, exuberant granulation tissue, human papillomavirus infection, gangrenous pyoderma, pressure ulcers, mucosal transplant).1 To prevent PPN, it is important to adjust the drainage device properly and change the collection pouch frequently. PPN is easy to treat, but without treatment complications such as bleeding, stenosis, and stoma occlusion may develop. The recommended treatment for urostomy-related PPN is urine acidification (cranberry juice and a vitamin C–rich diet or vitamin C supplements) and early treatment of infections.1,4 Few cases have been reported recently.3,4 We describe a new case that responded well to treatment, with the aim of reminding dermatologists of the existence of this probably underdiagnosed condition.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Latour-Álvarez I, García-Peris E, Pestana-Eliche MM, García-Bustínduy M. Lesiones nodulares periestomales. Actas Dermosifiliogr. 2017;108:363–364.