Classic or idiopathic Sweet syndrome is a neutrophilic skin disorder characterized by the association of cutaneous manifestations and systemic symptoms. The skin lesions tend to occur on the face, neck, chest, and arms, and present as painful papules, nodules, or erythematous plaques. Systemic symptoms, such as general malaise, joint pain, and neutrophilic leukocytosis, may appear days earlier or at the same time as the dermatosis. Classic or idiopathic Sweet syndrome has been linked to digestive and upper airway infections, inflammatory bowel disease, and pregnancy. More rarely, it is induced by drugs (most often granulocyte-colony stimulating factor) or associated with a malignant disease (most commonly hematologic malignancies).1 The atypical variant that arises on lymphedema is considered to be a less severe form.
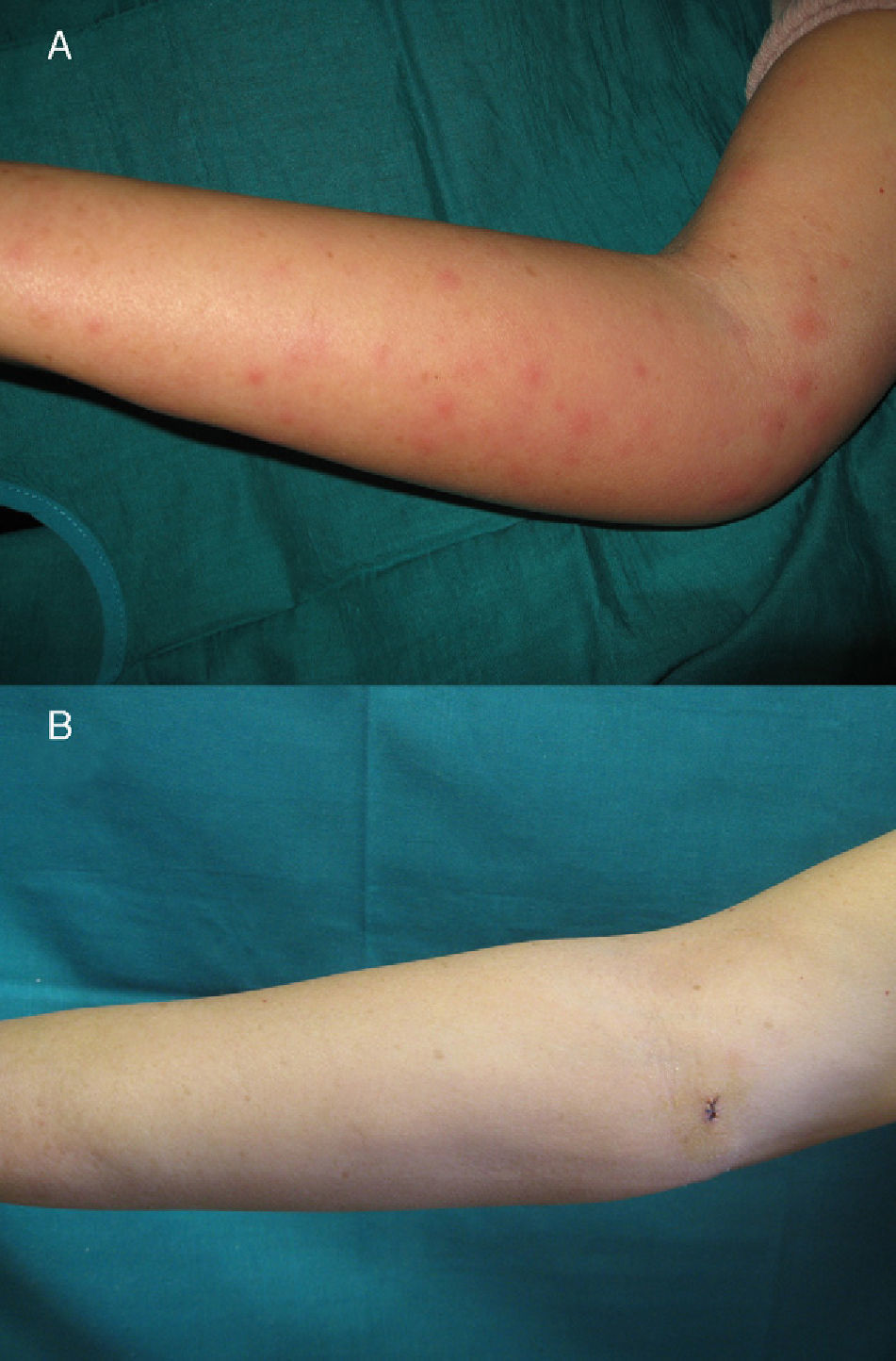
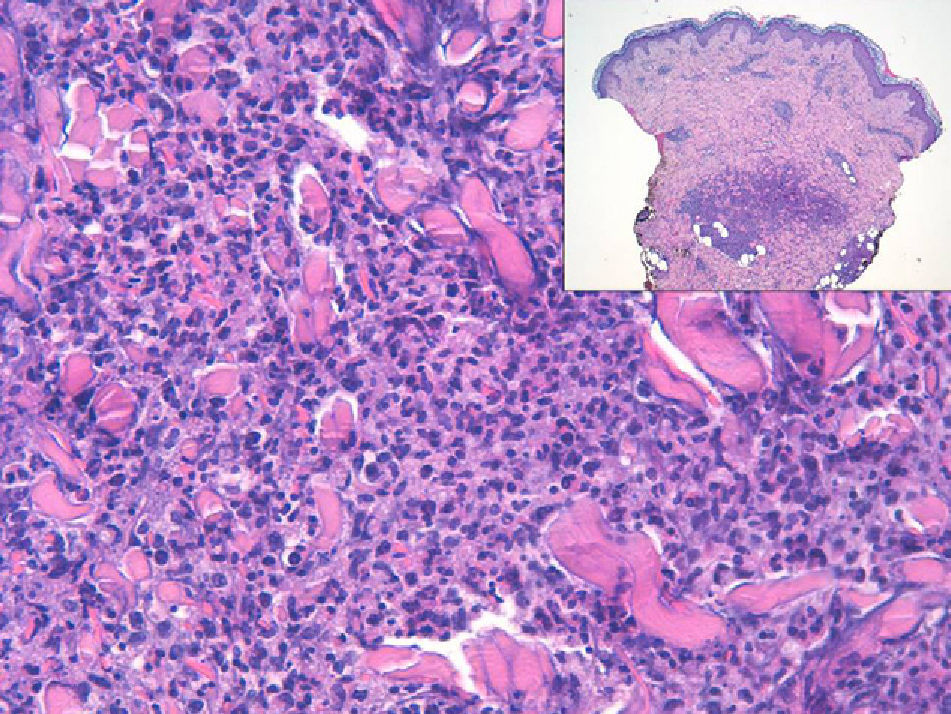
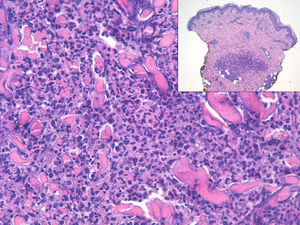
Our patient was a 60-year-old woman who had been diagnosed 6 years previously with invasive ductal carcinoma of the right breast. She underwent conservative surgery with axillary dissection and received radiation therapy and chemotherapy as adjuvant treatment. At the time of consultation, the patient was receiving treatment with capecitabine for liver metastases. Two days earlier, she had developed multiple erythematous maculopapular lesions on the inner aspect of the right upper arm and forearm; the entire arm was edematous and the lesions were very painful to the touch (Fig. 1A). Some days before the onset of the cutaneous symptoms, the patient had experienced general malaise, a sensation of poor temperature regulation, and shivers. The only blood test results of interest were elevated C-reactive protein levels (99.6mg/L), and no abnormalities were found in the complete blood count (leukocytes, 7590/mm3 [neutrophils, 69.9%]). A skin biopsy revealed a dense, neutrophilic inflammatory infiltrate in the dermis, which was predominantly perivascular and interstitial; the epidermis was normal (Fig. 2). After treatment with amoxicillin–clavulanic acid was initiated, the skin lesions resolved completely in less than a week (Fig. 1B).
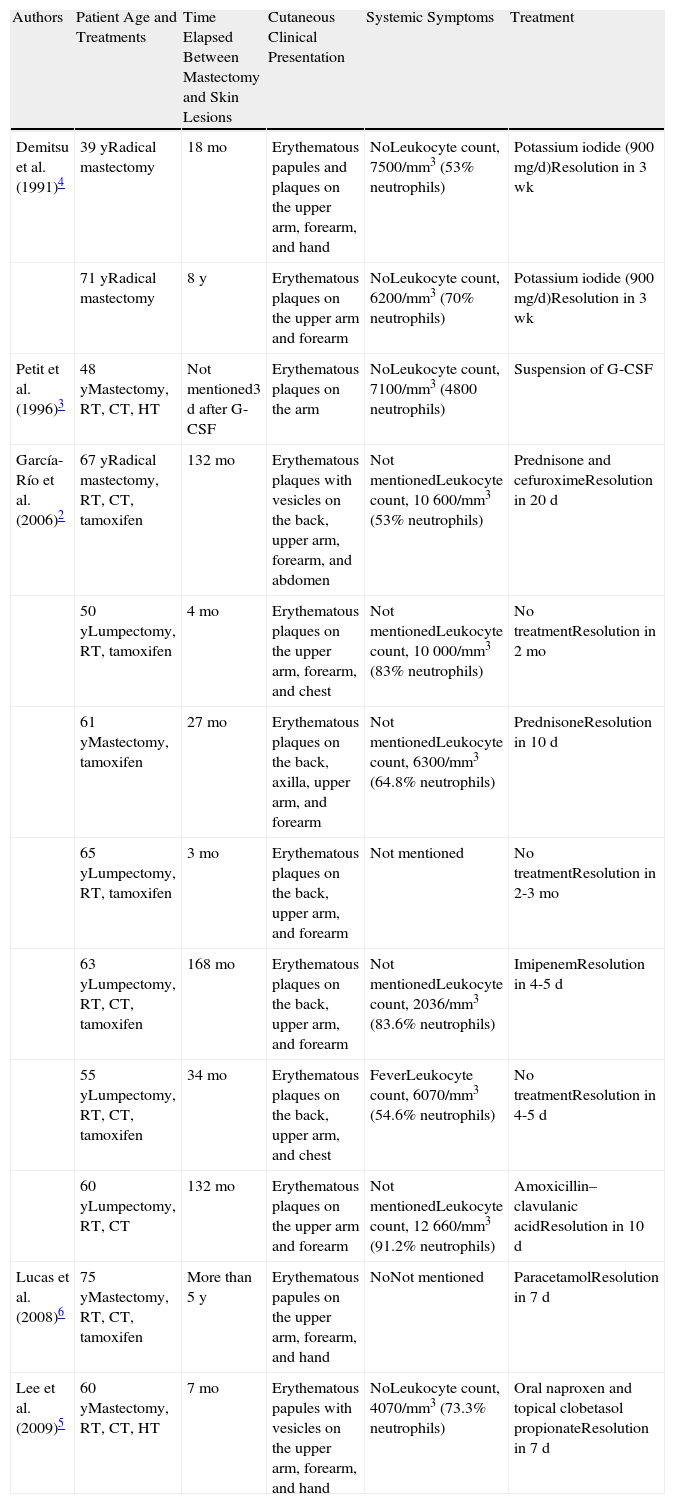
Neutrophilic dermatosis on the site of postmastectomy lymphedema is considered to be an atypical or localized variant of classic or idiopathic Sweet syndrome and only 12 cases have been reported to date (Table 1). The disorder has been reported in women aged between 39 and 75 years who have undergone surgery for breast cancer, axillary dissection, and other adjuvant treatments (radiation therapy, hormone therapy, and chemotherapy), and who have developed lymphedema in the ipsilateral arm as a result of those treatments. The interval between breast surgery and appearance of the Sweet skin lesions ranges from a few months to a number of years. Clinically, the disease manifests as multiple painful erythematous papules, which may coalesce to form plaques. The lesions appear on the edematous area, which in most cases comprises the upper arm, forearm, and dorsum of the hand. Less often, the lesions take the form of vesicles or blisters; hemorrhagic blisters or pustules have not been reported. The condition has not been linked to local relapse or distant metastases of the breast cancer, except in 1 case where it was described in association with skin metastases2; only 1 case has been reported in a patients receiving granulocyte-colony stimulating factor.2,3 Compared to classic Sweet syndrome, the systemic symptoms are mild (in some cases absent), neutrophilic leukocytosis is less common, and relapses are less prevalent. The other distinctive difference is that the lesions are restricted to the site of the lymphedema. Treatment with antibiotics appears to cure the lesions more rapidly than treatment with systemic corticosteroids or potassium iodide,4 and the disorder also responds well to oral anti-inflammatory drugs and high-potency topical corticosteroids.2–6
Reported Cases of Sweet Syndrome Located on the Site of Postmastectomy Lymphedema.
| Authors | Patient Age and Treatments | Time Elapsed Between Mastectomy and Skin Lesions | Cutaneous Clinical Presentation | Systemic Symptoms | Treatment |
| Demitsu et al. (1991)4 | 39 yRadical mastectomy | 18 mo | Erythematous papules and plaques on the upper arm, forearm, and hand | NoLeukocyte count, 7500/mm3 (53% neutrophils) | Potassium iodide (900mg/d)Resolution in 3 wk |
| 71 yRadical mastectomy | 8 y | Erythematous plaques on the upper arm and forearm | NoLeukocyte count, 6200/mm3 (70% neutrophils) | Potassium iodide (900mg/d)Resolution in 3 wk | |
| Petit et al. (1996)3 | 48 yMastectomy, RT, CT, HT | Not mentioned3 d after G-CSF | Erythematous plaques on the arm | NoLeukocyte count, 7100/mm3 (4800 neutrophils) | Suspension of G-CSF |
| García-Río et al. (2006)2 | 67 yRadical mastectomy, RT, CT, tamoxifen | 132 mo | Erythematous plaques with vesicles on the back, upper arm, forearm, and abdomen | Not mentionedLeukocyte count, 10 600/mm3 (53% neutrophils) | Prednisone and cefuroximeResolution in 20 d |
| 50 yLumpectomy, RT, tamoxifen | 4 mo | Erythematous plaques on the upper arm, forearm, and chest | Not mentionedLeukocyte count, 10 000/mm3 (83% neutrophils) | No treatmentResolution in 2 mo | |
| 61 yMastectomy, tamoxifen | 27 mo | Erythematous plaques on the back, axilla, upper arm, and forearm | Not mentionedLeukocyte count, 6300/mm3 (64.8% neutrophils) | PrednisoneResolution in 10 d | |
| 65 yLumpectomy, RT, tamoxifen | 3 mo | Erythematous plaques on the back, upper arm, and forearm | Not mentioned | No treatmentResolution in 2-3 mo | |
| 63 yLumpectomy, RT, CT, tamoxifen | 168 mo | Erythematous plaques on the back, upper arm, and forearm | Not mentionedLeukocyte count, 2036/mm3 (83.6% neutrophils) | ImipenemResolution in 4-5 d | |
| 55 yLumpectomy, RT, CT, tamoxifen | 34 mo | Erythematous plaques on the back, upper arm, and chest | FeverLeukocyte count, 6070/mm3 (54.6% neutrophils) | No treatmentResolution in 4-5 d | |
| 60 yLumpectomy, RT, CT | 132 mo | Erythematous plaques on the upper arm and forearm | Not mentionedLeukocyte count, 12 660/mm3 (91.2% neutrophils) | Amoxicillin–clavulanic acidResolution in 10 d | |
| Lucas et al. (2008)6 | 75 yMastectomy, RT, CT, tamoxifen | More than 5 y | Erythematous papules on the upper arm, forearm, and hand | NoNot mentioned | ParacetamolResolution in 7 d |
| Lee et al. (2009)5 | 60 yMastectomy, RT, CT, HT | 7 mo | Erythematous papules with vesicles on the upper arm, forearm, and hand | NoLeukocyte count, 4070/mm3 (73.3% neutrophils) | Oral naproxen and topical clobetasol propionateResolution in 7 d |
Abbreviations: CT indicates chemotherapy; G-CSF, granulocyte-colony stimulating factor; HT, hormone therapy; RT, Radiation Therapy.
The pathophysiology of this condition is not understood and a number of theories have been put forward, all of which posit a local disruption in cell trafficking due to inadequate lymphatic drainage caused by the lymphadenectomy and the radiation therapy. The hypothesis is that cytokines accumulate at the site of the lymphadenectomy attracting neutrophils to an area with reduced immunocompetence and thereby favoring local development of malignancies, infections, and immune disorders such as neutrophilic dermatosis.2,7
The differential diagnosis should include infections such as cellulitis, erysipelas, folliculitis, and herpes zoster, as well as thrombophlebitis and recall phenomenon. Histology should rule out chronic radiodermatitis, carcinoma erysipeloides, and contact dermatitis. The clinical course, biopsy findings, and additional tests will all help to establish the definitive diagnosis.2,6
In conclusion, we report a new case of neutrophilic dermatosis on the site of a lymphedema. This condition is a localized variant of classic Sweet syndrome with differences that include not only the location of the lesions but also a milder course with fewer systemic symptoms, fewer relapses, and a good response to oral antibiotics, anti-inflammatory drugs, and topical corticosteroids. Despite the large number of cases of breast cancer and of lymphedema arising as a complication of the different treatments used in these patients, few cases of neutrophilic dermatosis have been documented. This is probably due to confusion with other inflammatory or infectious diseases that are more common in this group of patients.2
Please cite this article as: Gutiérrez-Paredes E, González-Rodríguez A, Molina-Gallardo I, Jordá-Cuevas E. Dermatitis neutrofílica sobre área de linfedema posmastectomía. Actas Dermosifiliogr.2012;103:649-651.