Leprosy, a disease caused by Mycobacterium leprae, primarily affects the skin and nerves, but the nails are also involved in as many as 3 out of 4 patients. The factors that trigger nail changes in leprosy are numerous and include repeated trauma, neuropathy, vascular impairment, infections, lepra reactions, and the drugs used to manage the disease. The changes most often reported include subungual hematomas, onycholysis, onychauxis, onychogryphosis, pterygium unguis, and onychoheterotopia, most of which can be attributed to nerve damage and trauma. Furthermore, the acro-osteolysis that occurs in the advanced stages of the disease may present with brachyonychia, racquet nails, or even anonychia. Infections of the nail bed leading to paronychia and onychomycosis should also be taken into account in leprosy. Other typical changes include longitudinal striae, pitting, macrolunula, Terry nails, leukonychia, hapalonychia, and Beau lines. In this review, we describe the principal nail changes associated with leprosy. These changes, which are highly varied and diverse in origin, are in fact a reflection of the significant morbidity caused by M leprae infection.
La lepra es una enfermedad causada por Mycobacterium leprae. Afecta principalmente a los nervios y a la piel, y hasta en tres de cada cuatro pacientes también a las uñas. Las causas desencadenantes de las lesiones ungueales en la lepra son múltiples, y de ellas destacan los traumatismos repetidos, la neuropatía, la insuficiencia vascular, las infecciones, las leprorreacciones o los fármacos utilizados en el tratamiento. Entre los cambios más destacados se encuentran los hematomas subungueales, la onicolisis, la onicauxis, la onicogrifosis, el pterigium unguis dorsal o la onicoheterotopia, y en su mayoría pueden atribuirse al daño nervioso y a los traumatismos. Por otro lado, la acrosteolisis que se produce en estadios avanzados puede cursar con braquioniquia, uñas en raqueta o incluso llegar a la anoniquia. Las infecciones de las uñas, con la aparición de paroniquia y onicomicosis, constituyen otro de los capítulos a tener en cuenta en la lepra. Además hay otras alteraciones caracterísiticas como las estrías longitudinales, los pits, la macrolúnula, las uñas de Terry, la leuconiquia, la hapaloniquia o las líneas de Beau. A lo largo de esta revisión se describen los principales cambios que se producen en las uñas por esta enfermedad, que son muy variados y de origen muy diverso, y de hecho son el reflejo de la amplia morbilidad que causa la infección por M. leprae.
Leprosy, a disease known since antiquity and about which many notions have formed over the course of history, is caused by Mycobacterium leprae. Although not fatal, this infection significantly limits the physical, psychological, and social well-being of patients1 and while its prevalence is now extremely low in many parts of the world it remains a major public health problem in certain areas.2 We have known how to treat this disease since the end of the 1970s, yet full understanding did not come until the introduction of shorter duration multidrug therapy at established doses in 1982.3 With wide application of multidrug therapy and early diagnosis of leprosy, the prevalence of the disease has decreased worldwide and functional morbidity and mortality have diminished.2–6
M leprae infection mainly affects nerves and skin, but additional damage arises as other organs and structures (eyes, mouth, joints and more) become involved.4 Functional limitations and partial or full disability can develop, with dire consequences on the patient's quality of life.
The number of new cases of leprosy around the world fell from 620 000 in 2002 to 250 000 in 2009, according to the World Health Organization. Most new cases occur in India, Indonesia, Brazil, Nepal, Bangladesh, and certain African countries, such as Nigeria, Angola, and Ethiopia.2 In recent decades, fewer cases have emerged in the local population in Spain, but we are now diagnosing leprosy more often in immigrants as a result of global migration from regions where the disease is more prevalent.7,8 Furthermore, a fair number of young Spanish doctors are now traveling to work with organizations providing medical care in low-income countries, where they see patients with leprosy.9,10 This disease has been discussed in a few review articles in the recent Spanish medical literature,11–14 but as far as we can tell the effects of leprosy on the nails have not been addressed. Therefore, based on our experience treating patients with leprosy in Ethiopia,15,16 we aim to review the effects of this disease on the nails for the benefit of interested clinicians.
The Nails: Development and AnatomyNails are cutaneous adnexal structures that protect the tips of fingers and add a degree of precision that improves our ability to pick up objects and perform other delicate maneuvers.17–19 These structures are derived from the primitive epidermis, as are hair and the stratum corneum.17 The nail unit consists of the plate, matrix, bed, and proximal and lateral folds. The outer layer is the plate, which covers the matrix and the bed.19 The nail matrix is divided into the dorsal, middle, and ventral portions. The dorsal portion of the matrix forms the outer layers the nail plate, the middle of the matrix gives rise to the deeper layers of the plate, and the ventral matrix contributes to the formation of the nail bed. The proximal fold is the continuation of the skin of the finger, which folds back upon itself at the dorsal part of the matrix. The hyponychium, located just under the free margin of the nail plate, represents the transition from the epithelium of the nail bed.20
Causes of Nail Damage in LeprosyNail changes may derive from diseases specific to the unit itself or may be part of the general clinical picture of a skin disease. In addition, nail changes may occur during the course of a variety of systemic diseases, and most such changes are nonspecific.17–19
Examination of the nails is usually of great help in the clinical diagnosis of certain systemic diseases, such as dermatomyositis. Nail changes that occur in both the early and late (mutilating) stages of leprosy can affect the plate, the matrix, the bed, and the folds. Observation of these changes can aid diagnosis and help in the evaluation of the repercussions of leprosy on the patient's physical, psychological, and social well-being.
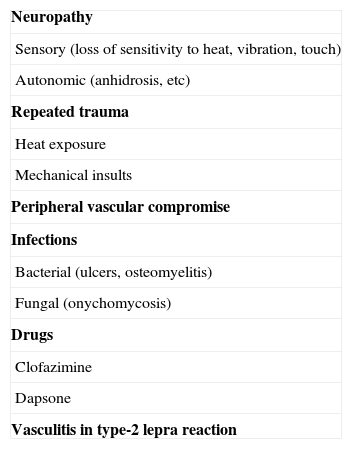
As many as 3 out of 4 patients with leprosy have nail involvement. The associated factors are many and include repeated trauma, neuropathy, vascular impairment, infections, or adverse effects of drugs used in treatment.17,21–23 The causes of leprous nail damage are summarized in Table 1. The main factor is neuropathy, which in addition exacerbates the negative effects of all the others.21–23 Therefore, peripheral neuropathy in leprosy might be assumed to lead to changes of the type seen in diabetic neuropathy, but this is not the case; nail problems in leprosy patients have been seen to be more common and more severe than in patients with diabetes.22
Main Causes of Nail Changes in Leprosy.
| Neuropathy |
| Sensory (loss of sensitivity to heat, vibration, touch) |
| Autonomic (anhidrosis, etc) |
| Repeated trauma |
| Heat exposure |
| Mechanical insults |
| Peripheral vascular compromise |
| Infections |
| Bacterial (ulcers, osteomyelitis) |
| Fungal (onychomycosis) |
| Drugs |
| Clofazimine |
| Dapsone |
| Vasculitis in type-2 lepra reaction |
Nerve damage leads to loss of sensation and deformities in fingers and toes; autonomic dysfunction also develops, leading to anhidrosis and dry skin and fissures that affect the hands and feet in particular. With the numbness at the distal ends of deformed fingers and toes, any slight mechanical trauma or exposure to heat will predispose the patient to further injury, particularly if the insult is often repeated. Infections will then develop, leading to lysis of the phalangeal bone, thinning and finally loss of the tips of fingers and toes along with their nails.5,6,24 Nail changes support the hypothesis of Baran and Juhlin25 that nail development is tied to that of the underlying bone; thus, anonychia and hyponychia occur when the bone is hypoplastic or absent. In fact, nail abnormalities in leprosy are usually secondary to distal resorption of the phalanges.21
The nails are also affected by the vasculitis caused by a type-2 lepra reaction (erythema nodosum leprosum). In this condition a humoral immune response leads to the production of circulating immune complexes.12 The clinical picture includes subcutaneous nodules with erythema, nerve damage, and multiorgan involvement. Iridocyclitis, orchiepididymitis, and other systemic manifestations, such as fever, arthritis, lymphadenitis, neuritis, or nephritis, may also develop.26,27 This reaction compromises peripheral vessels, triggering loss of distal tissues, including the nails.28 A type-2 lepra reaction may present before leprosy is diagnosed or it might develop during treatment or in final phases.5,26
Drugs used to treat leprosy (eg, clofazimine or dapsone) have also been implicated in certain nail changes, such as Beau lines and subungual hyperkeratosis,21–23 as will be discussed below.
Nail Changes According to Leprosy Classification SystemsThe 1962 classification system of Ridley and Jopling29 described 5 types of leprosy: tuberculoid, borderline tuberculoid, borderline-borderline, borderline lepromatous, and lepromatous. Nail abnormalities are more common in the lepromatous form than in the tuberculoid form. Patients whose disease has progressed over many years even after it was first recognized, and those with neuropathic and nutritionally related changes in hands and feet, will also have more nail abnormalities. The causes of nail disorders in tuberculoid and lepromatous forms of the disease are similar.21–23 However, in lepromatous leprosy, nail abnormalities may be associated with granulomatous infiltration of the distal phalanges and with vascular impairment resulting from a type-2 lepra reaction.21,22
The effect of the 2 forms of leprosy on the nails differs most clearly in the pattern of onset of changes and in the symmetry of their distribution.17,21,22 Nail changes come late to patients with lepromatous leprosy and damage is bilateral and symmetric. In patients with the tuberculoid form, however, nail abnormalities are seen in the early phases of the disease and are unilateral and asymmetric.
In practice, patients are usually classified according to bacterial load as recommended by the World Health Organization.30 In the paucibacillary form, up to 5 cutaneous lesions are present, only a single nerve trunk is involved, and bacilloscopy is negative. In the multibacillary form, more than 5 lesions are present, more than 1 nerve trunk is compromised, or bacilloscopy is positive. Nail lesions are more common in the multibacillary form21 because neuropathy, trauma, infections, and vascular compromise mediated by immune complexes are all more severe.4,13,14
Prevalence of Nail Changes in LeprosyFew studies have investigated the prevalence of nail changes in patients with leprosy. The first was the 1991 study of Patki and Baran21 in India. They found nail abnormalities in 64% of 357 patients. Kaur and coworkers22 later (2003) published a study of 300 Indian patients with leprosy, reporting an overall prevalence of 77.3% for nail changes. The rates were 56% for the paucibacillary form and 87.3% for the multibacillary type. Among long-time residents of a leper colony the rate was 96%. More recently, El Darouti and coworkers23 found nail changes in 86% of 115 patients with both forms of leprosy in Turkey.
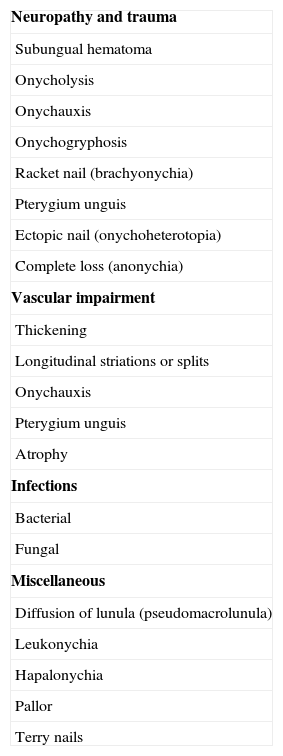
Nail Changes in LeprosyAlthough the nail changes observed in leprosy are highly characteristic, they are not specific to the disease but, as mentioned above, are found in other conditions that involve peripheral neuropathy, such as diabetes mellitus.31 In leprosy, the nail plate, the matrix, and the bed can be involved, as well as the periungual skin folds. The possible changes are many, affecting the shape, size, thickness, surface, consistency, and the color of the nail and bed or the nail tissues overall. Table 2 gives a classification of nail changes based on the one proposed by Patki and Baran4 for this disease.
Classification of Nail Damage in Leprosy.
| Neuropathy and trauma |
| Subungual hematoma |
| Onycholysis |
| Onychauxis |
| Onychogryphosis |
| Racket nail (brachyonychia) |
| Pterygium unguis |
| Ectopic nail (onychoheterotopia) |
| Complete loss (anonychia) |
| Vascular impairment |
| Thickening |
| Longitudinal striations or splits |
| Onychauxis |
| Pterygium unguis |
| Atrophy |
| Infections |
| Bacterial |
| Fungal |
| Miscellaneous |
| Diffusion of lunula (pseudomacrolunula) |
| Leukonychia |
| Hapalonychia |
| Pallor |
| Terry nails |
Adapted from Patki and Baran21
Traumatic insults that are not perceived by the patient or that are repeated can injure the nail, sometimes significantly. The main nail changes that arise from trauma and neuropathy are described in this section, although the reader must remember that other conditions can also cause the same signs.
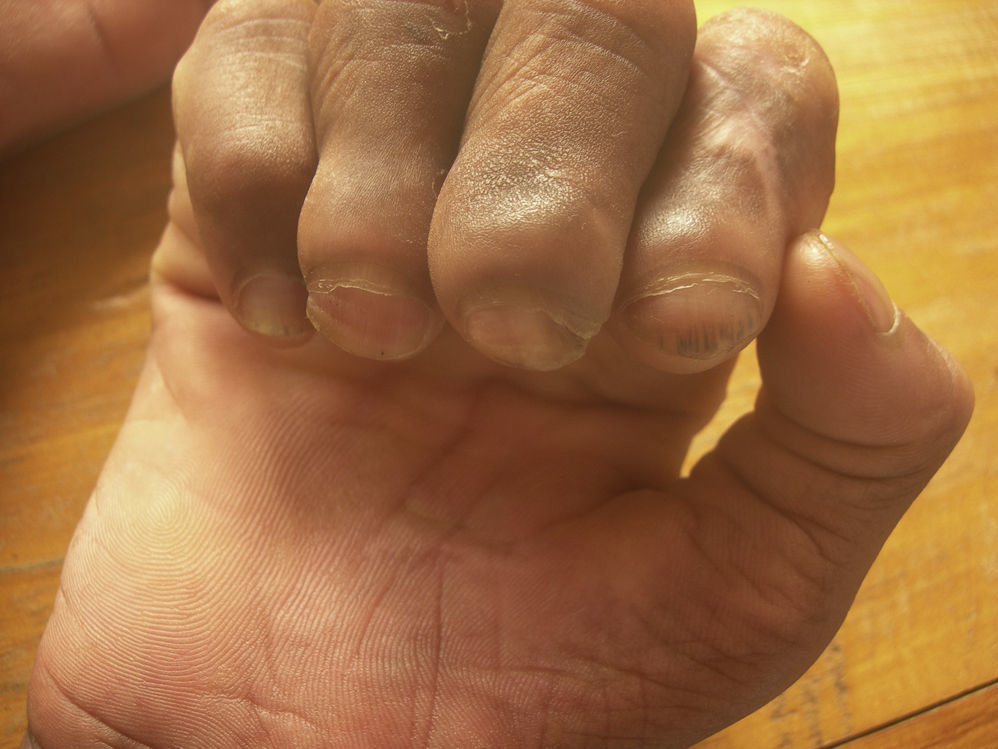
Subungual HematomaA subungual hematoma (Fig. 1) can be seen through the nail plate as a bluish gray or even black area and is the result of mechanical trauma that usually goes unnoticed by these patients. Such bruising may be an early sign, one that is usually followed by loss of a part of the nail or even the entire plate. A subungual hematoma should be distinguished from other lesions of similar appearance, such as nevi or subungual melanoma, which may also be present in patients with leprosy. If necessary, dermatoscopy can be used to aid diagnosis.32
OnycholysisIn onycholysis, the nail plate detaches from the bed, leaving a subungual space where keratin and debris collect.19 This condition usually develops as a result of repeated trauma and often provides a point of entry for bacterial and fungal infections.33 Onycholysis is frequent in patients with leprosy.21–23
We should also mention that so-called green nail, denoting a greenish hue from the pyocyanin and pyoverdin synthesized by Pseudomonas aeruginosa organisms, is a condition that tends to develop in the presence of onycholysis when there is exposure to moist environments.34
OnychauxisOnychauxis refers to the thickening of nails that leads to a change in color, usually to a brownish tint,17 that is often a feature of the nail dystrophy in patients with leprosy.21,22
OnychogryphosisOnychogryphosis (Fig. 2) is the presence of a highly hypertrophic nail plate that becomes hornlike.17 This condition develops in response to many small insults to the nails of the type that can also lead to onychauxis. This condition is more common in toenails than fingernails, and it appears to be a result of faster growth of the nail matrix on one side than on the other.35
In a series of 20 patients recovering from leprosy in Japan, onychogryphosis was the most common nail abnormality.36 It is speculated that in patients under treatment for leprosy, clofazimine may be implicated in the development of this complication.37
Pterygium Unguis (Dorsal)Pterygium unguis (Fig. 3) involves the gradual invasion of the nail bed by the proximal fold and the cuticle until the cuticle, plate, and bed of the nail fuse.38 In leprosy this condition is related to traumatic insults and/or ischemia in a nail matrix that is poorly vascularized due to obliterating endarteritis and endarteritis resulting from a type-2 lepra reaction.39,40 Although not common, this nail complication is highly characteristic.21,22
Ectopic NailAn ectopic, or displaced, nail (Fig. 4) develops as a result of trauma causing a small part of the nail matrix to become detached. If such a separated portion is not destroyed, small nail spicules may grow.41 This event is rare41 but does occur in patients with leprosy, in whom it can be seen with certain frequency because of ongoing trauma that occurs particularly in the context of longstanding nerve damage.21,22
Acro-osteolysis and Nail LesionsAcro-osteolysis, referring to the distal resorption of phalangeal bone that is common in advanced stages of leprosy, arises as a consequence of neuropathic damage that leads to thickening of nerves and consequent sensory, motor, and vasomotor disorders.42,43 Repeated trauma, ischemia due to endarteritis and type-2 lepra reaction, diffuse osteoporosis related to testicular atrophy in leprosy, secondary infection that can lead to osteomyelitis, and bone damage caused by the granulomas specific to lepromatous leprosy also contribute to the development of acro-osteolysis.42,43 Early radiographic signs consist of transverse lytic bands in the distal phalanges; if the condition progresses, resorption progressively deforms the ends of fingers and toes, also leading to nail dystrophy.22
BrachyonychiaBrachyonychia and micronychia involve nail shortening as a result of acro-osteolysis and subsequent acronecrosis of finger pads.36
Pseudoclubbing, or Racket NailIf finger-pad necrosis progresses, the distal phalanx not only shortens but also widens. Pseudoclubbing or racket nail (Fig. 5) is the result of this process. Pseudoclubbing and brachyonychia are common in syndromes with brachydactyly, supporting the hypothesis of Baran and Juhlin25 that nail development is linked to that of the underlying bone.
AnonychiaComplete absence of the nail, or anonychia (Fig. 6), generally comes with disease progression and may be associated with complete loss of the distal phalanges. During the process, the nails become dry and dull and increasingly striated before disappearing altogether.44 All the nails are usually affected, and in this mutilating phase of the disease the hands, lacking nails and fingers, come to resemble fins (Fig. 7).
A perforating ulcer (Fig. 8) is one that is painless and tends to deepen.5 This lesion is associated with the sensory neuropathy that develops in patients with leprosy, and when an ulcer occurs at the tip of a finger or toe the nail is affected indirectly.
Nail Changes Secondary to InfectionsPatients with leprosy often develop infections at the distal end of extremities in the wake of injuries that are slight but that the patient fails to notice.
ParonychiaParonychia is an acute inflammation of periungual folds that commonly develops in response to direct or indirect injury to the area.45 Infection with Staphylococcus aureus and/or Streptococcus pyogenes then follows. Repeated bacterial infections destroy the nail matrix, leading to loss of the nail plate and, finally, scarring of the nail bed.
OnychomycosisOnychomycosis refers to the fungal infection of nails,46 which is observed in 20% to 30% of patients with leprosy according to Pardo-Castello and Pardo.47 The reported prevalence has been under 5% in more recent case series,21,22 but more cases would probably be diagnosed if more exhaustive studies were conducted on prospectively gathered data.48 The prevalence of onychomycosis is around 2% in the general population,48 indicating that this infection is more common among individuals with leprosy.46,49
A nail infection might be the result of the spread of a superficial fungal infection caused by such dermatophytes as Trichophyton rubrum, Trichophyton mentagrophytes, or Trichophyton tonsurans or by other fungi, such as Candida albicans.46,48,49
Other Nail AbnormalitiesLongitudinal Striations and MelanonychiaIn longitudinal melanonychia (Fig. 9), a pigmented band extends from the lunula to the free margin of the nail bed.50 According to Baran,51 these melanotic lines appear when melanocytes in the nail matrix are activated by repeated trauma. The causes are multiple, and in Spain we generally associate these striations with the use of certain drugs (hydroxyurea, doxorubicin, and zidovudine, among others50) rather than leprosy. Longitudinal melanonychia was the most common nail change in the leprosy patients studied by Kaur and coworkers,22 followed by other longitudinal striations, which also ranked second in the leprosy case series described by El Darouti and coworkers.23
Pitting of the Nail PlatePitting, or the presence of small round depressions on the surface of the nail plate, develops because of parakeratosis in the proximal matrix. The distribution pattern may or may not be uniform. Pitting may also be present in psoriasis, alopecia areata, and lichen planus, among other conditions19 and occurs in up to 4% of patients with leprosy.22
Flag SignAlternating bands of different colors on the nail constitute the flag sign, which arises as a consequence of the vasculopathy present in these patients. El Darouti and coworkers23 recently reported that 15% of leprosy patients and 5% of diabetic patients have this sign.
Pseudomacrolunula, or Diffuse LunulaPseudomacrolunula is an early sign that is characteristic of leprosy.47 The lunula extends distally, giving a whitish color to the nail, for which reason it is also known as apparent leukonychia. The white aspect recedes with pressure and does not change shape as the nail grows. The nail remains transparent, since the matrix and plate are healthy. Pseudomacrolunula was the most common nail abnormality in the series of 118 patients described by El Darouti and coworkers.23
Terry NailsA Terry nail has a particular type of macrolunula that is white, opaque, and covers the whole nail except a band of 1to 2mm along the distal border that remains pink or brown.17 First described by Terry in a patient with cirrhosis of the liver,18 this sign was linked to leprosy in 1987 by Singh and coworkers,52 who reported it in a patient in India. In the study of El Darouti and coworkers,23 17% of the patients had Terry nails.
True LeukonychiaIf the nail plate loses its transparency because of the presence of parakeratosis on the ventral side, the condition is known as true leukonychia. Keratinization of the distal nail matrix is the result of trauma.17,18
Hapalonychia and OnychorrhexisIn hapalonychia (soft, fragile nails) and onychorrhexis (brittle nails that break easily), the nails may curve over the finger pads; this complication is seen in mature, long-standing leprosy.36 Thus, it is more common in advanced stages of the disease, particularly on so-called claw hands.21,53,54
Transverse Lines (Beau Lines)Beau lines are solitary linear indentations that cross the nail and that grow out with the nail (Fig. 10). These grooves are the result of a temporary pause in nail growth. They may appear after a disease or injury to the nail and are associated with serious diseases, nutritional disorders (particularly zinc or iron deficiencies), and medications.55 These lines are also seen in leprosy because of severe type-2 lepra reactions or they may develop in relation to treatment with dapsone and/or clofazimine.56,57
Nail PallorThe nail pallor that may be present in patients with leprosy is caused by anemia when the disease becomes chronic, by hemolysis attributable to dapsone (methemoglobinemia), or by vascular impairment (Fig. 11).22,23
ConclusionIn summary, nail changes in leprosy are highly variable, originate as a result of many different processes, and reflect the extensive morbidity caused by infection with M leprae. We believe that familiarity with these changes is of great interest because, as we have shown in this review, the abnormalities have repercussions not only on the shape and appearance of hands and feet but also on function. Furthermore, significant complications and serious mutilation can develop.
Although we may think we will rarely or never meet diseases like leprosy in practice, our work as volunteer physicians or providing care for immigrants may well bring us into contact with patients experiencing these problems. At such times, an understanding of nail abnormalities, which are usually only superficially treated in textbooks, will become useful. This review is intended to help practitioners understand and improve the quality of life of these patients.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We would like to express our thanks to all who provide patient care at the Gambo General Hospital for leprosy patients, particularly to Nurse Deriba Lemma and to the hospital's head, Father Renzo Meneghini, member of the Consolata Missionaries. We are grateful for their patience and help, as this paper could not have been written without them.
Please cite this article as: Belinchón Romero I, et al. Las uñas en la lepra. Actas Dermosifiliogr.2012;103:276-284.