Tumescent anesthesia is a local anesthetic technique that consists of the infiltration of a large volume of solution with a low concentration of the local anesthetic agent and epinephrine. Its main advantages are that it achieves adequate anesthesia and a significant reduction in intraoperative and postoperative bleeding, leading to greater ease of surgery with the added benefit that it facilitates tissue dissection. This technique can be used safely for anesthesia of large areas, given that systemic absorption of the local anesthetic and vasoconstrictor agent is limited, reducing the incidence of systemic side effects. The simplicity and numerous applications and benefits of this technique make it very useful in current dermatologic surgical practice.
La anestesia tumescente es una técnica de anestesia local consistente en la infusión de un volumen importante de una disolución a baja concentración de anestésico local y adrenalina. Sus principales ventajas son que logra una adecuada anestesia y una reducción importante del sangrado operatorio y postoperatorio, permitiendo una cirugía cómoda con el beneficio añadido de facilitar la disección de los tejidos. Puede emplearse con seguridad en la anestesia de áreas extensas ya que se consigue una disminución de la absorción sistémica del anestésico local y del vasoconstrictor, reduciéndose la aparición de efectos secundarios sistémicos. Por su sencillez y sus múltiples aplicaciones y beneficios es una herramienta muy útil en la práctica de la cirugía dermatológica actual.
Tumescent anesthesia was first described in 1987 by Klein,1 who showed that a large volume of a solution containing a low concentration of lidocaine, epinephrine, and sodium bicarbonate could be injected into subcutaneous tissues before liposuction to prevent the copious intraoperative and postoperative bleeding associated with this procedure and to avoid the risks of general anesthesia.2 Since then slight changes in concentrations have been made, and the applications of Klein's technique have been extended to other types of plastic and cosmetic surgery as well as to skin surgery.3
Although the lidocaine-epinephrine combination provides adequate local analgesia and excellent vasoconstriction, this solution is acidic. Acidity can be reduced by adding sodium bicarbonate, bringing the pH of the buffered solution close to normal and very near the pKa of lidocaine (7.9); pain on injection of the solution is thereby reduced and as diffusion is faster, the onset of the local anesthetic effect comes more quickly.4,5
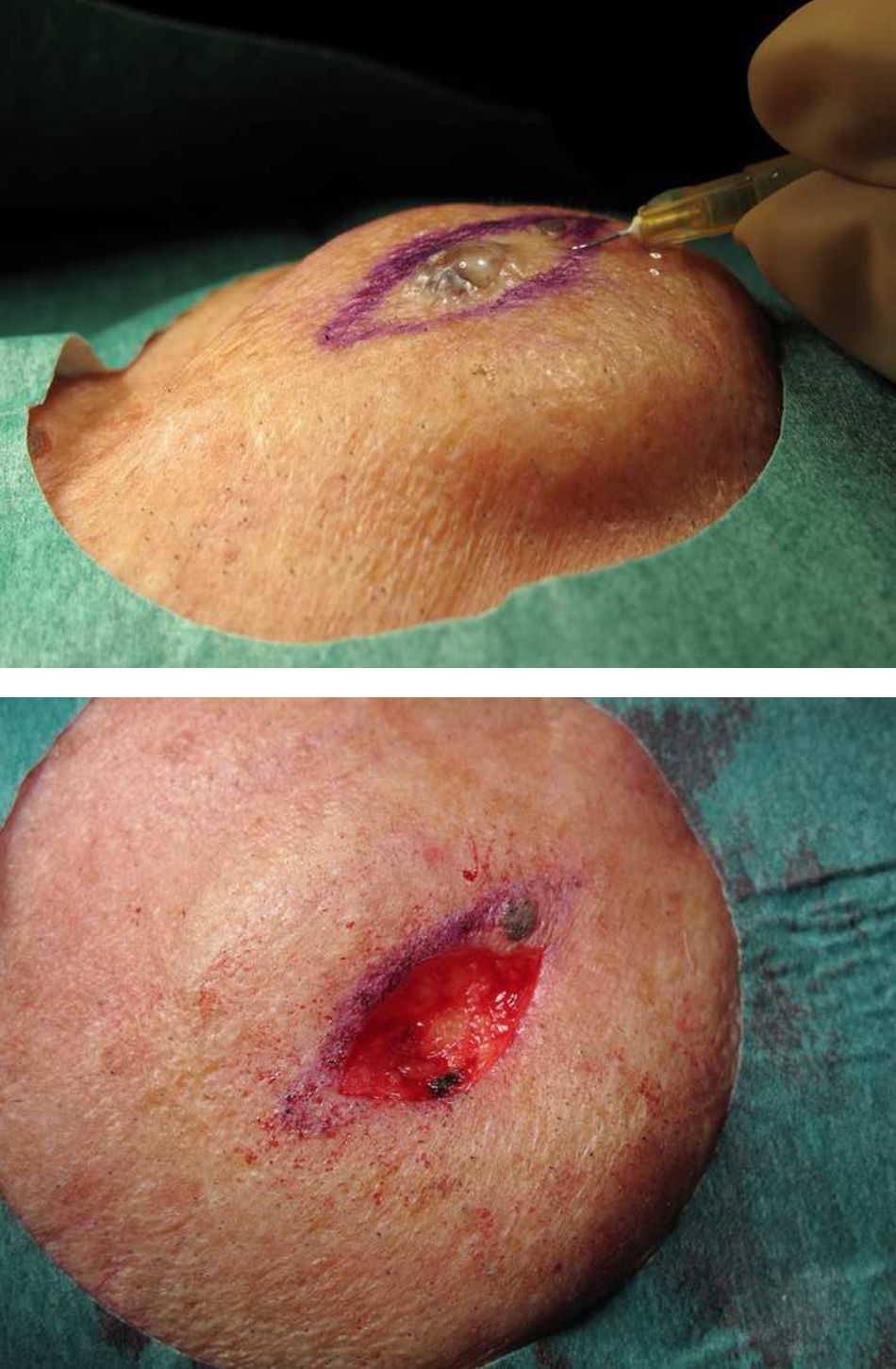
This technique is not difficult to perform and once the solution is prepared (Table 1), it is ready to be administered. Starting with subcutaneous injection through a small needle (24-27gauge) attached to a 10-or 20-mL syringe attenuates pain. Discomfort can be reduced further by applying ethyl chloride to the injection site, for its cooling analgesic effect, or simply by pinching or otherwise physically stimulating the neighboring skin to distract the patient from the painful point of entry. Pain is also reduced by initially infiltrating the relatively lax subcutaneous tissue; the solution can then be injected into the dermis.6,7 The anesthetized zone is easily recognizable by its pale,8 swollen appearance. The volume injected ranges from 10mL to amounts as high as 50to 100mL. If performing the technique for the first time, it is important to remember to inject a sufficient amount to significantly change the architecture of the infiltrated area and then wait while the solution drains into adjacent tissues and the architecture of the lesion is restored. If a large area is to be anesthetized, it is possible to switch to a larger and longer needle. Large volumes can be injected through a cannula connected to an infusion pump; alternatively, a bag containing the tumescent solution can simply be connected to a pressure cuff. Large amounts can then be transferred quickly and easily without repeated needle punctures.9
Recipe for a Tumescent Anesthetic Solution.
| 0.05mL of epinephrine (1 mg/mL) |
| 1mL of sodium bicarbonate (1 mol/L)a |
| 10-mL vial of 1% mepivacaine |
| 10-mL vial of 2% mepivacaine |
| 50mL of 0.9% physiological saline solution |
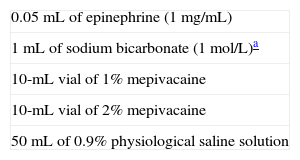
Tumescent anesthesia offers many benefits over traditional local anesthetic techniques. Adequate anesthesia can be achieved with diluted amounts of the local anesthetic. Thus, there is less systemic absorption of both lidocaine and epinephrine, and consequently fewer local and systemic adverse effects. Furthermore, the effect of tumescent anesthesia lasts longer, thanks to the reduced systemic uptake and more local concentration of the anesthetic. For all these reasons, more of the anesthetic can be infiltrated than is possible when the agent is injected conventionally for local anesthesia: as much as 55mg/kg10,11 can be injected with the tumescent method without causing toxicity. For patients who have heart disease or hypertension or who are taking β-blockers, epinephrine will also be safer in a tumescent solution.7 In addition, bleeding is significantly reduced (Fig. 1) during surgery and in the hours following the procedure. This advantage is the result of both the effect of epinephrine and the compression of blood vessels, which collapse under the increased hydrostatic pressure from the injected fluids.
One of the greatest advantages of this technique in dermatologic surgery, however, is that it facilitates tissue dissection: large-volume fluid infiltration mechanically separates the different anatomical planes, making it easier to follow them when resecting lesions and to avoid important anatomical structures such as arteries and nerves in the surgical field.
The main theoretical disadvantage of tumescent anesthesia in dermatologic surgery is the significant architectural deformation caused by the infiltrating solution. This problem can be circumvented by planning the intervention carefully and delineating the area with a surgical skin marker before injecting the solution. Gentle compression of the zone a few minutes after completing infiltration will reduce the initial swelling.
Safety has been demonstrated by studies showing a lack of adverse effects when this technique has been used in liposuction, which requires large volumes of anesthetic solution (up to 4 L); these studies have also found that postoperative analgesia is more satisfactory.8,12
The uses of tumescent anesthesia in dermatologic surgery, which are many and varied, usually require the infiltration of no more than 100mL. The technique can be used when removing small skin lesions and epidermal cysts as well as for complicated flaps or full- or partial-thickness grafts and hair micrografting13; sentinel lymph node biopsy in melanoma14; laser repair of abrasions15; and hair removal from particularly sensitive areas or from zones where topical anesthesia is difficult, such as the axillas.16 Tumescent anesthesia is also useful for reducing bleeding during debridement or skin grafting in burn patients.17 The tissue elevation caused by local tumescence can also be used to advantage in order to facilitate shave biopsies or excisions, curettage, and in general the removal of lesions in cartilaginous structures such as the outer ear.
Finally, we suggest that tumescent anesthesia should be used regularly in scheduled dermatologic surgery so that we can take advantage of its many benefits, simplicity, and safety. This practice has become routine in our dermatology department, where even large interventions are done without resort to nerve blocks, which we now reserve for procedures requiring anesthesia of fingers or toes.
Conflict of InterestsThe authors declare that they have no conflicts of interest.
Please cite this article as: Dávila P, García-Doval I. Anestesia tumescente en cirugía dermatológica. Actas Dermosifiliogr.2012;103:285-7.