Histoplasmosis is a systemic mycosis caused by the dimorphous fungus Histoplasma capsulatum (H. capsulatum). The fungus enters the body through the respiratory tract in the form of microconidia, which are transformed into intracellular yeast-like structures in the lungs before disseminating hematogenously. Primary infection is usually asymptomatic and self-resolving. Some patients develop severe disease with acute or chronic respiratory involvement. Immunosuppressed patients, mainly those with altered cellular immunity, may have disseminated disease with variable mucocutaneous involvement characterized by papules, nodules, gummas, or ulcers with a granulomatous base. We report the case of 3 HIV-negative patients infected by H capsulatum in whom diagnosis based on the skin lesions proved essential for early initiation of treatment.
La histoplasmosis es una micosis sistémica causada por el hongo dimorfo Histoplasma capsulatum (H. capsulatum). Este entra en el organismo a través del tracto respiratorio en forma de microconidias, que a nivel pulmonar se transforman en elementos levaduriformes intracelulares, y luego se diseminan por vía hematógena. La primoinfección suele ser asintomática y autorresolutiva. Algunos pacientes desarrollan una enfermedad grave con compromiso respiratorio agudo o crónico. Los pacientes inmunosuprimidos, principalmente aquellos con alteración de la inmunidad celular, pueden presentar una enfermedad diseminada con compromiso mucocutáneo proteiforme, con pápulas, nódulos, gomas o úlceras de fondo granulomatoso. Se comunican 3 casos clínicos de pacientes inmunosuprimidos no VIH, con infección por H. capsulatum, en quienes el diagnóstico a partir de las lesiones cutáneas resultó fundamental para el inicio precoz del tratamiento.
Histoplasmosis is a systemic mycosis caused by the dimorphic fungus Histoplasma capsulatum, which enters the body upon inhalation of microconidia. Phagocytosis of these microconidia by alveolar macrophages transforms them into yeast-like structures, which are then disseminated in the bloodstream. Cell-mediated adaptive immunity promotes the activation of macrophages and the formation of epithelioid granulomas to control the infection.1,2 This response is absent in immunocompromised patients, and the infection spreads to multiple organs. We describe 3 cases of H capsulatum infection in patients with compromised immunity unrelated to human immunodeficiency virus (HIV) infection. In all cases, diagnosis based on skin lesions was fundamental to allow early initiation of treatment.
Case DescriptionsCase 1A 54-year-old man reported fever, asthenia, dyspnea on moderate effort, and mucocutaneous lesions that had appeared 3 months earlier. The patient had an erythematous plaque with a tough, elastic-like consistency and diffuse borders that covered the nasal dorsum and left malar region, and on which sat a painful, rounded ulcer with a fibrinous base (Fig. 1). On the patient's soft palate was an ulcer 2cm in diameter with clearly defined borders and a granulomatous base (Fig. 2). The results of laboratory tests were as follows: hemoglobin, 14g/dL; white blood-cell count, 5540/mm3; CD4+ T-cell count, low (78 cells/L); platelet count, 234 900/mm3. Liver and kidney function were normal, and the results of the tuberculin test, blood tests for HIV and hepatitis C and B, and the venereal disease research laboratory test were negative. The patient's protein profile was normal and the results of tests for antibodies (immunoglobulin M) against the Epstein-Barr virus, herpes 6 virus, cytomegalovirus, parvovirus B19, and human T-cell leukemia virus type 1 were negative. Computed tomography (CT) of the thorax, abdomen, and pelvis revealed a bilateral micronodular pulmonary infiltrate, mediastinal adenopathy, and bilateral adrenal gland hyperplasia. Direct microscopic examination of the lesions with Giemsa stain revealed intracytoplasmic yeast-like structures, with a predominantly polar staining pattern. Histology showed histiocytes and multinucleated Langhans giant cells in the dermis, with intrahistiocytic yeast-like structures. Skin cultures were positive for H capsulatum. The patient was treated with liposomal amphotericin (3mg/kg/d) for 10 days. Continued outpatient treatment with itraconazole (400mg/d) for 1 year resulted in resolution of the clinical signs. Serial blood tests ruled out HIV infection. Autoantibody analyses and serial blood tests revealed no immunological or hematological diseases. A diagnosis of idiopathic lymphopenia was established.
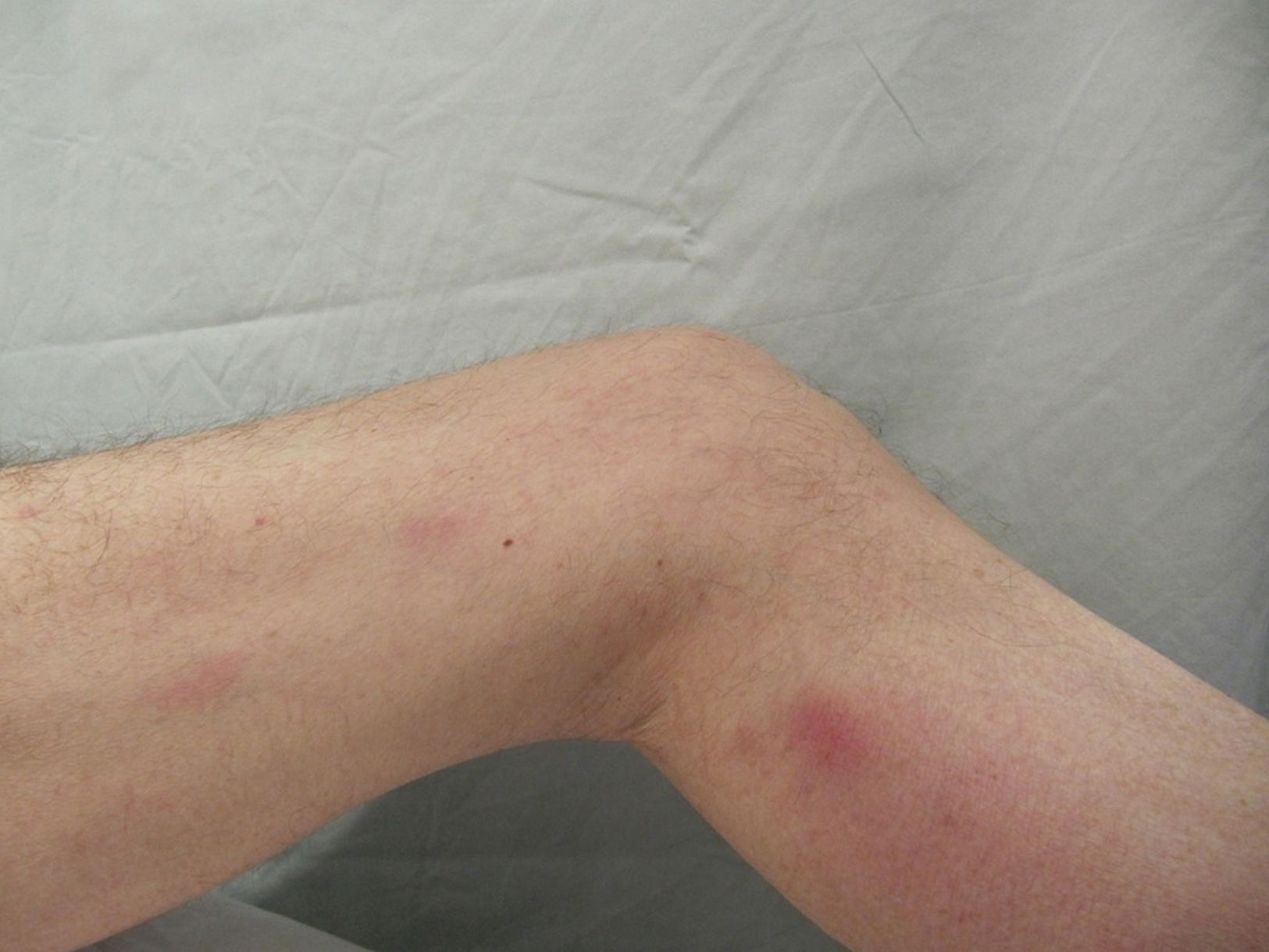
The patient was a 57-year-old man who had undergone a heart transplant for dilated cardiomyopathy and was being treated with mycophenolate mofetil (2g/d) and meprednisone (8mg/d). He reported fever, weight loss, and cough that had appeared 15 days earlier. The patient had multiple painful erythematous nodules 1cm in diameter on the lower limbs (Fig. 3). The results of serological tests for HIV and hepatitis B and C were negative. A chest CT scan revealed a cotton-like infiltrate in the middle lobe of the right lung. H capsulatum was detected by histology and culture. The clinical signs resolved after 1 year of treatment with itraconazole (400mg/d). Bimonthly check-ups were scheduled.
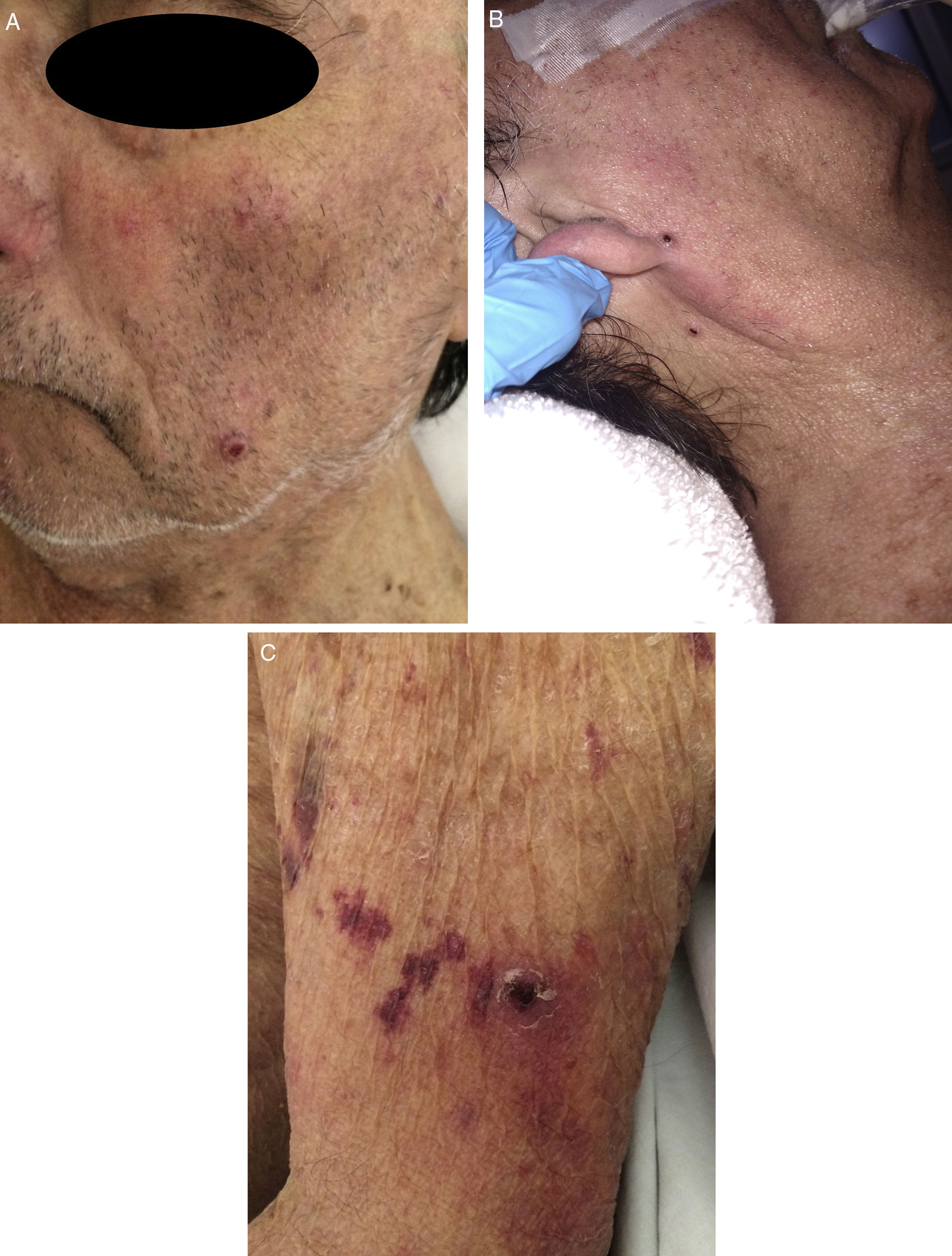
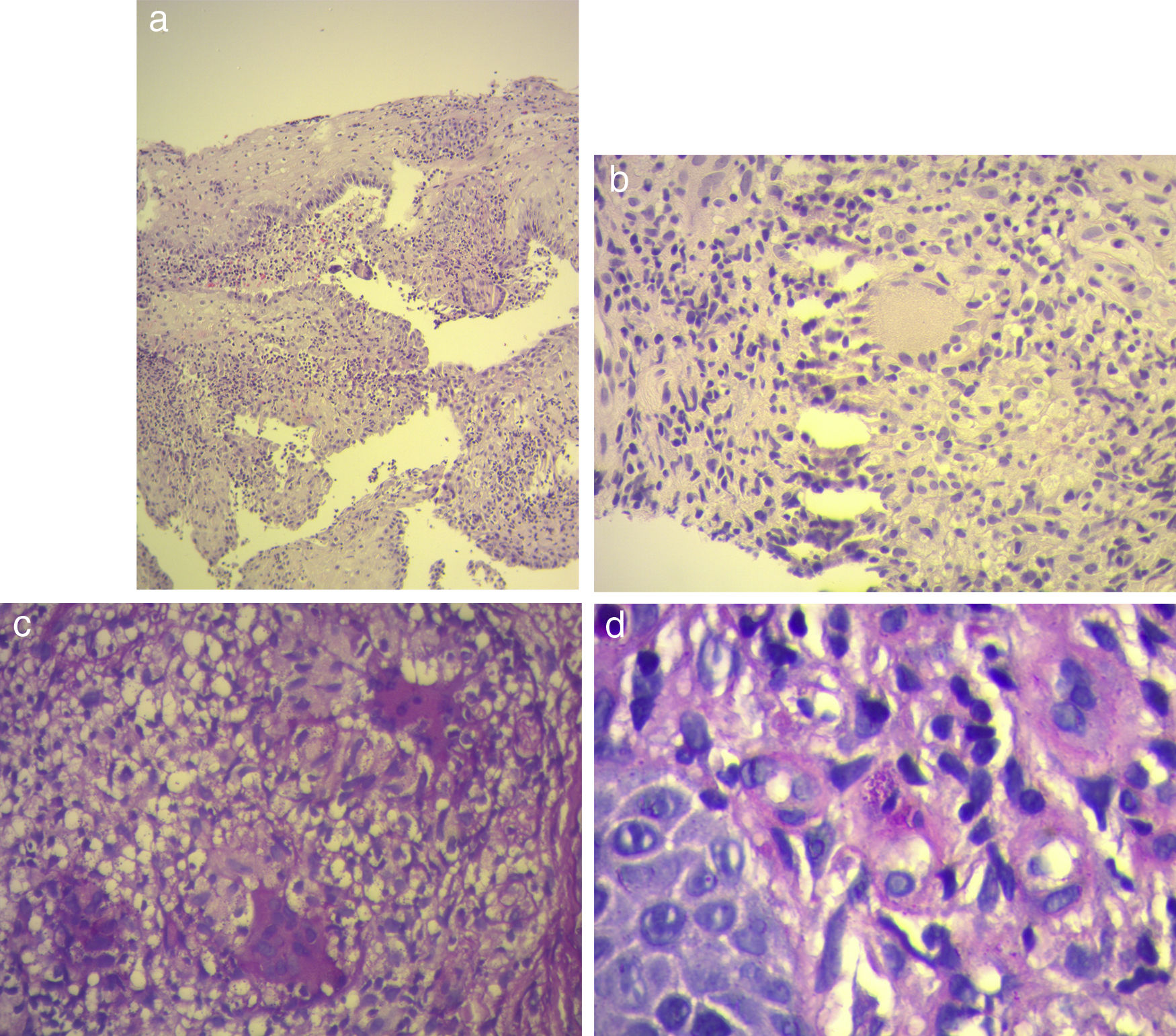
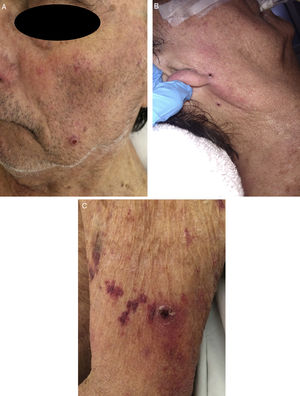
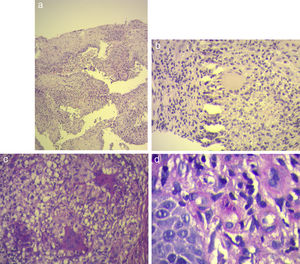
Case 3The patient was a 75-year-old man who had undergone a liver transplant for primary sclerosing cholangitis and was being treated with methylprednisone (4mg/d), tacrolimus (3mg every 12h), and mycophenolic acid (360mg every 12h). He complained of fever and sensory deterioration. Multiple rounded purpuric papules with central umbilication ranging in size from 2mm to 4mm were located on the face, abdomen, and limbs (Fig. 4). Chest CT showed a bilateral micronodular pulmonary infiltrate. Brain CT and cerebrospinal fluid analysis revealed no findings of note. The results of serological tests for HIV and hepatitis B and C were negative. The presence of H capsulatum was demonstrated by direct smear using Giemsa stain as well as culture and skin histopathology (Fig. 5). Treatment with liposomal amphotericin (5mg/kg/d) was initiated. However, 4 days later multiple organ failure developed and the patient died.
A, Histiocytes and multinucleated Langhans giant cells in the dermis (hematoxylin-eosin, original magnification ×10). B, Multinucleated Langhans giant cells (hematoxylin-eosin, original magnification ×40). C, Multiple multinucleated giant cells (periodic acid-Schiff, original magnification ×40). D, Intrahistiocytic yeast-like structures (periodic acid-Schiff, original magnification ×100).
Two varieties of H capsulatum (var. duboisii and var. capsulatum, found in Africa and the Americas, respectively) are pathogenic to humans, and histoplasmosis is the most prevalent mycosis in endemic countries.2,3 Several cases reported in the United States and Latin America have highlighted the presence of disseminated infections in immunocompromised patients, 70% to 90% of whom had HIV infection.4,5 Cases have been reported in countries in Africa, Asia, and Europe, and histoplasmosis is therefore considered a globally distributed infection.6
In the majority of cases, primary exposure to H capsulatum results in a nonsymptomatic infection or causes nonspecific symptoms and resolves without need for treatment.2–7 Disseminated histoplasmosis occurs in patients with impaired cell-mediated immunity, such as HIV-positive patients with a CD4+ count of less than 100 cells/μL,7 patients with oncohematological diseases, recipients of solid organ or hematopoietic cell transplants, patients treated with immunosuppressants or tumor necrosis factor antagonists, and those with congenital T-cell deficiencies.1,6 Two of the patients we have described had been treated with immunosuppressants after undergoing solid organ transplantation, and one was diagnosed with idiopathic CD4+ lymphopenia after other infectious and neoplastic diseases were ruled out as possible causes of immunodeficiency.
Clinical signs of disseminated disease include constitutional symptoms, organomegaly, generalized lymphadenopathy, lung and/or liver disease, and bone marrow and adrenal gland deficiencies. Central nervous system compromise is observed in 5% to 10% of patients.2,3,8 In Latin America, cutaneous involvement is observed in 38% to 85% of histoplasmosis patients with AIDS, as compared with 10% to 25% in the rest of the world. This higher frequency in Latin America is thought to be due to the presence of different phylogenetic species of H capsulatum (classes 5 and 6) in the region.2,9 Skin lesions can be primary, resulting from direct inoculation of the fungus into the skin (although this is very rare), or secondary to hematogenous spread of the fungus. Lesions are characterized by marked polymorphism and can manifest as papules, plaques, pustules, nodules, erosions, or molluscoid or acneiform lesions.2,3,10 The most common mucosal lesions are granulomatous ulcers located on the tongue, palate, and buccal and gingival mucosa, and less frequently on the larynx and the penis.1,9,10 The first of our patients presented with ulcerated granulomatous lesions, while the other 2 patients had multiple, disseminated nodular and molluscoid lesions.
Diagnosis is established by direct microscopy using Giemsa or silver methenamine stains, serum antigen detection, and detection of specific antibodies by enzyme-linked immunosorbent assay.11 Isolation of the fungus in tissue culture is the gold standard for diagnosis, but requires the use of facilities and practices corresponding to biosafety level 3.11,12 Histology reveals the presence of multinucleated giant cells and granulomas with or without caseating necrosis, and the presence inside macrophages of yeast-like structures, which can be visualized using periodic acid-Schiff, methenamine silver, or Gomori-Grocott staining. The epicutaneous histoplasmin test is used for epidemiological studies but is not useful for diagnosis.6,9 Another diagnostic method is the detection of DNA by polymerase chain reaction techniques, which have a diagnostic sensitivity and specificity close to 90% and are useful in severely immunocompromised patients.4,12 In the 3 cases presented here, H capsulatum was isolated from skin cultures.
Liposomal amphotericin B is the drug of choice for initial treatment in patients with systemic compromise.13 For oral treatment, azo compounds are used. Currently, itraconazole is the treatment of choice. It is administered at 400mg/d for at least a year. To reduce the risk of relapse, its blood concentration should be measured periodically until levels reach 1 to 2μg/mL.11,14 Other recently developed triazoles, such as voriconazole and isavuconazole, have shown in vitro activity against H capsulatum similar to that of itraconazole. However, owing to their frequent interactions with other drugs administered long term, triazoles are reserved for the small number of patients with disseminated histoplasmosis who cannot tolerate other treatments.13,15 Further studies are required to demonstrate their advantages over other currently used drugs.15
ConclusionHistoplasmosis is a systemic mycosis that should be included in the differential diagnosis of comparable skin lesions, even in nonendemic countries given today's high levels of migration. It is necessary to fully review the patient's clinical history, in which all recent trips and activities should be recorded, in order to establish a diagnosis and initiate appropriate and timely treatment. This is especially important in immunocompromised patients.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Gómez-Santana LV, Torre AC, Hernández BA, Volonteri VI, Laura B, Luis-Galimberti R. Manifestaciones mucocutáneas de la infección por Histoplasma capsulatum en pacientes inmunosuprimidos. Actas Dermosifiliogr. 2018;109:e27–e32.