Milroy disease or primary congenital lymphedema was first described in 1892. It is characterized by congenital lymphedema of the lower limbs. Associations have been observed between chronic lymphedema and a number of neoplasms, including angiosarcoma, Kaposi sarcoma, lymphoma, basal cell carcinoma, melanoma, and squamous cell carcinoma (SCC).1,2
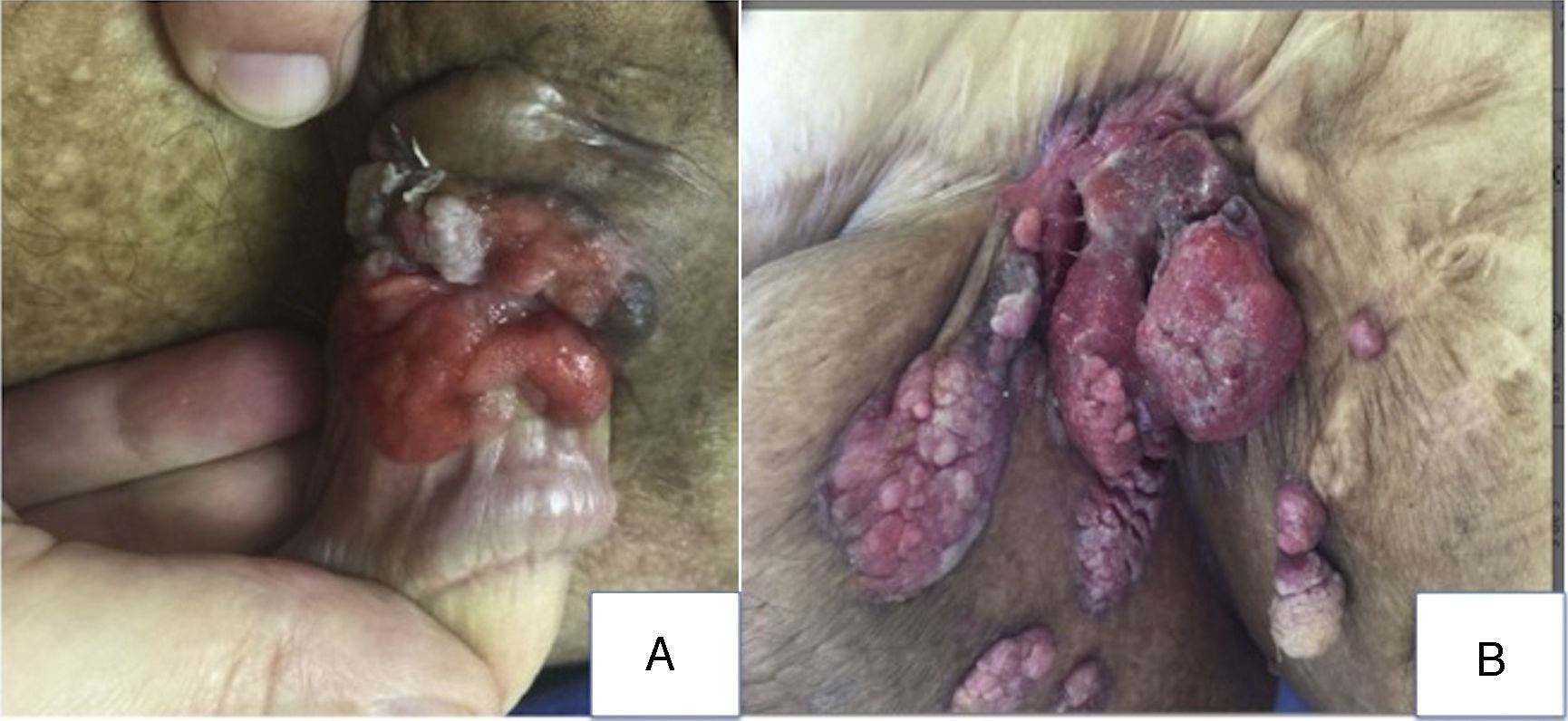
A 58-year-old man with a history of congenital lymphedema, with aplasia of lymph vessels in both lower limbs demonstrated on lymphoscintigraphy in childhood and a hereditary family history of the same disease (father), had undergone numerous operations to improve lymphatic circulation. He was seen in the dermatology department for a deterioration of the lesions that affected both lower limbs symmetrically and the genitalia since birth. In the pretibial region, the calves, and the dorsum of the feet, the patient presented papillomatous verrucous plaques, areas of fibrosis and atrophy, retracted scars, and small circular ulcers with erythematous borders and a seropurulent exudate. The thighs presented marked, hard edema, with surgical scars, and there was massive edema of the testicles that deformed the region, associated with verrucous plaques (Fig. 1, A and B).
A multilobulated tumor measuring 14cm in diameter was observed in the left inguinal region. The exophytic tumor had a friable erythematous surface covered by fibrin (Fig. 2A). A poorly defined erythematous exophytic tumor with hyperkeratotic areas and elevated pigmented borders was observed on the shaft of the penis (Fig. 2B).
On a suspicion of SCC or angiosarcoma, incisional biopsies were taken from the lesions in the left inguinal region and on the penis, and computed tomography (CT) of the abdomen, pelvis, and lower limbs was requested.
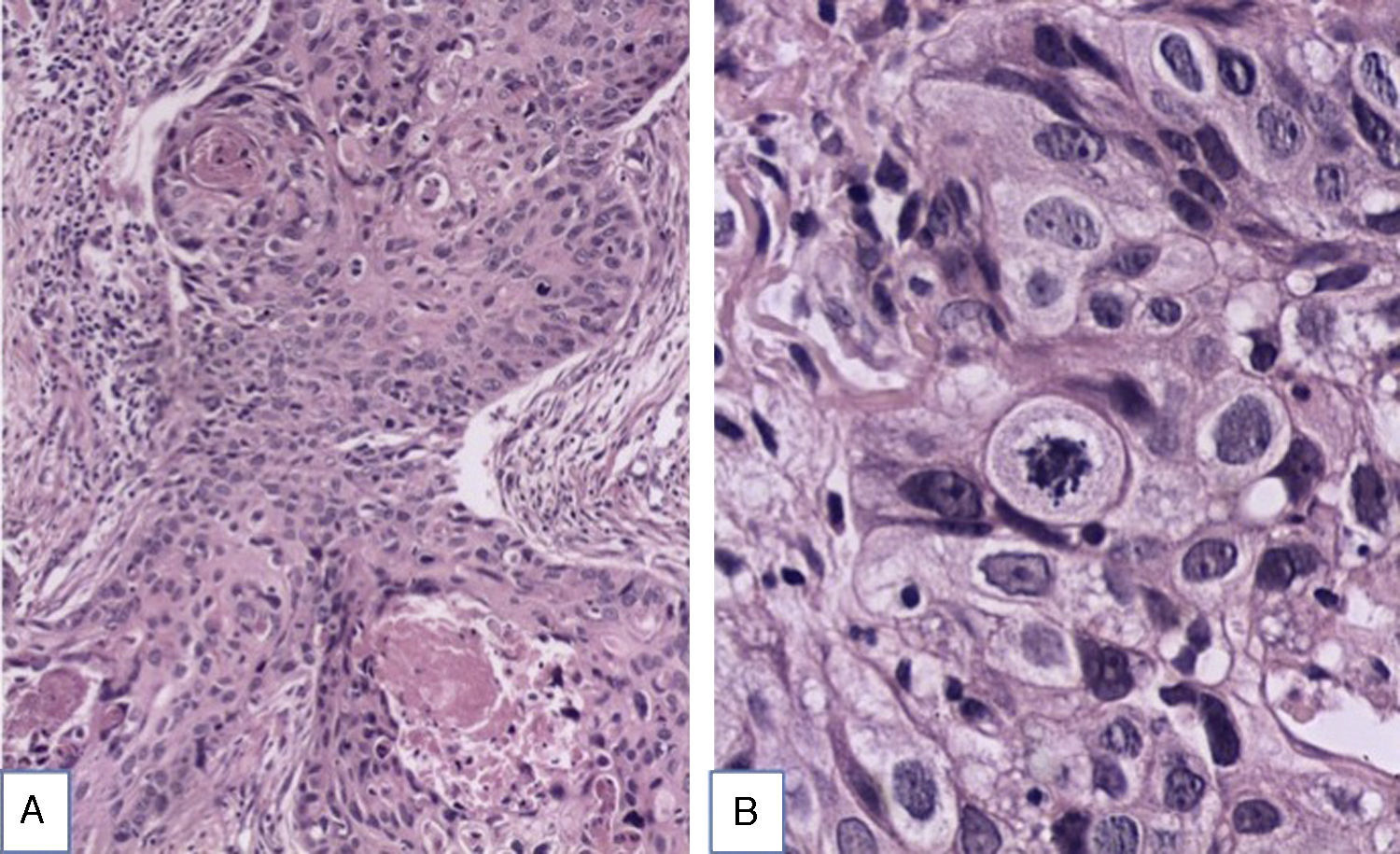
Histopathology revealed a poorly differentiated, invasive squamous cell carcinoma with a thickness of 4.22mm, Clark level V, with 11 mitoses per mm2, and, on the penis, a well-differentiated invasive SCC with a thickness of 1.2mm, Clark level IV, with 15 mitoses per mm2. Neither tumor presented perineural or lymphovascular invasion or association with human papillomavirus (Fig. 3, A and B). On CT, numerous lymph nodes with a diameter less than 1cm were visible in the mediastinum and more than 15 lymph nodes of up to 12mm diameter in the right axilla. The patient was referred to another hospital where he has received chemotherapy with paclitaxel, cisplatin, and ifosfamide; he has completed 4 cycles but has shown no clinical or radiological improvement.
Lymphedema is a progressive edema of the tissues secondary to a dysfunction of the lymphatic system. It can be primary or secondary. Primary lymphedema is due to abnormal development of the lymphatic system and the secondary form is due to trauma, lymph-node resection, tumors, or infections such as filariasis. Secondary lymphedema accounts for 99% of cases.1–3
Primary lymphedema is usually idiopathic, with no hereditary family history. The incidence is 1.15 per 100000 population.3 Non-idiopathic causes include a number of diseases with an autosomal dominant pattern of transmission, such as Milroy disease, which is characterized by congenital lymphedema of the lower limbs.1–5 The locus has been mapped to 5q35.3 and the mutated gene is FLT4, which codes for endothelial growth factor receptor 3. It presents with lymphedema of the lower limbs affecting the dorsum of the feet, knees, and thighs; the edema has a woody texture.4–7
Diagnosis is made in patients with symmetrical bilateral congenital edema of the lower limbs, but other factors must be taken into account, such as a positive family history and mutation of endothelial growth factor receptor 3 (present in 42% of patients).4
The lymphedematous region becomes an immunocompromised territory due to altered migration of dendritic cells, T cells, and macrophages to the dermal lymph vessels.7,8 One of the most common tumors to arise in Milroy disease is angiosarcoma (Stewart-Trevès syndrome), which, despite being more common in patients after surgery for breast cancer, has also been reported in lymphedema of the lower limbs. Other associated tumors are Kaposi sarcoma, lymphoma, basal cell carcinoma, melanoma, and SCC. The time over which the neoplasm develops can vary from years to decades.6–10 The most relevant risk factors for SCC in patients with primary lymphedema are common warts, angiosarcoma, widespread vitiligo, chronic ulcers, chronic verrucous hyperplasia, dystrophic epidermolysis bullosa, and a history of UV-B therapy.9,10
Only 15 cases of SCC associated with chronic lymphedema have been reported, and only 3 of these were associated with primary lymphedema. All these cases occurred in men. The mean age was 40.5 years and the most common site was on the lower limbs.8–10
The treatment of choice is resection of the tumor, combined with lymphadenectomy when lymph-node metastases are present. Adjuvant radiotherapy and chemotherapy may be administered.10
The importance of this case derives from the low frequency of these tumors in the context of primary lymphedema and the few cases reported in the literature. Knowledge of this association will favor early diagnosis and appropriate treatment.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Cheirif-Wolosky O, Ramírez-Hobak L, Toussaint-Caire S, Lammoglia-Ordiales L. Enfermedad de Milroy o linfedema primario congénito asociado a carcinoma espinocelular invasor. Actas Dermosifiliogr. 2016;107:865–867.