Epithelioid hemangioma (EH) is a rare, benign, idiopathic vascular proliferation first described by Wells and Whimster in 1969.1 It typically arises in the skin or subcutaneous cellular tissue of the head and neck and, more rarely, has been reported on the trunk and limbs. Trauma, infection, and an underlying vascular malformation have been proposed as possible causes. We present the case of an adolescent male diagnosed with multiple EHs on the left upper limb. Imaging studies revealed a large asymptomatic aneurysmal lesion that required surgery in order to bring about resolution of the EH lesions.
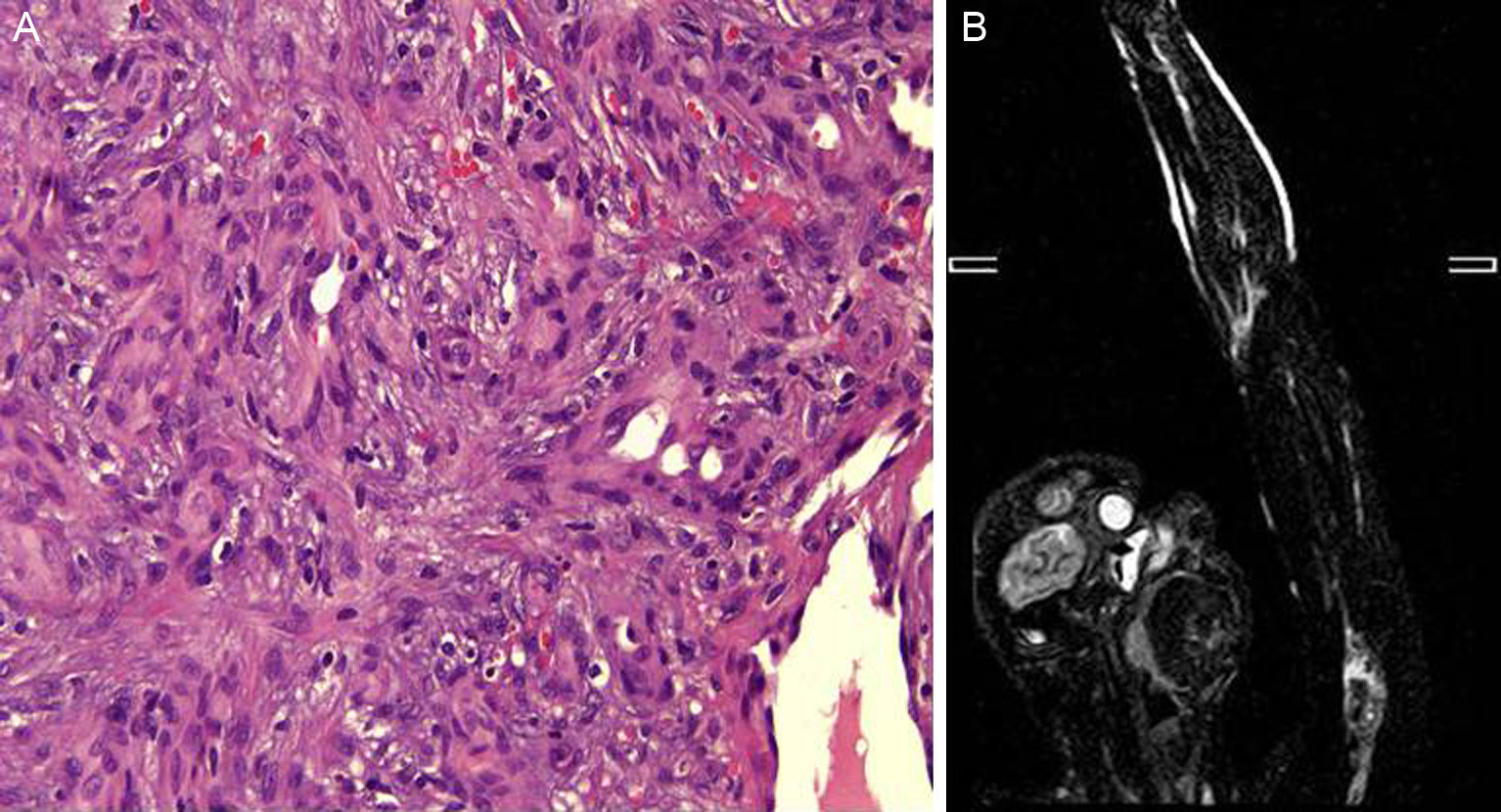
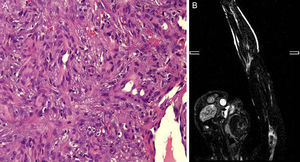
A boy aged 14 years with no past history of interest consulted for the progressive appearance over the previous 2 years of a number of violaceous tumors on his left upper limb. He described the lesions as slow growing and asymptomatic, though some of the lesions had bled on minimal trauma in recent months. Examination revealed the presence of multiple erythematous-violaceous cutaneous and subcutaneous papules and tumors in a linear distribution along the left upper limb (Fig. 1); lesions in the distal region of the second, third, and fourth fingers produced clubbing, and some had superficial hemorrhagic scabs. Biopsy was performed on a suspicion of lesions of vascular origin, and histology revealed a proliferation of endothelial cells lining large vascular spaces, with a lymphocytic inflammatory infiltrate and abundant eosinophils in the dermis (Fig. 2A). Immunohistochemistry was positive for CD31 and CD34. Based on these findings, we made a diagnosis of EH. Complete blood count, routine biochemistry, and coagulation studies were within normal limits except for the presence of a moderate peripheral eosinophilia. Results of the imaging studies, including magnetic resonance imaging (MRI) and arteriography of the affected limb, suggested the existence of a complex aneurysmal lesion in the proximal humeral artery, with destructured vessels and arterial occlusion, and repermeabilization distal to the aneurysmal dilatation (Fig. 2B). Vascular nests were observed at the elbow and in the hand, supplied mainly by a branch arising from the area of the aneurysm. Venous return was also abnormal. The final diagnosis was arteriovenous malformation in the left upper limb with humeral artery pseudoaneurysm. Treatment involved resection of the lesion with by-pass using basilic vein from the same arm. Three months after the operation we observed a surprising reduction in the size of the EHs, some of which had disappeared completely. A number of residual fibrotic tags were observed on the distal areas of the fingers (Fig. 3). Six months after surgery the patient continued on prophylactic antiplatelet treatment (acetylsalicylic acid, 100mg/d) and there was no recurrence of the EHs.
A, Histology showing the vascular proliferation of epithelioid endothelial cells with a solid pattern lining vascular spaces. Hematoxylin and eosin, original magnification ×40. B, Magnetic resonance angiography image of the arteriovenous malformation in the left upper limb, showing occlusion of the proximal humeral artery.
EH occurs mainly in adult patients of all races; it is rare in the pediatric population. Involvement of the trunk and limbs is extremely rare.2 Clinically they present as reddish-brown papules and tumors that are usually asymptomatic, though they may give rise to pruritus, bleeding, ulceration, or pain, due mostly to lesion growth. They may be superficial or deep; few cases with multiple lesions or a zosteriform pattern have been reported.3,4 Peripheral eosinophilia is observed in less than 20% of cases, and a regional lymphadenopathy more rarely still. Histologically, the lesions are characterized by a proliferation of large endothelial cells of epithelioid morphology that obstruct the vessel lumen, associated with a variable lymphoplasmacytic inflammatory component with abundant eosinophils. Immunohistochemistry is positive for endothelial markers CD31 and CD34, and negative for epithelial markers (cytokeratins).5 In children, the main differential diagnosis is with pyogenic granulomas,6 whose eruptive presentation has been associated with certain drugs, minor trauma, and Kimura disease (predominantly in oriental patients, associated with peripheral lymphadenopathy, hypereosinophilia, and elevated immunoglobulin E levels).7 Other conditions with differing degrees of malignancy must also be considered, including hemangioendothelioma and angiosarcoma5; the presence of mitoses, cellular atypia, and morphological alterations will orient the diagnosis. A number of theories on the etiology of EHs have been proposed, with debate over whether this is a true neoplasm, a reactive process with a traumatic or infectious origin, or is secondary to an underlying vascular malformation.2 The presence of arteriovenous connections may be observed histologically.3 However, it may require the expertise of an experienced dermatopathologist to identify their presence in venules and capillaries. Imaging studies including MRI or arteriography are recommended to exclude identifiable arteriovenous abnormalities susceptible to treatment, as in our case. Other treatment options described in the literature include surgery, corticosteroids, radiotherapy, intralesional chemotherapeutic agents, cryotherapy, and laser.8 Recurrences have been reported in around 10% of cases and spontaneous regression has been observed.9
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Martínez-Peinado C, Ruiz-Villaverde R, Galán-Gutierrez M, Martínez de Victoria JM. Hemangioma epiteloide múltiple lineal asociado a malformación vascular quiescente. Actas Dermosifiliogr. 2016;107:862–864.