Skin metastases are relatively rare, with an incidence of less than 1% among patients with visceral neoplasms.1 However, this rate increases to 24% in patients in whom the primary tumor is a breast cancer.2 Clinical suspicion of metastases is usually based on the previous existence of a malignant primary tumor, although a third of skin metastases are discovered before the primary tumor.3 Immunohistochemistry is a fundamental technique to establish the connection with the tumor of origin, and a number of diagnostic algorithms have been developed to identify this connection.4
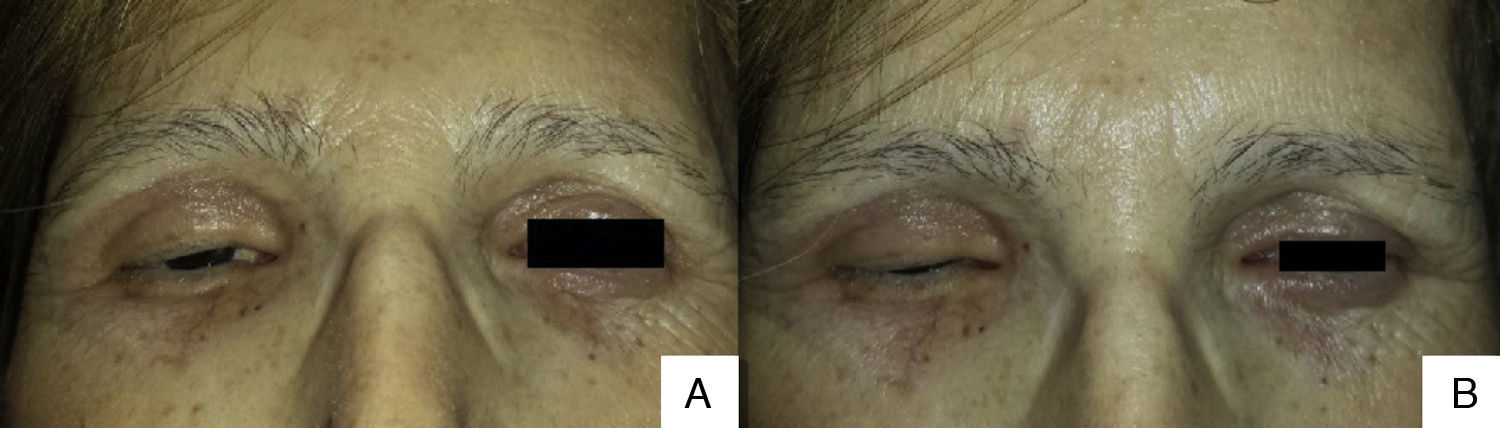
We present the case of a 55-year-old woman diagnosed with lobular breast carcinoma 15 years earlier. The patient was referred to our unit for a 1-year history of lesions that had arisen in the cervical region and that had extended to the upper third of the back and chest. Physical examination revealed hard, well-defined, edematous, erythematous papules and plaques in the posterior cervical region (Fig. 1), and localized erythema of all 4 eyelids that infiltrated to the deeper planes and interfered with eye opening (Fig. 2A) and closure (Fig. 2B).
At the time of consultation, the patient's tumor was stage IVB, with uterine and gastric metastases that had been treated surgically. She had received multiple cycles of chemotherapy and radiotherapy, and continued on treatment with letrozole.
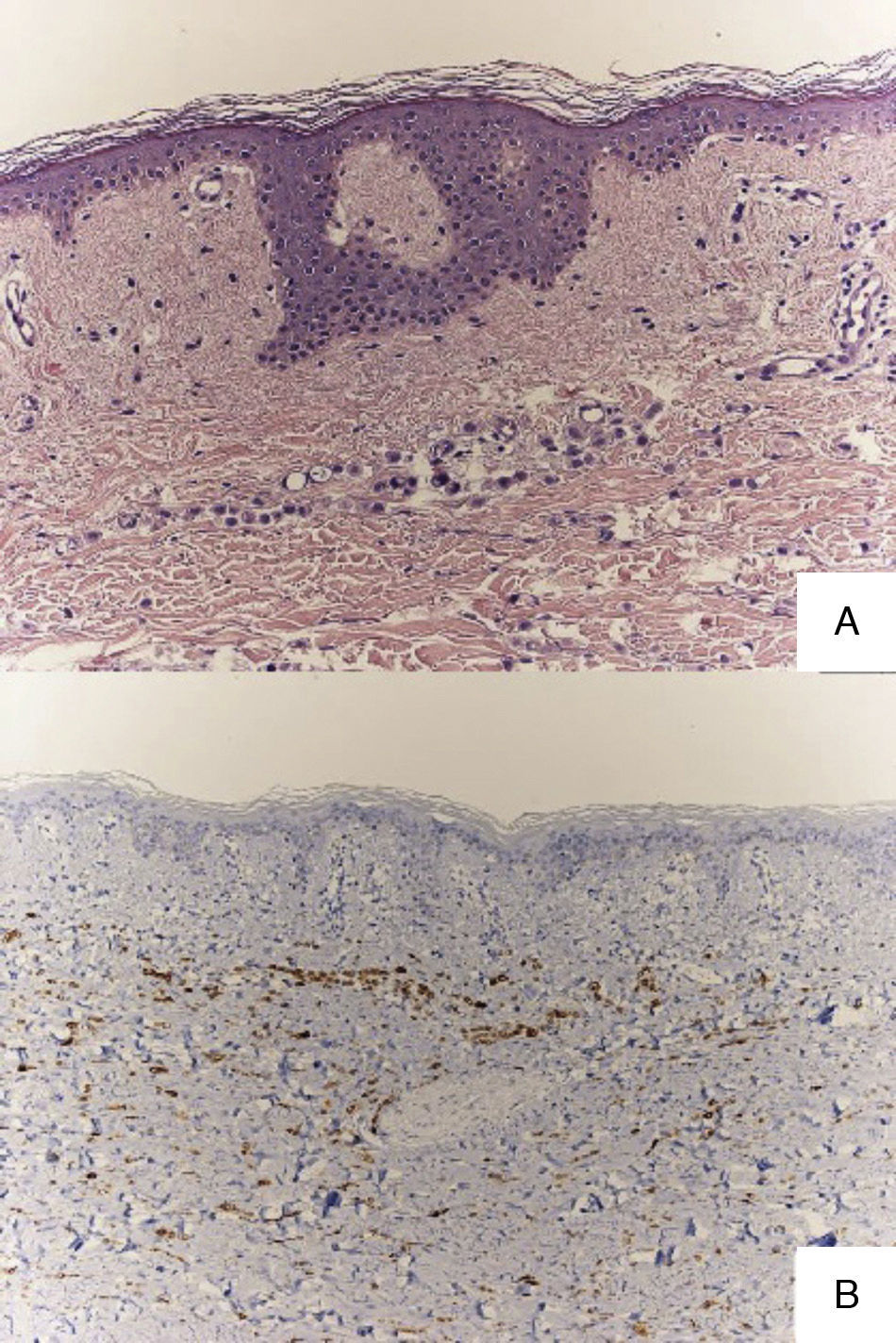
Histology of all the biopsies performed showed a dermal infiltrate of anaplastic cells arranged in cords (Fig. 3A). The cells were positive for GCDFP-15 stain (Fig. 3B), weakly positive for estrogen and progesterone receptors, negative for her2, and had a Ki67 proliferation index of 20%. A further cycle of chemotherapy was therefore administered with capecitabine, 2g/d, but the patient died 2 months after starting the treatment.
Skin metastases are a very rare cause of eyelid tumors, accounting for less than 1% of malignant lesions of the eyelids.5 Three clinical forms have been described: the nodular form, which is the most common and is characterized by painless subcutaneous nodules that can be confused clinically with a chalazion6; the diffuse inflammatory pattern, with a morpheaform appearance, as in our case; and the ulcerated form, in which histology reveals an infiltrate that extends beyond the dermis into the epidermis.
The other structures of the orbit can be affected in any case,7 and imaging studies or ophthalmologic examination is therefore recommended. In our patient, we observed diffuse hyperechoic retroocular images that surrounded the optic nerves, suggestive of metastatic infiltration.
Recently, Martorell-Calatayud et al.8 reported 2 cases similar to ours, with bilateral eyelid metastases, and they gathered 11 previously published cases. In 9 of those cases, the primary neoplasm was a breast carcinoma and in the remaining 2 it was a gastric adenocarcinoma. Skin metastases affecting all 4 eyelids are very rare. They are associated with long-standing breast carcinoma and indicate systemic spread of the neoplastic disease. In addition to the previously mentioned gastric and uterine metastases, subsequent imaging studies in our patient revealed rectal involvement, peritoneal carcinomatosis, bone metastases, and metastases in the posterior region of the orbit.
It is currently thought that the increase in the incidence of metastases at these particular sites is due to the increased survival of cancer patients.9 In conclusion, in our patient with a 15-year history of malignant disease, the administration of multiple cycles of chemotherapy was interpreted as a factor that favored the appearance of this rare type of metastasis.
Please cite this article as: Díaz-Martínez MA, Almodóvar-Real A, Ruiz-Villaverde R, Ruiz-Carrascosa JC. Metástasis en antifaz, letálides de pronóstico nefasto. Actas Dermosifiliogr. 2016;107:263–264.