Dermatologic manifestations of leukemia can be both specific and nonspecific (e.g., opportunistic infections, purpura and ecchymosis, Sweet syndrome). Leukemia cutis refers to the infiltration of the skin with neoplastic leukocytes and its early diagnosis has important prognostic implications. We report on 17 cases of leukemia cutis seen in our department between 1994 and 2014 and describe the characteristics of the patients (age, sex, medical history), the morphology of the lesions, and associations with systemic disease. Most of the patients were male and the most common associated malignancy was acute myeloid leukemia. The most frequent dermatologic manifestations were nodules or erythematous papules on the limbs. We describe our experience with the diagnosis and management of leukemia cutis over a period of 20 years and emphasize the importance of clinical signs in the early diagnosis of this condition.
Las manifestaciones dermatológicas de las leucemias incluyen lesiones específicas e inespecíficas (infecciones oportunistas, púrpura y equimosis, síndrome de Sweet, etc.). La infiltración de leucocitos neoplásicos en la piel se conoce como leucemia cutis, y es de especial interés el diagnóstico por su implicación pronóstica.
Hemos recogido los casos de leucemia cutis en nuestro servicio entre 1994 y 2014, con un total de 17 pacientes, y hemos evaluado sus características (edad, sexo, historia médica), la morfología de las lesiones y su relación con la enfermedad sistémica.
En nuestra serie la mayoría de los pacientes fueron varones, y la asociación más frecuente fue con leucemia mieloide aguda y se presentó como nódulos o pápulas eritematosas en las extremidades de forma mayoritaria.
Presentamos nuestra experiencia en el diagnóstico y manejo de esta entidad en los últimos 20 años, llamando la atención sobre las características clínicas para un diagnóstico precoz.
Leukemia is defined as a neoplastic proliferation of hematopoietic cells in the bone marrow that subsequently invade peripheral blood and other tissues.
Infiltration of the skin by neoplastic leukocytes is known as leukemia cutis.1 Its frequency ranges from 3% to 30% depending on the type of leukemia,2 and it is more common in children.3,4 The prognosis of leukemia cutis is poor, with a mortality rate of 80% at 1 year after diagnosis.
The term “leukemia cutis” refers to the specific cutaneous manifestations caused by neoplastic cells. However, cutaneous symptoms can also affect patients with leukemia, without there necessarily being a leukemic infiltration. The resulting lesions are known as leukemids (nonspecific cutaneous manifestations).5,6 Leukemids are more frequent than leukemia cutis and present in around 25%–40% of patients during the course of the disease. Leukemia cutis may be secondary to pancytopenia in the bone marrow (mucosal bleeding, pale skin, tendency to develop infections) owing to factors such as adverse reactions to drugs and paraneoplastic syndromes.
Most reports of this condition in dermatology journals are of single cases, with very few case series published to date. Our objective was to present our experience with leukemia cutis and to discuss the clinical and histologic characteristics of this entity.
Material and MethodsWe report the results of a descriptive study of patients with leukemia cutis diagnosed in our department, which belongs to a tertiary dermatology reference center, over a 20-year period (1994–2014). Based on the biopsy samples registered with the diagnosis of leukemia cutis, we collected data from the clinical history, as follows: age, sex, date of diagnosis of cutaneous and systemic disease (where applicable), diagnosis of hematologic disease at the visit, form of presentation, systemic treatment, and outcome. In order to establish the percentage of cases of leukemia cutis in relation to all cases of leukemia diagnosed at our center during the study period, we obtained data on the number of cases of leukemia diagnosed in the hematology department from our hospital database.
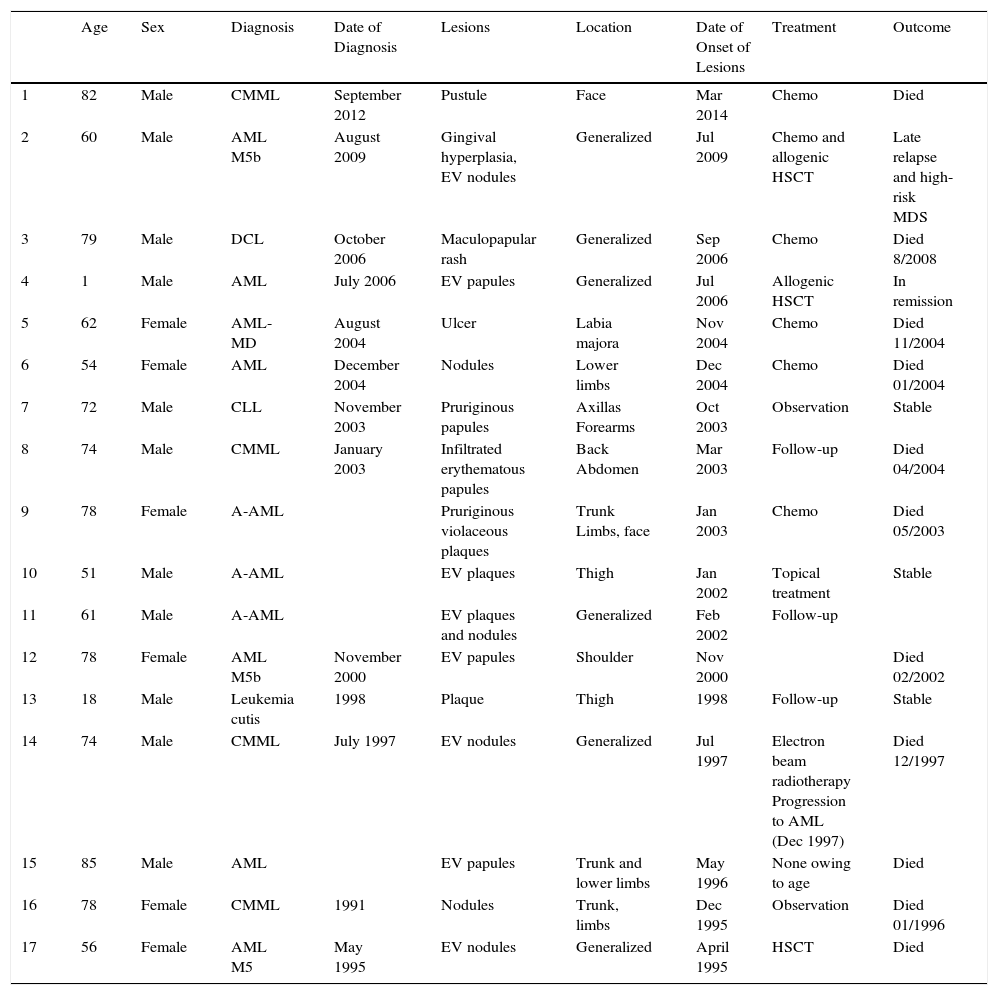
ResultsClinical CharacteristicsThe clinical characteristics are summarized in Table 1. During the study period, a total of 882 cases of leukemia were diagnosed in the hematology department. Of these, 406 were chronic lymphocytic leukemia, 298 were nonspecific leukemia, 66 chronic myelomonocytic leukemia, 58 chronic myeloid leukemia, 49 natural killer cell leukemia, and 5 hairy cell leukemia. During the same period in our department, biopsy specimens were taken from 17 patients diagnosed with leukemia cutis (11 men and 6 women [ratio, 1.83:1]), that is, 1.92% of the total, with a mean age of 62.5 years and a median age of 72 years. As for the hematologic diagnosis, 12 patients had acute leukemia (4 monocytic, 3 myelomonocytic, 1 myelocytic, 1 plasmacytoid dendritic cell neoplasm, and 3 unspecified). The remaining 5 patients had chronic leukemia (4 chronic myelomonocytic leukemia and 1 chronic lymphoid leukemia).
Clinical Characteristics.
| Age | Sex | Diagnosis | Date of Diagnosis | Lesions | Location | Date of Onset of Lesions | Treatment | Outcome | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 82 | Male | CMML | September 2012 | Pustule | Face | Mar 2014 | Chemo | Died |
| 2 | 60 | Male | AML M5b | August 2009 | Gingival hyperplasia, EV nodules | Generalized | Jul 2009 | Chemo and allogenic HSCT | Late relapse and high-risk MDS |
| 3 | 79 | Male | DCL | October 2006 | Maculopapular rash | Generalized | Sep 2006 | Chemo | Died 8/2008 |
| 4 | 1 | Male | AML | July 2006 | EV papules | Generalized | Jul 2006 | Allogenic HSCT | In remission |
| 5 | 62 | Female | AML-MD | August 2004 | Ulcer | Labia majora | Nov 2004 | Chemo | Died 11/2004 |
| 6 | 54 | Female | AML | December 2004 | Nodules | Lower limbs | Dec 2004 | Chemo | Died 01/2004 |
| 7 | 72 | Male | CLL | November 2003 | Pruriginous papules | Axillas Forearms | Oct 2003 | Observation | Stable |
| 8 | 74 | Male | CMML | January 2003 | Infiltrated erythematous papules | Back Abdomen | Mar 2003 | Follow-up | Died 04/2004 |
| 9 | 78 | Female | A-AML | Pruriginous violaceous plaques | Trunk Limbs, face | Jan 2003 | Chemo | Died 05/2003 | |
| 10 | 51 | Male | A-AML | EV plaques | Thigh | Jan 2002 | Topical treatment | Stable | |
| 11 | 61 | Male | A-AML | EV plaques and nodules | Generalized | Feb 2002 | Follow-up | ||
| 12 | 78 | Female | AML M5b | November 2000 | EV papules | Shoulder | Nov 2000 | Died 02/2002 | |
| 13 | 18 | Male | Leukemia cutis | 1998 | Plaque | Thigh | 1998 | Follow-up | Stable |
| 14 | 74 | Male | CMML | July 1997 | EV nodules | Generalized | Jul 1997 | Electron beam radiotherapy Progression to AML (Dec 1997) | Died 12/1997 |
| 15 | 85 | Male | AML | EV papules | Trunk and lower limbs | May 1996 | None owing to age | Died | |
| 16 | 78 | Female | CMML | 1991 | Nodules | Trunk, limbs | Dec 1995 | Observation | Died 01/1996 |
| 17 | 56 | Female | AML M5 | May 1995 | EV nodules | Generalized | April 1995 | HSCT | Died |
A-AML, aleukemic acute myeloid leukemia; AML, acute myeloid leukemia; AML-MD, acute myeloid leukemia, multilinear dysplasia; Chemo, chemotherapy; CLL, chronic lymphoid leukemia; CML, chronic myeloid leukemia; CMML, chronic myelomonocytic leukemia; DCL, dendritic cell leukemia; EV, erythematous-violaceous; HSCT, hematopoietic stem cell transplant; MDS, myelodysplastic syndrome.
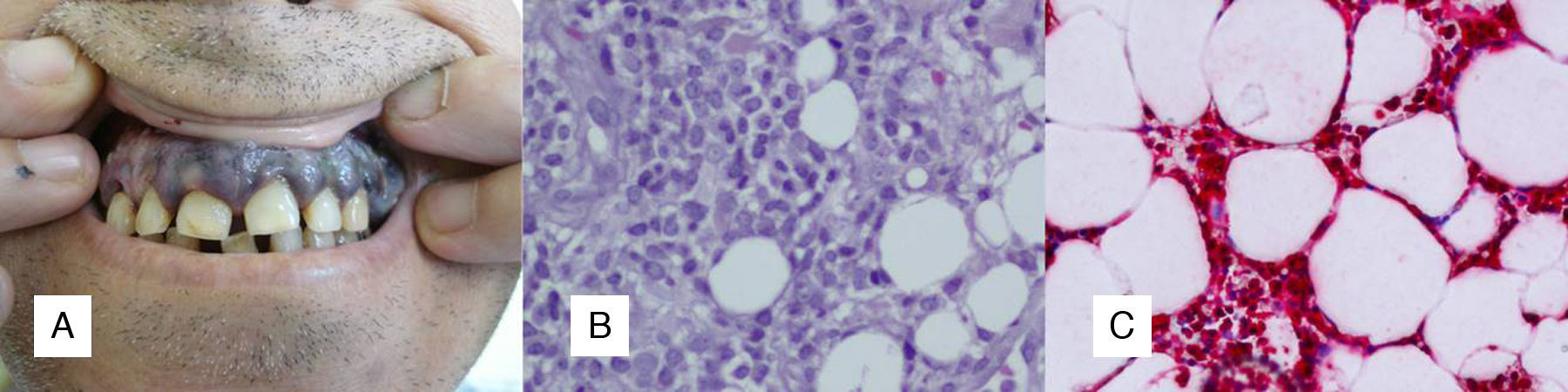
The lesions were located on the limbs in 9 patients, the trunk in 5, the face in 3, and the vulva in 1. The most common presentation was in the form of nodules (7 patients), followed by papules (5 patients) and erythematous-violaceous plaques (4 patients). One of the patients consulted for 2 pustular lesions on the face that were compatible with leukemia cutis (a very unusual presentation) and only 1 patient had gingival hyperplasia, which is characteristic of myelomonocytic leukemia (Fig. 1).
No differences were found for the temporal association with systemic disease, and 5 patients did not have systemic disease (aleukemic leukemia cutis).
Seven patients died during the first year after diagnosis, and 1 was lost to follow-up because he was sent to a hematology reference center for treatment.
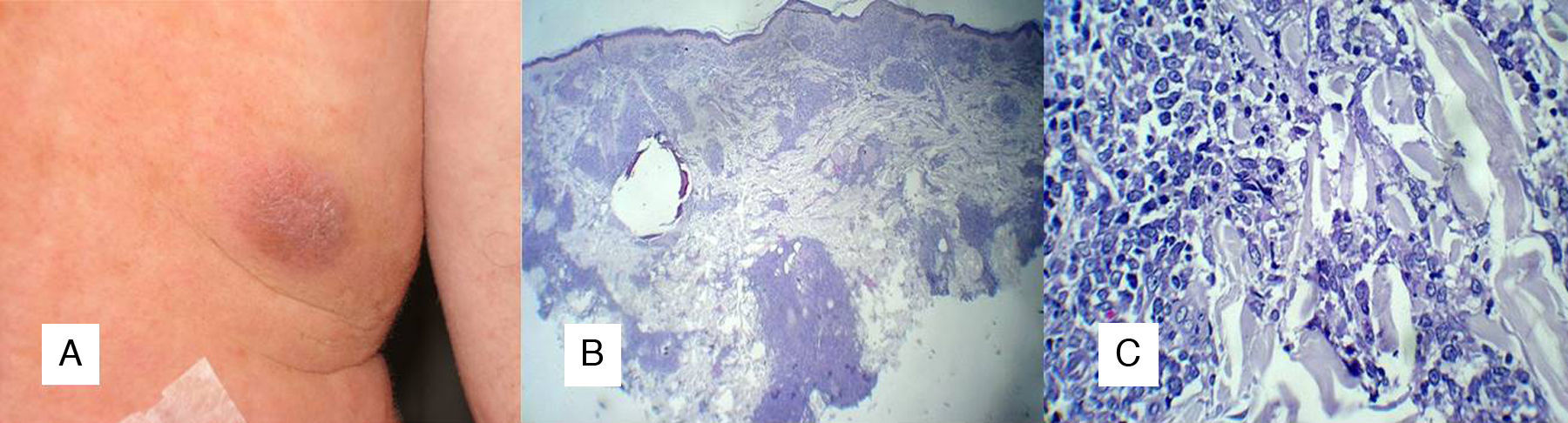
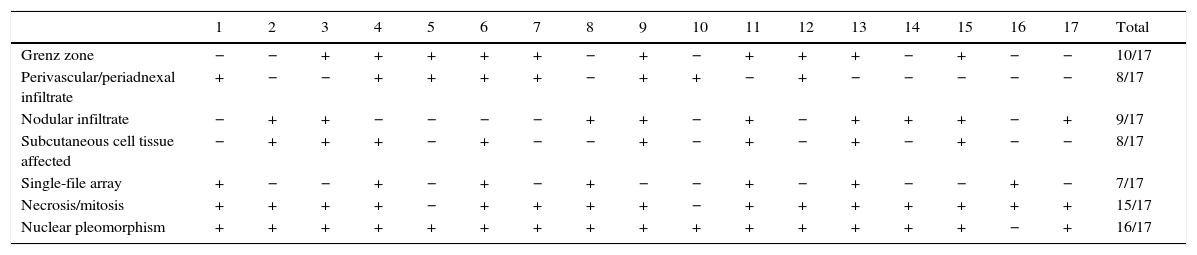
Histologic CharacteristicsAn area of the dermal-epidermal junction (Grenz zone) was spared in 10 lesions, a predominantly perivascular and periadnexal infiltrate was observed in 8 lesions, and a nodular infiltrate occupying the dermis was observed in 9 lesions (Table 2). The subcutaneous cell tissue was affected in 8 cases (Fig. 2). One case, in which the clinical presentation was that of folliculitis, had a cellular infiltrate that was blastic in appearance surrounding and infiltrating the hair follicles. This is the first such finding reported to date. The presence of cells in a single-file array dissecting the collagen fibers in the dermis was only observed in 7 of the 17 cases. Necrotic and mitotic figures and nuclear pleomorphism were observed in almost all samples (16/17).
Histologic Characteristics.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Grenz zone | − | − | + | + | + | + | + | − | + | − | + | + | + | − | + | − | − | 10/17 |
| Perivascular/periadnexal infiltrate | + | − | − | + | + | + | + | − | + | + | − | + | − | − | − | − | − | 8/17 |
| Nodular infiltrate | − | + | + | − | − | − | − | + | + | − | + | − | + | + | + | − | + | 9/17 |
| Subcutaneous cell tissue affected | − | + | + | + | − | + | − | − | + | − | + | − | + | − | + | − | − | 8/17 |
| Single-file array | + | − | − | + | − | + | − | + | − | − | + | − | + | − | − | + | − | 7/17 |
| Necrosis/mitosis | + | + | + | + | − | + | + | + | + | − | + | + | + | + | + | + | + | 15/17 |
| Nuclear pleomorphism | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | − | + | 16/17 |
We compared the histology findings between acute and chronic leukemia. The most common findings in acute disease were a Grenz zone (75% vs 20%), a nodular infiltrate (58% vs 40%), and infiltration of the subcutaneous cell tissue (100% vs 0%); the most common finding in the chronic cases was cells in a single-file array between the collagen bundles (60% vs 33%).
DiscussionBlood stem cells divide into 2 lineages, a myeloid lineage and a lymphoid lineage, from which blood cells develop. Starting from this premise, we can find both types of leukemia in clinical practice. Acute myeloid leukemia is the subtype most frequently observed with leukemia cutis (in up to 10%-15% of cases), mainly acute myelomonocytic and monocytic leukemia. Lymphoid leukemia is much less frequent in the general population, although it can present as a skin disease in up to 5% of cases of chronic lymphoid leukemia, in 25% of cases of prolymphocytic leukemia, and in 20%-70% of cases of mature T-cell leukemia.5–7 The low percentage of patients with leukemia cutis compared with the total percentage of cases of leukemia diagnosed at our center could be due to a loss of patients with cutaneous symptoms, ie, the patient was not referred to the dermatology department, or the patient was referred but no biopsy specimen was taken, or the patient was referred early to a hematology reference center for systemic treatment (ie, before the onset of cutaneous symptoms).
When patients were subclassified, 9 (52%) had acute myeloid leukemia. As for lymphoid neoplasms, 1 patient (5.8%) was diagnosed with chronic lymphoid leukemia. Clinically, the disease presents as nodules (60%), plaques (25%), or erythematous-brownish papules on the lower limbs, followed by the upper limbs, back, scalp, and face5–9; these findings are consistent with those we observed. Although we were unable to find differences in the temporal association with systemic disease, the literature we reviewed shows that in most cases the lesions appear after the blood disease is diagnosed, although they may appear concomitantly in 30% of cases or previously in at least 10% (aleukemic leukemia cutis).10,11 Extramedullary involvement is already present in most cases (mainly at the level of the central nervous system) when the cutaneous symptoms appear, and this is generally indicative of poor prognosis. In our study, 7 patients (41.17%) died within the first year after diagnosis. As for chronic lymphoid leukemia, the onset of cutaneous symptoms could be associated with Richter syndrome, although this condition was not observed in the only patient with chronic lymphoid leukemia in our study.12
Histopathology generally reveals the presence of a Grenz zone at the dermal-epidermal junction. This usually appears in the form of a predominantly perivascular and periadnexal or nodular infiltrate that affects the subcutaneous cell tissue, groups of cells in a single-file array dissecting the collagen bundles, and numerous mitotic figures and necrotic cells in the infiltrate. In our series, we observed greater involvement of the subcutaneous cell tissue in acute leukemia than in chronic leukemia, a finding that was not observed in the literature. The cytological characteristics vary with the type of leukemia. For example, in acute lymphoid leukemia, we find large lymphoblasts with scant cytoplasm and pleomorphic nuclei, whereas in chronic lymphoid leukemia we find small basophilic lymphocytes in a monomorphic infiltrate.5,6,12–14
Immunohistochemistry shows the myeloid neoplasms to be positive for myeloperoxidase and lysozyme, whereas in lymphoid neoplasms, staining for lysozyme is negative, and the neoplasms gradually lose their positivity for myeloperoxidase and terminal deoxynucleotidyl transferase as the cells mature.5,14
Finally, the treatment of leukemia cutis is that of the systemic disease. Similarly, de novo hematologic neoplasms have been reported in association with chemotherapy.15 We did not observe an association with previous therapy in any cases.
ConclusionsWe present a series of cases of leukemia cutis and describe the specific clinical and histologic characteristics of the disease, bearing in mind that this condition is unusual in routine clinical practice and in patients with leukemia. We believe it is important to disseminate our findings, since the clinical presentation of the disease is very varied and diagnosis should be based not only on macroscopic findings, but also on the results of additional tests and histopathology. The characteristic findings in histopathology are cells with a blastic appearance and nuclear pleomorphism, mitosis, and necrosis that dissect collagen fibers in a single-file array, with involvement of the subcutaneous cell tissue (mainly in the acute forms). The study is limited mainly by its retrospective design and the small percentage of patients with a histologic diagnosis of leukemia cutis compared with the total number of cases diagnosed in our center. New prospective studies with larger populations are warranted to define the clinical and histopathological characteristics and to study in depth the pathogenic mechanisms of leukemia cutis.
Ethical DisclosuresProtection of humans and animalsThe authors declare that no tests were carried out in humans or animals for the purposes of this study.
Confidentiality of dataThe authors declare that they have followed their insitutional protocols on publication of patient data.
Right to privacy and informed consentThe authors declare that no private patient data appear in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Martínez-Leboráns L, Victoria-Martínez AM, Torregrosa-Calatayud JL, Miquel VAd. Leucemia cutis. Serie de 17 casos y revisión de la literatura. Actas Dermosifiliogr. 2016;107:e65–e69.