The patient was an asymptomatic 58-year-old woman with no history of interest who consulted for an erythematous-purpuric plaque measuring 2cm at its maximum diameter on the right forearm that had appeared 4 months previously.
Physical ExaminationPhysical examination revealed an erythematous-purpuric plaque with a rough surface, elastic consistency, and slightly irregular borders on the extensor aspect of the right forearm (Fig. 1).
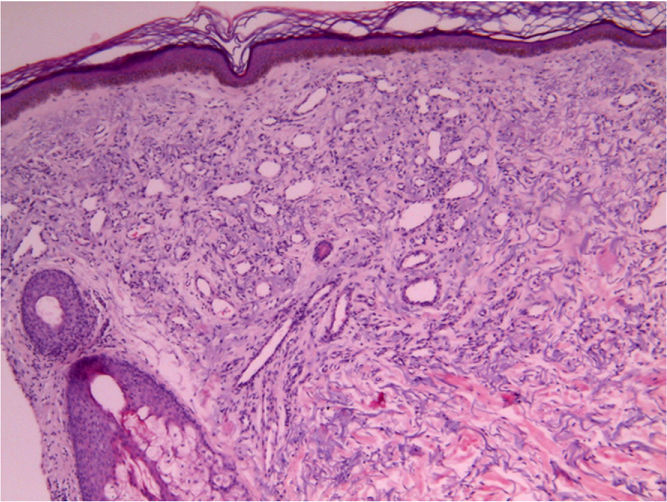
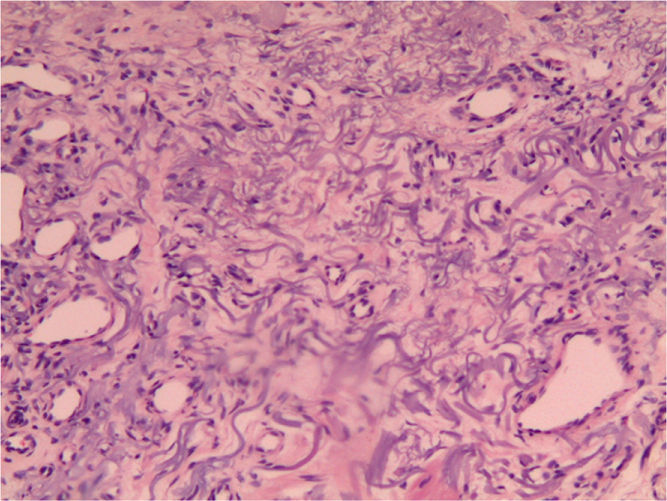
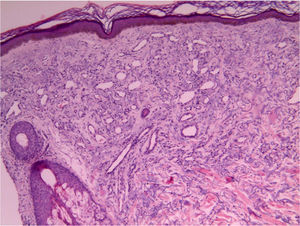
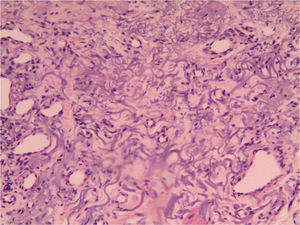
HistopathologyExamination of a biopsy specimen from the center of the lesion revealed an epidermis with no significant histologic abnormalities and hyperpigmentation in the stratum basale. Below the epidermis, a fibrous band of superficial dermis acted as a border against a proliferation of small-caliber venous vessels running parallel to the epidermis that occupied the upper third of the reticular dermis (Fig. 2). The vessels had oval lumina (some of which were collapsed) covered by a simple endothelium without atypia, mitotic figures, or intraluminal projections. The dermis surrounding the vessels showed intense elastotic degeneration, and the elastic fibers took the form of irregular arabesques with pointed ends (Fig. 3). The adnexa were displaced by the vascular proliferation. All the vessels stained positive for the immunohistochemical marker CD34, thus facilitating visualization of some vascular walls, which were slightly collapsed, with respect to the degenerated elastic fibers.
What Is Your Diagnosis?
DiagnosisAcquired elastotic hemangioma.
Clinical Course and TreatmentThe lesion was removed by simple excision, with no signs of recurrence at 1 year.
CommentAcquired elastotic hemangioma was first reported by Requena et al.1 in 2002. This benign acquired vascular lesion grows in the form of a plaque that is not always angiomatous in appearance. Consequently, clinical opinions on the lesion are somewhat heterogeneous. Given the clinical characteristics of the lesion in the case we report, the various diagnoses proposed included neutrophilic dermatosis and granuloma annulare, although the lesion was angiomatous in appearance, thus indicating the possibility of Kaposi sarcoma or another type of hemangioma.
The lesion is found mainly on photoexposed areas and is composed of a proliferation of small-caliber vessels arranged in the form of a band running parallel to the epidermis, from which it is separated by a homogeneous collagen band. The vessels, whose lumina may be open or collapsed, can present a prominent endothelium, without atypia, mitosis, or intraluminal projections.2–5 The dermis always shows intense actinic damage, and elastic fibers twisted in the form of arabesques are common. The vessels stain positive for endothelial markers such as CD34 and CD31. Positivity for podoplanin indicates that the vessels are lymphatic in origin, although in the case we report, there were, at least focally, vascular structures whose morphology was compatible with venous vessels (consistent with the observations of Tong and Beer6).
Once the vascular nature of the lesion has been confirmed, a differential diagnosis should be made with other conditions characterized by proliferation of small vessels. Histopathology rules out Kaposi sarcoma and other spindle-cell vascular tumors. In clinical terms, the lesion is not compatible with cherry hemangioma or hobnail hemangioma.
There continues to be some debate as to whether the lesion is hyperplastic or neoplastic, and the low number of cases reported in the literature contributes to this situation.
The treatment of choice is simple excision, with no relapses reported to date.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Torres Gómez FJ, Fernández Machín P, Neila Iglesias J. Placa eritematopurpúrica asintomática en antebrazo. Actas Dermosifiliogr. 2016;107:771–772.