A 24-year-old woman with no medical history of interest presented with a 4-month history of asymptomatic lesions in the axillas. She first noticed the lesions after 3 sessions of hair removal using intense pulsed light.
Physical ExaminationPhysical examination revealed abundant tiny follicular flesh-colored to yellowish papules clustered symmetrically in both axillas (Fig. 1).
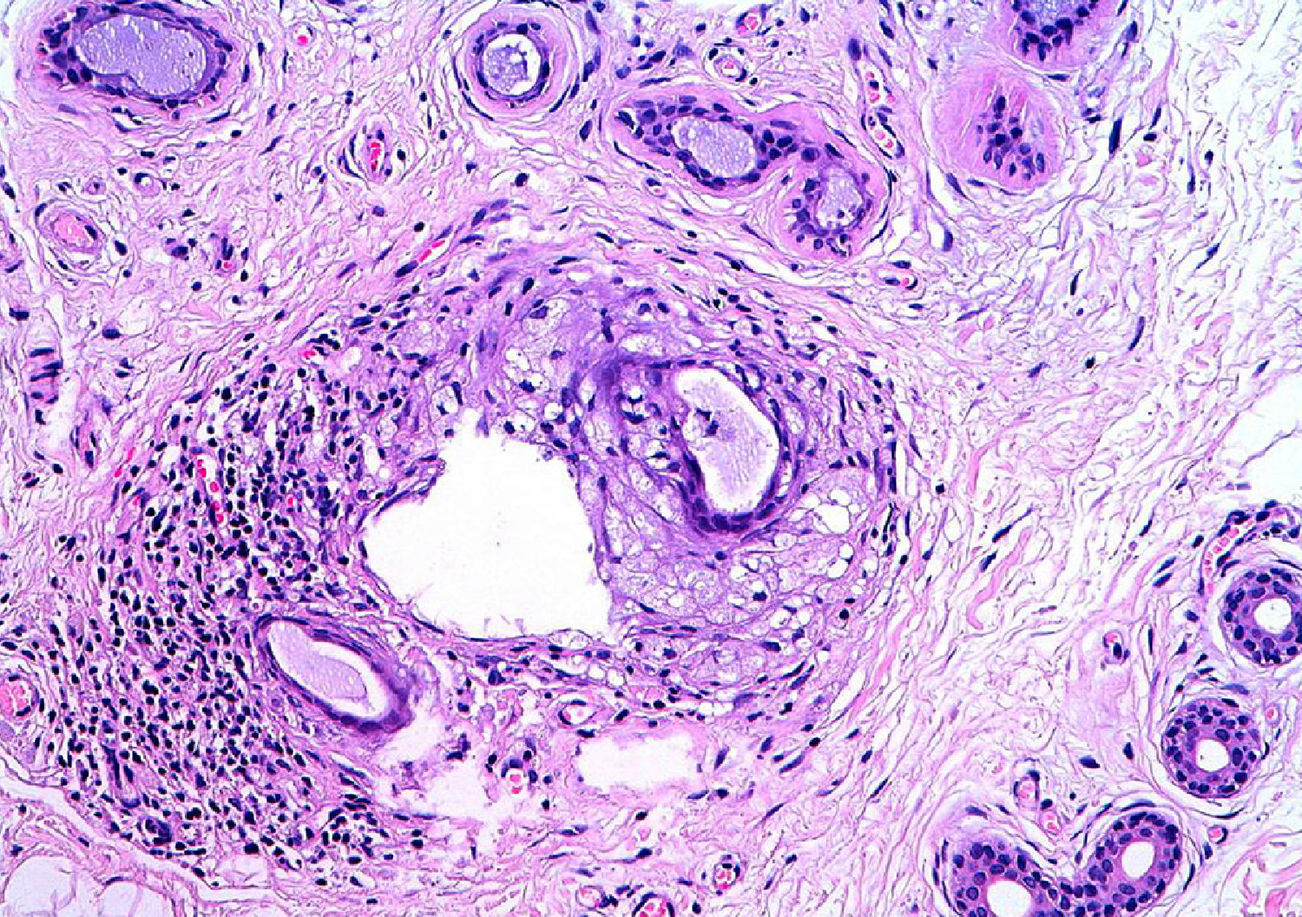
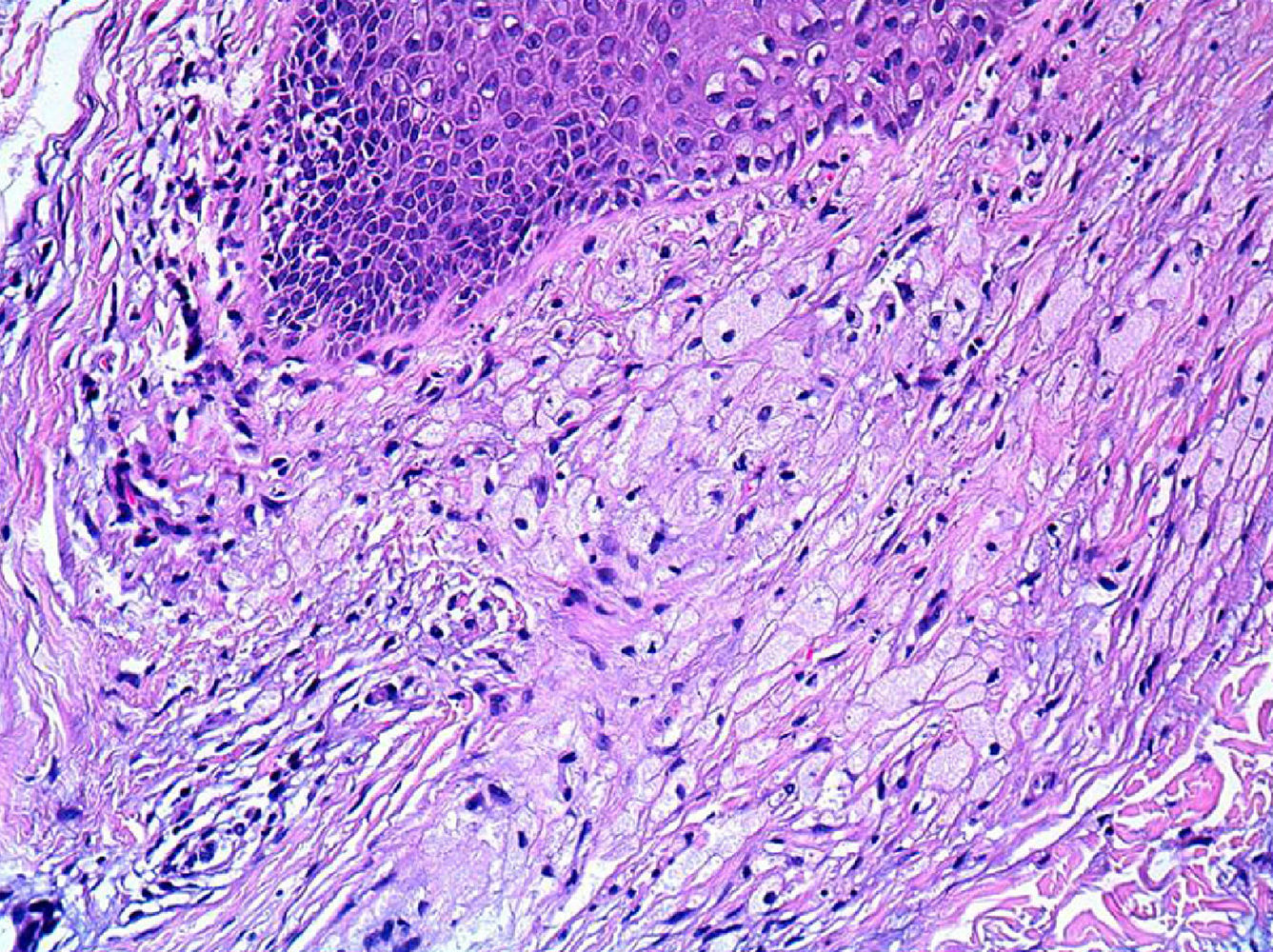
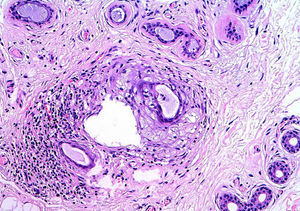
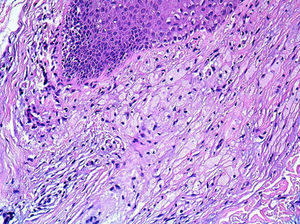
HistopathologySkin biopsy revealed apocrine glands with dilated ducts surrounded by an inflammatory infiltrate similar to that located around the follicular infundibulum (Fig. 2). The inflammatory infiltrate was composed mainly of cells with abundant, clear cytoplasm and microscopic lipid granules corresponding to xanthomatous histiocytes and is known as perifollicular xanthomatosis (Fig. 3). Spongiosis was observed in the excretory duct of the apocrine gland, and a keratotic plug was observed in the follicular infundibulum.
What Is Your Diagnosis?
DiagnosisFox-Fordyce disease after hair removal using intense pulsed light.
Clinical Course and TreatmentThe patient received tretinoin 0.05% cream, which was applied before bedtime. Her condition improved but did not resolve completely.
DiscussionFox-Fordyce disease, or apocrine miliaria, is a rare condition that was described by Fox and Fordyce in 1902. It is characterized by chronic abnormality of the apocrine sweat glands. Clinically, it manifests as symmetrical tiny flesh-colored or yellowish papules at the sites of the apocrine glands, such as the axillas, the mammary areolas, the anogenital area, and the umbilical area.1 It mainly affects postpubertal women, and the symptoms tend to resolve with the menopause, oral contraceptives, and pregnancy. It is caused by abnormal keratinization in the infundibulum, which is followed by obstruction of the apocrine duct and dilation of the apocrine gland. The disease is thought to be associated with hormonal and mechanical factors.
Three cases of axillary Fox-Fordyce disease caused by laser hair removal have been reported in recent years.2–4 Hair removal systems—both laser and intense pulsed light—are based on the phenomenon of selective photothermolysis, in which the melanin in the hair follicle absorbs the light emitted and converts it to heat, with the consequent damage to the tissue of the follicle and hair loss. The narrow temporal association between these hair removal mechanisms and onset of Fox-Fordyce disease indicates that the procedure can damage the follicular infundibulum, thus affecting maturation of infundibular keratinocytes and triggering pathogenesis.
The histopathologic characteristics of Fox-Fordyce disease are very varied and include traditional findings such as dilation and hyperkeratosis of the follicular infundibulum, spongiosis of the infundibular epithelium, and periadnexal histiocytic and lymphocytic infiltrate. More recently described findings include perifollicular xanthomatosis, which is defined as a clearly consistent and specific marker of Fox-Fordyce disease,5,6 especially in the axillas. Perifollicular xanthomatosis is caused by follicular obstruction leading to retention and subsequent extravasation of lipid-rich apocrine material, which is then phagocytosed by macrophages; hence the resultant xanthomatous appearance. The presence of perifollicular foamy macrophages contributes to the elevation of the lesions and gives them their characteristic yellowish coloring.
Treatment of Fox-Fordyce disease is generally unsatisfactory. The treatments proposed include topical and intralesional corticosteroids, topical and systemic retinoids, topical antibiotics (eg, clindamycin), oral contraceptives, topical pimecrolimus, and a modified liposuction technique in the most refractory cases.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Alés-Fernández M, Ortega-Martínez de Victoria L, García-Fernández de Villalta MJ. Lesiones axilares después de tratamiento de depilación con luz pulsada intensa. Actas Dermosifiliogr. 2015;106:61–62.