Extramammary Paget disease (EMPD) is a very rare form of intraepithelial adenocarcinoma. We report the cases of EMPD diagnosed in a referral hospital over a 5-year period from 2009 to 2013. Ten cases of EMPD were diagnosed in 4 men and 6 women aged between 50 and 79 years. Erroneous clinical diagnoses led to diagnostic delays of 1 to 5 years in all cases. Six patients had in situ lesions and dermal invasion was observed in the other 4 cases. Four patients had a second neoplasm and 2 of the patients with invasive EMPD died. Because EMPD is rare and its clinical presentation is nonspecific, a high degree of clinical suspicion is required to avoid delays in diagnosis and treatment.
La enfermedad de Paget extramamaria (EPEM) es una forma extremadamente rara de adenocarcinoma intraepitelial. Presentamos los casos de EPEM diagnosticados en los últimos 5 años en un hospital de referencia (2009-2013). Se trata de 10 casos, 4 varones y 6 mujeres, con edades comprendidas entre los 50-79 años. Todos ellos sufrieron un retraso diagnóstico de uno a 5 años debido a sospechas diagnósticas erróneas. Seis casos correspondieron a EPEM in situ y en 4 existía invasión dérmica. Existió una segunda neoplasia en 4 pacientes y 2 con EPEM invasiva fallecieron. La baja incidencia de esta enfermedad y su clínica inespecífica nos debe alertar sobre la necesidad de establecer una alta sospecha clínica para evitar retrasos diagnósticos y terapéuticos.
Extramammary Paget disease (EMPD) was first described by Crocker in 1889 as a localized carcinoma affecting the penis and scrotum in a 60-year-old goldsmith. The symptoms and histopathological characteristics were similar to those of mammary Paget disease, first described by James Paget in 1874.1 The disease is an extremely rare form of intraepithelial adenocarcinoma that may be accompanied by other malignant neoplasms.2 We report all cases of EMPD diagnosed during a 5-year period at a tertiary referral hospital.
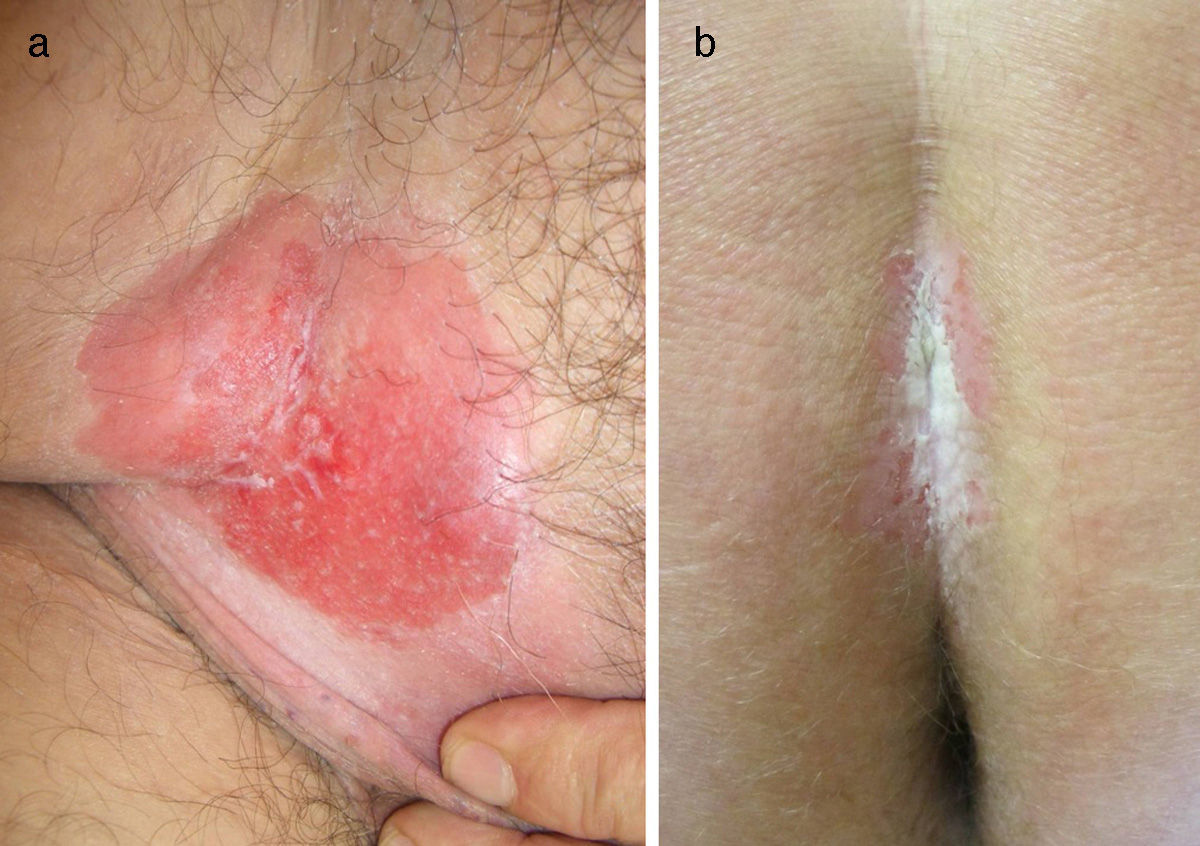
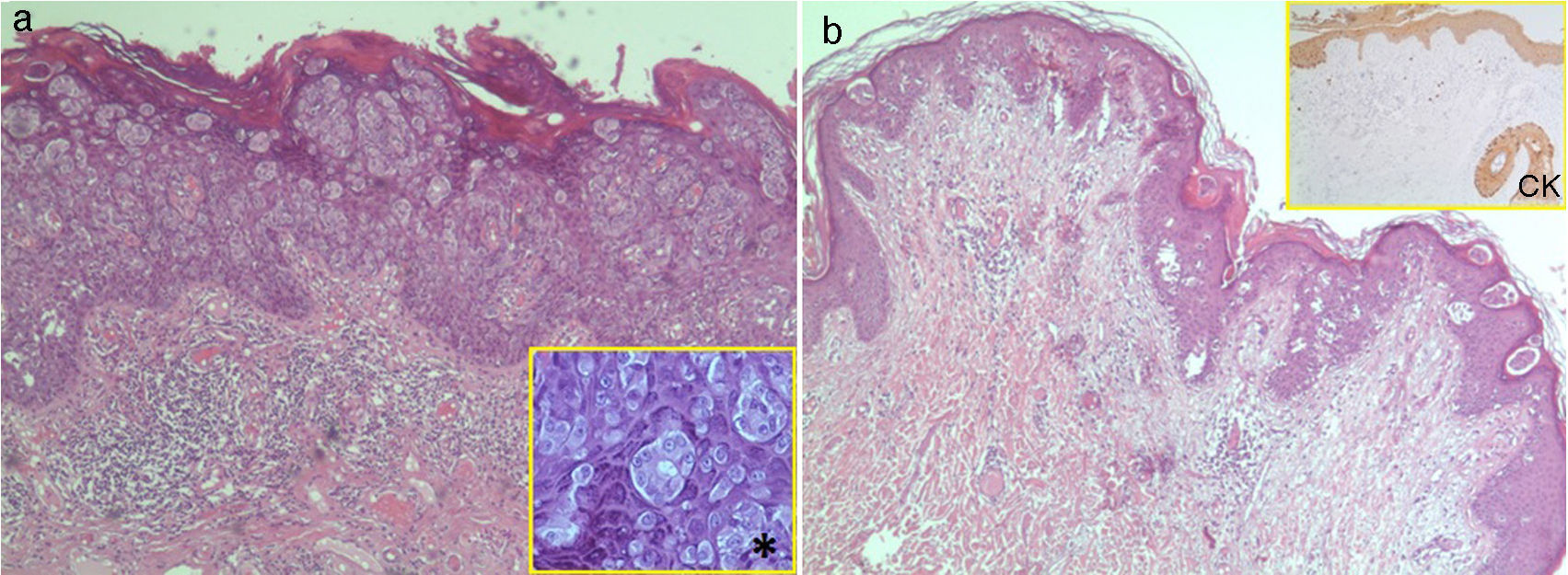
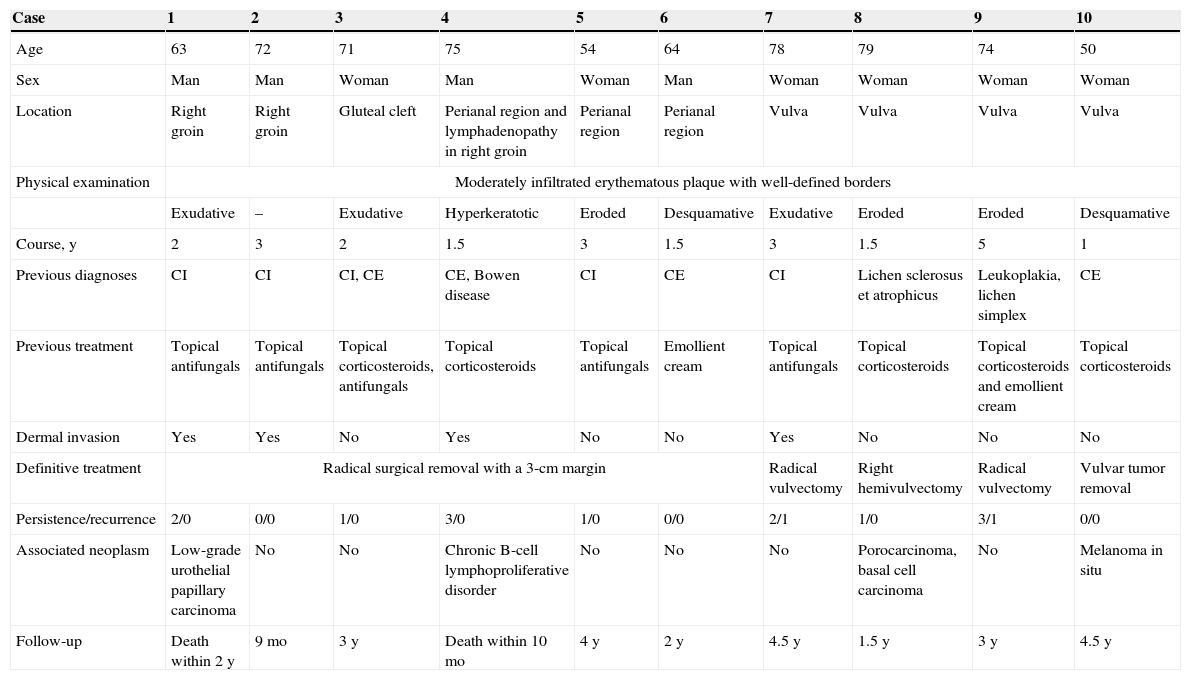
Case DescriptionsThe clinical and histologic characteristics of patients with EMPD are summarized in Table 1. We recorded 10 cases (4 on the vulva, 3 in the perianal region, 2 on the right groin [Fig. 1A], and 1 on the gluteal cleft [Fig. 1B]) in 4 men and 6 women aged between 50 and 79 years. In all cases there was a diagnostic delay of between 1 and 5 years, and the patients received treatment that was ineffective for fungal infections in 5 cases (50%), chronic inflammatory disease (eczema and lichen simplex) in 5 cases (50%), Bowen disease in 1 case (10%), lichen sclerosus et atrophicus in 1 case (10%), and leukoplakia in 1 case (10%). The diagnosis of EMPD was confirmed in all cases by histopathologic study of the skin biopsy, and treatment was by radical removal of the lesion with wide margins. EMPD was in situ in 6 patients (60%) (Fig. 2A), and dermal invasion was detected in 4 patients (40%) (Fig. 2B). The disease persisted after surgery in 4 patients (66.7%) with EMPD in situ and in 3 patients (75%) with invasive disease. In addition, recurrence was detected in 1 case of EMPD in situ (16.7%) and in 1 case of invasive EMPD (25%); further surgery was necessary in both cases. A second neoplasm was detected in 4 patients: 2 (33.3%) with EMPD in situ had melanoma in situ (1 patient) and porocarcinoma and basal cell carcinoma (1 patient); 1 patient (25%) with invasive disease had chronic B-cell lymphoproliferative disorder; and 1 patient (25%) had low-grade papillary urothelial carcinoma. Two patients (20%), both with the invasive form, died from metastasized disease, one at 10 months and the other at 2 years. In the remaining 8 patients (80%), no recurrence was observed during a follow-up period ranging from 9 months to 4.5 years.
Clinical and Histologic Characteristics of Patients With Extramammary Paget Disease.
| Case | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Age | 63 | 72 | 71 | 75 | 54 | 64 | 78 | 79 | 74 | 50 |
| Sex | Man | Man | Woman | Man | Woman | Man | Woman | Woman | Woman | Woman |
| Location | Right groin | Right groin | Gluteal cleft | Perianal region and lymphadenopathy in right groin | Perianal region | Perianal region | Vulva | Vulva | Vulva | Vulva |
| Physical examination | Moderately infiltrated erythematous plaque with well-defined borders | |||||||||
| Exudative | – | Exudative | Hyperkeratotic | Eroded | Desquamative | Exudative | Eroded | Eroded | Desquamative | |
| Course, y | 2 | 3 | 2 | 1.5 | 3 | 1.5 | 3 | 1.5 | 5 | 1 |
| Previous diagnoses | CI | CI | CI, CE | CE, Bowen disease | CI | CE | CI | Lichen sclerosus et atrophicus | Leukoplakia, lichen simplex | CE |
| Previous treatment | Topical antifungals | Topical antifungals | Topical corticosteroids, antifungals | Topical corticosteroids | Topical antifungals | Emollient cream | Topical antifungals | Topical corticosteroids | Topical corticosteroids and emollient cream | Topical corticosteroids |
| Dermal invasion | Yes | Yes | No | Yes | No | No | Yes | No | No | No |
| Definitive treatment | Radical surgical removal with a 3-cm margin | Radical vulvectomy | Right hemivulvectomy | Radical vulvectomy | Vulvar tumor removal | |||||
| Persistence/recurrence | 2/0 | 0/0 | 1/0 | 3/0 | 1/0 | 0/0 | 2/1 | 1/0 | 3/1 | 0/0 |
| Associated neoplasm | Low-grade urothelial papillary carcinoma | No | No | Chronic B-cell lymphoproliferative disorder | No | No | No | Porocarcinoma, basal cell carcinoma | No | Melanoma in situ |
| Follow-up | Death within 2 y | 9 mo | 3 y | Death within 10 mo | 4 y | 2 y | 4.5 y | 1.5 y | 3 y | 4.5 y |
Abbreviations: CE, chronic eczema; CI, candidal intertrigo.
A, Case 1: Erythematous, exudative plaque measuring 10×12cm, with moderate infiltration and well-defined borders on the right groin corresponding to invasive extramammary Paget disease. B, Case 3: Erythematous plaque with a whitish exudate measuring 6×4cm, moderate infiltration, and well-defined borders in the gluteal cleft corresponding to extramammary Paget disease in situ.
A, Case 9: infiltration of the epidermis with no involvement of the dermis by cells with abundant, eosinophilic cytoplasm and evident nucleoli (Paget cells) grouped in nests (hematoxylin-eosin, original magnification ×4). *Occasional formation of small glands (×20). B, Case 2: presence of Paget cells in the epidermis and dermis (hematoxylin-eosin, original magnification ×4). CK immunostaining with low- and high-molecular-weight keratins (AE1 and AE3) showing positivity in the epidermis, follicular epithelium, and (more intense) in Paget cells, with invasion of the reticular dermis by individual cells and small groups of cells (×4). CK indicates cytokeratin.
Hospital Universitario Virgen de las Nieves, Granada, Spain is a tertiary referral hospital serving a population of 439 035 people, among whom 10 patients were diagnosed with EMPD from 2009 to 2013. EMPD is a very infrequent neoplasm whose exact incidence is unknown, although it accounts for no more than 6.5% of all Paget diseases and only a few hundred cases have been published in the literature.2–4 EMPD generally affects whites aged between 50 and 80 years, mainly women at a ratio of 2.4:1, as in our series, although in Asians it usually affects men.5–7 There are 2 theories on the origin of EMPD. According to the first, EMPD is considered an abnormal differentiation of the epidermal cells of the basal layer (primary EMPD); therefore, Paget disease would be considered an adenocarcinoma that is independent of a second neoplasm. According to the second theory, EMPD is an epidermal metastasis of an underlying carcinoma (secondary EMPD), although solitary lesions would remain unexplained.6,8 At least 6 cases of familial EMPD have been identified.6 The clinical symptoms are insidious and often minor in the initial stages, with the result that patients do not request medical care until several years have passed, thus delaying diagnosis and treatment for a mean period of 2 years.2,9 The lesions consist of infiltrated brownish or erythematous plaques that are generally solitary with well-defined borders. They are occasionally edematous and exudative and can cause pruritus, pain, and a burning sensation. They may also be asymptomatic (Fig. 1).4 The surface is sometimes rough, and there may be erosions, crusts, or lichenification.6 The lesions rarely present as infiltrated nodules, vegetating lesions, or locoregional lymphadenopathies.9 Unlike mammary Paget disease, EMPD is associated with underlying adnexal carcinoma in 24%-33% of cases and visceral cancer in 12%-15% of cases, including tumors of the gastrointestinal tract and urinary tract, mainly in organs with a contiguous lining and more commonly in the perianal region.6,10 Associated tumors generally include those affecting the breast, bladder, and cervix, although they can also affect the rectum, colon, prostate, ovaries, urethra, vagina, endometrium, and kidneys.6 We observed an association with skin cancer in 2 cases, one with urothelial involvement and the other with hematologic involvement. The neoplasm is found mainly at sites rich in apocrine glands, such as the external genitalia, the perianal region, the groin, and the axillas,2,3 although it can also be found anywhere on the skin or mucosae.7 The most common site is the vulva (65%), as in the cases we report, although this figure only represents 2% of all primary vulvar tumors.4,9 The second most common site is the perianal region (20%), and the third is the male genitalia (14%).4,9 Exceptionally, the tumor is found in the axillas or groin, as in 2 of the cases reported here, in which the disease was invasive, probably because the atypical location of the lesion meant that diagnosis was delayed.4,9 Since this neoplasm is rare, there is no established protocol for its diagnosis, treatment, and follow-up, thus making it a challenge in clinical practice.7 Diagnosis is based on symptoms and histopathology. Skin biopsy reveals cells with an abundant, pale cytoplasm, large pleomorphic nuclei, and, occasionally prominent nucleoli; the nuclei are sometimes eccentric and resemble signet rings (Fig. 2).6 The differential diagnosis should include more common diseases such as eczematous lesions, lichen simplex chronicus, lichen sclerosus et atrophicus, lichen planus, inverse psoriasis, candidal intertrigo, erythroplasia of Queyrat, Bowen disease, superficial spreading amelanotic melanoma, and familial benign pemphigus.4,6 The treatment of choice is extensive surgical removal, although the disseminated nature and poorly defined margins of this tumor lead to recurrence in 16%-44% of cases11; therefore, Mohs micrographic surgery is increasingly used and can reduce the recurrence rate to 8%-28%.2,6 At our center, local persistence after surgery was recorded in 7 cases (70%) and recurrence in 2 (20%). Alternative approaches include carbon dioxide laser treatment, topical imiquimod, cryotherapy, radiotherapy, and photodynamic therapy, although the recurrence rate is very high (50%-60%).2,4,12,13 Systemic chemotherapy with 5-fluorouracil, mitomycin C, docetaxel, and etoposide is used in inoperable cases, although few complete responses have been achieved.4,5,9 During the EMPD workup, every attempt should be made to rule out associated neoplasms and identify signs of recurrence, which affects up to 35% of patients with EMPD in situ and 67% of invasive cases.2 Screening for associated neoplasms should include gynecologic and abdominal ultrasound, colonoscopy, and mammography. EMPD remains in situ in more than 65% of cases, as with the patients in the present study, in whom the survival rate was greater than 90% at 5 years and spontaneous regression was occasionally observed after partial surgical removal.4,6 Survival decreases dramatically in invasive disease or in the presence of associated tumors, as in the 2 patients who died in the present series. The low incidence of this disease and its nonspecific clinical picture should alert us to the need for high clinical suspicion in order to avoid delays in diagnosis and therapy, which can worsen the prognosis in these patients.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Blasco-Morente G, Martín-Castro A, Garrido-Colmenero C, Tercedor-Sánchez J. Enfermedad de Paget extramamaria: 10 casos. Actas Dermosifiliogr. 2015;106:61–65.