Indeterminate cell histiocytosis (ICH) is a rare disease characterized by a proliferation of histiocytes with a mixed immunohistochemical phenotype between Langerhans cells and non-Langerhans histiocytes. The behavior of the disease varies from exclusively cutaneous forms with a chronic benign or self-resolving clinical course to fulminant acute systemic forms.
We present the case of a girl aged 16 months, with no personal or family history of interest. She was seen in outpatients for facial lesions that had appearance rapidly 15 days earlier and had not improved with amoxicillin–clavulanic acid, which was prescribed by her health area pediatrician because of the sudden onset of the condition. No manifestations of any associated disease were detected in the medical history. Physical examination revealed multiple erythematous-orange papules with an erythematous halo, some showing pseudovesiculation, umbilication, and the formation of a central scab (Fig. 1A). The lesions mainly affected the face and there were no palpable lymph nodes. A smear was taken from the lesions for direct microscopy, microbiological culture, and polymerase chain reaction for varicella-zoster virus and coxsackieviruses. The results were normal or negative. A week later, all the lesions persisted in their papular phase, with the additional appearance of yellow-orange papules on the forearms and root of the limbs (Fig. 1, B and C). The patient remained in a good general state of health. With a suspected diagnosis of benign cephalic, generalized eruptive, or Langerhans cell histiocytosis (LCH), skin biopsy was taken from a lesion on the right forearm. Histology revealed an ulcerated epidermis with an infiltrate formed mainly of mononuclear and histiocytoid cells, accompanied by lymphocytes and occasional eosinophils, affecting the papillary dermis and deep dermis, where histiocytic nodules were observed (Fig. 2). Immunohistochemistry was intensely and diffusely positive for CD1a both in the epidermis and in the dermal nodules, with clear and intense but more scattered positivity for CD68 and S100 in the epidermis, interstitial dermis, and in the histiocytic nodules. In contrast, langerin (CD207) was positive in the epidermal control sample, and very focally, practically negative, in the interstitial dermis and dermal nodules. Based on these findings we made a diagnosis of ICH (Fig. 3). The workup was completed with blood biochemistry, complete blood count, plasma osmolarity, and urinary sediment, together with abdominal ultrasound, and x-rays of the chest, cranial vault, and vertebral column. The additional tests were within normal limits. After 2 months of follow-up, and on treatment with only topical methylprednisolone, the facial lesions started to resolve. However, bullous lesions appeared on the forearms and hands (Fig. 1D), obliging us to start systemic corticosteroid treatment, which achieved good control of the new lesions. At the time of writing, no systemic complications have developed, but the patient has required a low maintenance dose of oral corticosteroids to prevent outbreaks of vesicular-bullous lesions on the trunk and limbs, and periodic follow-up has been continued due to the possibility of developing associated hematologic tumors or extracutaneous, multiorgan forms of her disease.
A, Erythematous-orange papules, some of which are umbilicated and show pseudovesiculation and the presence of scabs. B and C, A week later, all the lesions were in the papular phase, and yellow-orange papules had appeared on the forearms. D, Bullous lesions on the hands 2 months after onset of the condition.
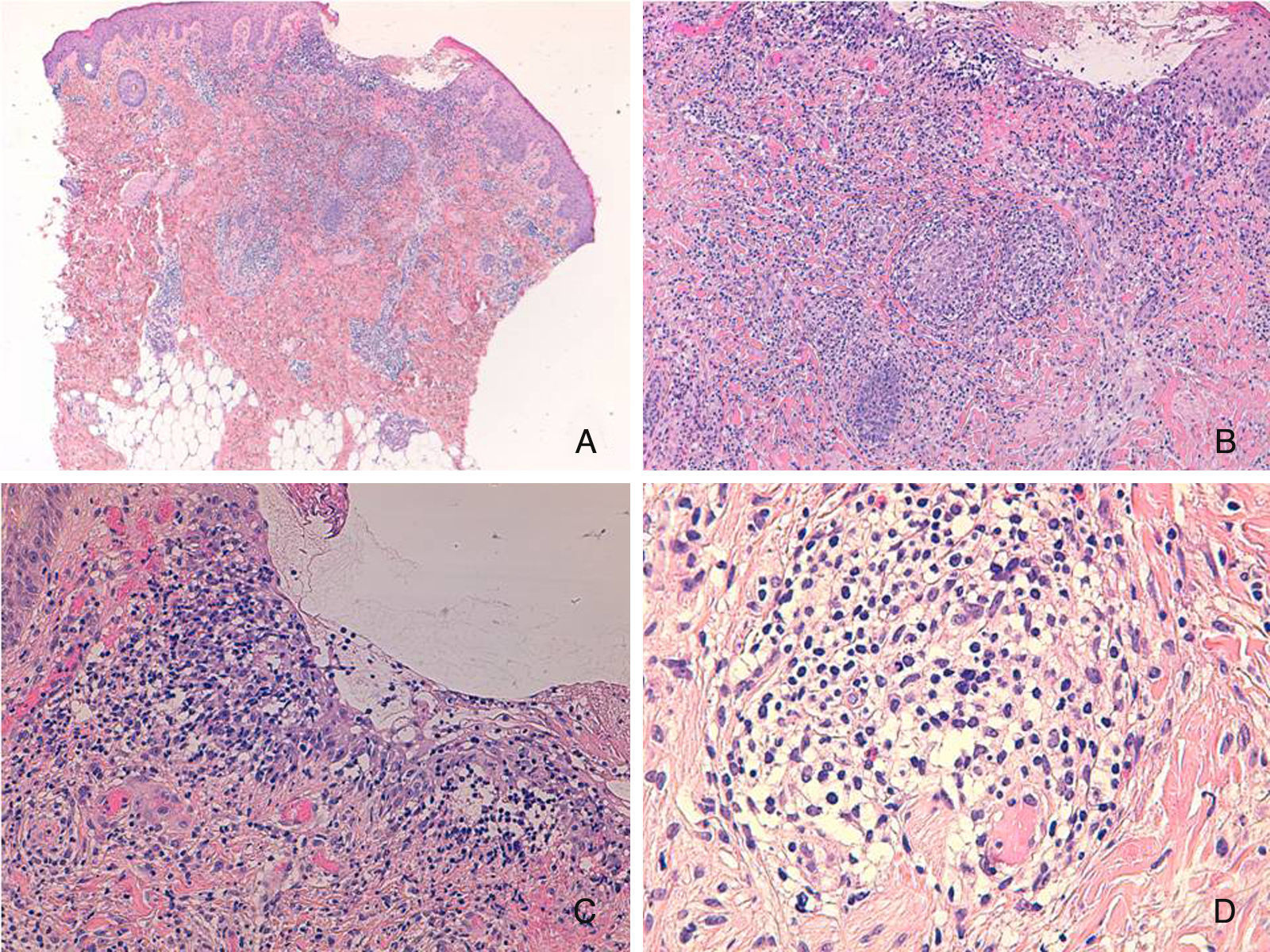
Ulcerated epidermis with a nodular superficial and deep dermal infiltrate, with a predominance of mononuclear histiocytes accompanied by lymphocytes and eosinophils. A, Hematoxylin and eosin (H&E), original magnification×40. B, H&E, original magnification×100; C, H&E, original magnification×200; D, Detail of a nodule. H&E, original magnification×400.
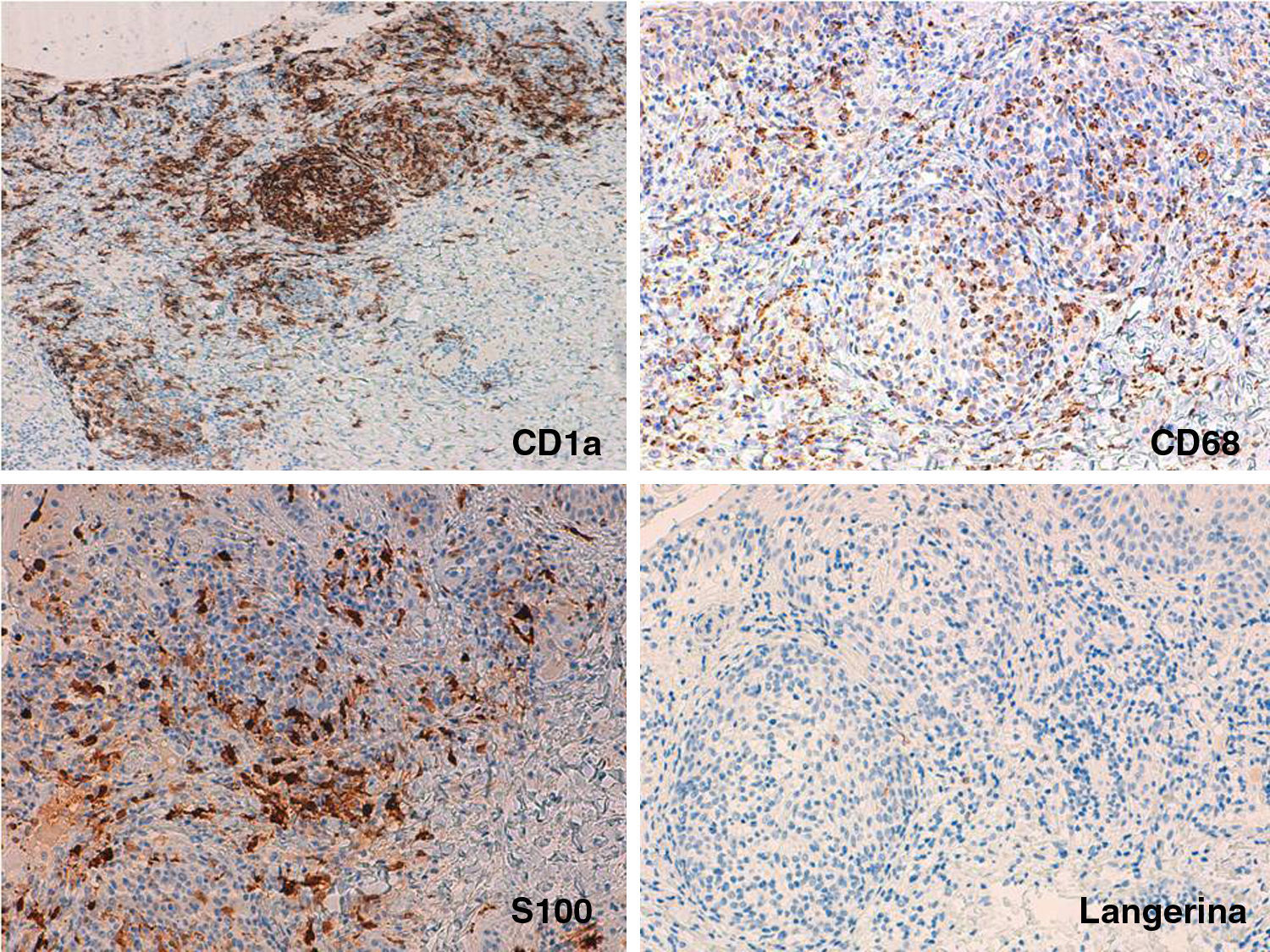
Immunohistochemistry: A, Extensive and diffuse positivity for CD1a. Original magnification×100. B and C, Detail of the nodules showing scattered but extensive positivity for CD68 and S100 in the epidermis, interstitial dermis, and dermal nodules. Original magnification×200. D, Detail of the nodules showing weak positivity for langerin in the same areas that were positive for CD1a, CD68, and S100. Original magnification×200.
The histiocytoses are a heterogeneous group of disorders whose common feature is an excessive proliferation of histiocytes. They are traditionally classified according to their immunohistochemical phenotype as LCH (CD1a+, S100+, langerin+, and CD68−) and non-LCH (CD68+, CD1a−, S100−, langerin− and factor XIIIa±). ICH is a rare group within this spectrum of histiocytoses, with markers of the 2 main groups, that is, CD1a+, S100+, CD68+, with langerin− (langerin is the immunohistochemical marker of Birbeck granules).1,2
ICH has been reported in patients of all ages and even as a congenital disease. It presents with brownish-red, occasionally ulcerated papular lesions on the trunk and limbs, and that may be widely distributed or occur as an isolated lesion; cases similar to ours, with predominantly or exclusively facial lesions, have been reported.1 Although purely cutaneous involvement with an acute, chronic, or recurrent-remitting presentation and an indolent or even self-resolving clinical course are typical of ICH, eye or bone involvement can occasionally develop, or even multiorgan disease with a fatal outcome.2 Clinical presentation can thus mimic LCH or non-LCH, especially the generalized eruptive forms and benign cephalic histiocytosis, and histology is essential to make the correct diagnosis.3
The pathophysiology of the disease was described by Badalian-Very et al.4 in 2010 in a series of 61 patients with LCH, finding mutations in BRAF V600E in 57% of patients. Three cases were reported recently with translocations in genes ETV3-NCOA2, a genetic alteration not previously found in histiocytosis; NCOA2 codes for the protein TIF2, a transcription cofactor for nuclear steroid receptors.5 These data support the clonal origin of histiocytosis, and in the future may have therapeutic implications. However, cases of histiocytosis with the immunohistochemical profile of ICH have been reported after inflammatory diseases such as scabies or pityriasis rosea and have shown a self-resolving clinical course.6,7 This allows us to propose the hypothesis that the histiocytoses are a spectrum of diseases defined only by their immunohistochemical pattern, and that they include truly neoplastic diseases as well as reactive inflammatory conditions. Molecular study will probably contribute to a better characterization of this entity in the near future.
Because of the low frequency of ICH, no clear drug of choice has yet emerged for its treatment. A wait-and-see approach is an option, given the indolent or even self-resolving course in the majority of cases, with support using topical corticosteroids in the cutaneous forms. However, a wide variety of treatments other than systemic corticosteroids have been reported in the literature, including phototherapy, thalidomide, isotretinoin, methotrexate, cyclophosphamide, pravastatin, electron beam therapy, and the excision of solitary lesions.8,9 Polychemotherapy is an option usually reserved for more serious cases with multiorgan disease and, as with other hematologic tumors, hematopoietic stem cell transplant may be considered in refractory cases that put the patient's life in danger.
In conclusion, we would like to draw attention to the importance of follow-up in these patients for the early detection of possible organ involvement by the disease or the appearance of associated second hematologic tumors. In this regard, low grade B-cell lymphoma and acute leukemia are the most frequently reported in the literature, even years after onset of the ICH, requiring us to perform long-term clinical and laboratory follow-up.10
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Sahuquillo-Torralba A, Navarro-Mira MA, Llavador-Ros M, Botella-Estrada R. Histiocitosis de células indeterminadas en edad pediátrica: a propósito de un caso. Actas Dermosifiliogr. 2017;108:871–874.