The patient was a 3-year-old girl with no history of interest who consulted for asymptomatic hypochromic lesions in the pubic region. The lesions had been present since birth, although they had gradually increased in number and size during the first months of life. Neither her parents nor her older brother had similar lesions.
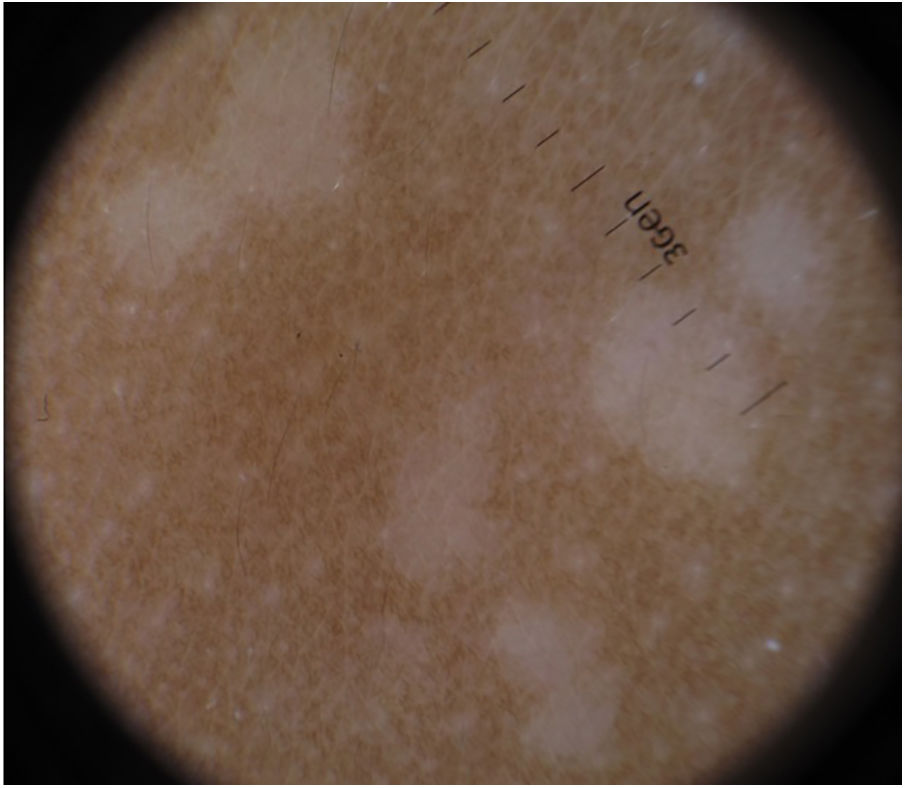
Physical ExaminationWe observed minimally tender hypopigmented papules of different sizes clustered symmetrically in the pubic region (Fig. 1). No lesions were observed in other areas.
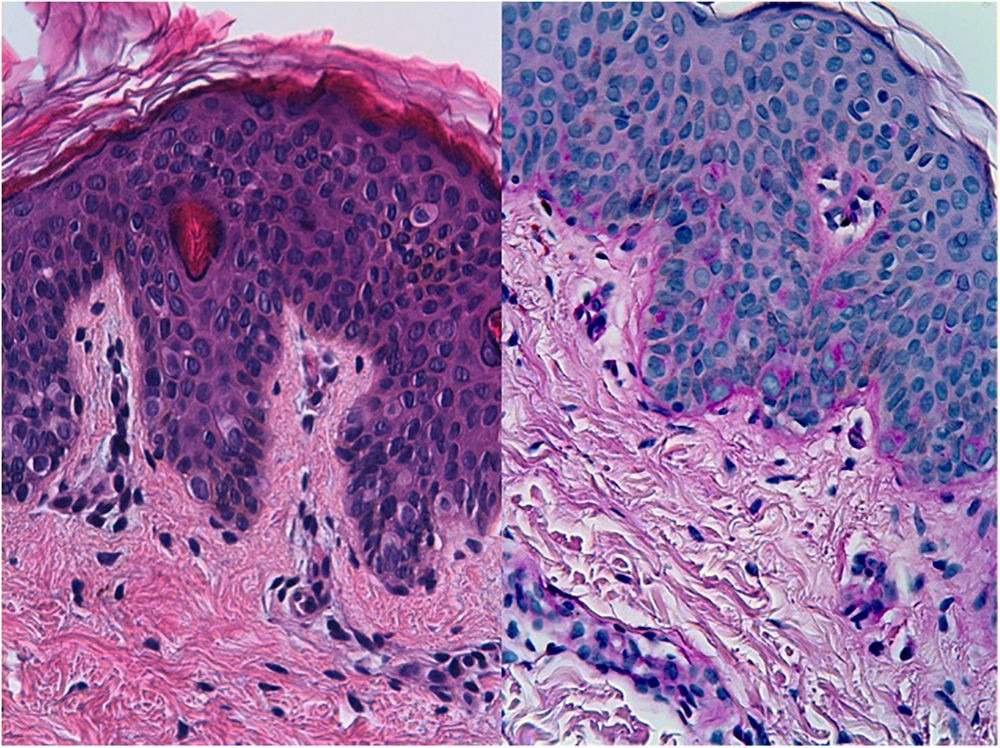
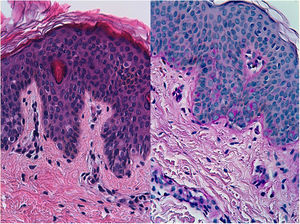
HistopathologyHistopathology was remarkable for the presence of a slightly acanthotic epidermis with mild orthokeratotic hyperkeratosis and numerous cells with a clear and abundant cytoplasm in the lower half of the epidermis (Fig. 2A). The clear cells were positive for periodic acid–Schiff (PAS) staining (Fig. 2B).
Additional TestsDermoscopy revealed well-defined hypopigmented papules measuring 3-4mm with no desquamation or internal structures (Fig. 3).
What is your diagnosis?
DiagnosisClear cell papulosis.
Clinical Course and TreatmentGiven the benign nature of these lesions and the absence of symptoms, we recommended clinical observation.
CommentClear cell papulosis is an uncommon skin condition that affects children and appears as hypopigmented macules and papules generally on the lower abdomen and suprapubic area. Since it was first described in 1987 by Kuo et al.,1 36 cases have been reported. Most involve patients of Asian origin and, to a lesser extent, patients of Hispanic or Indian origin, with a predominance in females (male:female, 1:1.4).1–5 While the etiology of this condition is unknown, the fact that as many as one quarter of the cases reported occur in siblings has led some authors to favor a possible autosomal recessive inheritance pattern.3,4
The lesions may be present at birth, although they usually develop during the first 2 years of life.2 Clinically, they present as multiple, minimally palpable hypopigmented, nondesquamative macules or papules. The lesions are asymptomatic and are found mainly on the lower abdomen and pubis, although they have also been reported on the thorax, axillas, and limbs.3
The differential diagnosis includes progressive macular hypomelanosis, verruca plana, pityriasis versicolor, guttate vitiligo, and nevus anemicus.
Histologically, the lesion is characterized by the presence of large cells with a benign appearance and abundant clear cytoplasm that occur in isolation or are found in small clusters along the basal layer and, occasionally, in the suprabasal layer of the epidermis. Other findings include mild hyperkeratosis, mild to moderate acanthosis, and reduced or no melanin in the basement membrane. The diagnosis is supported by positive staining of clear cells for mucin with PAS, mucicarmine, or alcian blue. Characteristic immunohistochemistry findings include strong positivity for cytokeratin AE1/AE3 and variable positivity for carcinoembryonic antigen and epithelial membrane antigen. Results are consistently negative for S100.2,3
It has traditionally been thought that there is a possible association between clear cells in clear cell papulosis and Toker cells, given the histological and immunohistochemical similarities between them and their distribution along the milk lines. The importance of this association lies in the potential role of Toker cells as precursors in mammary and extramammary Paget disease.4–6 However, current evidence is insufficient to support the hypothesis of an eventual transformation of clear cell papulosis to Paget disease.2,3,5 On the contrary, long-term follow-up has revealed partial or complete resolution of the lesions in the vast majority of cases.3 Recognition of this benign, asymptomatic lesion is important if we are to avoid unnecessary examinations and treatments.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: López-Sánchez C. Pápulas hipopigmentadas en niña sana Eczema y urticaria en Portugal. 2019;110:767–768.