A 40-year-old man was referred by the oncology department for assessment of pigmented lesions on the upper limbs that had appeared progressively over the previous 5 years. The patient's medical history included a cholangiocarcinoma diagnosed 2 years earlier, which was treated with surgery, radiation therapy, chemotherapy, and oral capecitabine. The patient was disease-free at the time of the visit.
The patient reported that the lesions had been stable and asymptomatic since they appeared, that they did not change in appearance when exposed to high temperatures or physical exercise, and that they did not change after treatment with topical antifungal agents prescribed by a primary care physician.
Physical ExaminationPhysical examination revealed multiple well-defined brownish macules with fine superficial telangiectasias, distributed in a bilateral symmetric pattern on the external aspect of both arms (Figs. 1 and 2). The lesions were negative for the Darier sign. No similar lesions were observed elsewhere on the body.
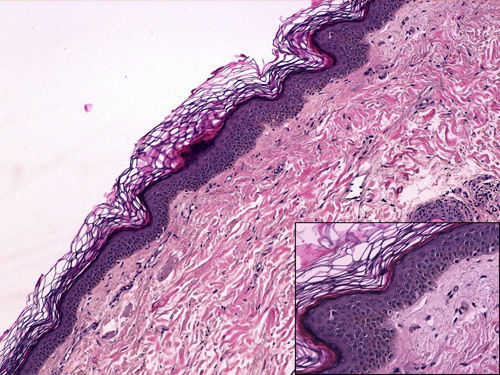
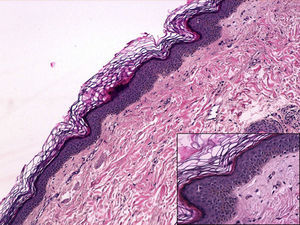
Additional TestsBiopsy of a lesion revealed basal layer hyperpigmentation and no other findings of interest (Fig. 3). No increase in the number of mast cells or melanocytes was observed with hematoxylin-eosin staining or with immunostaining for c-kit.
What Is Your Diagnosis?
DiagnosisAcquired bilateral telangiectatic macules.
Clinical CourseThe lesions have remained stable after 1 year of follow-up.
CommentAcquired bilateral telangiectatic macules are a recently described entity.1 The lesions have certain constant clinical and pathological characteristics that allow them to be differentiated from similar entities.
The lesions typically occur in middle-aged men with skin phototype III-IV1 and follow an insidious clinical course. Patients present with symmetrically distributed brownish erythematous macules with fine superficial telangiectasias on the extensor surface of the arms. The lesions are asymptomatic and negative for the Darier sign.
Histologic examination of the lesions reveals basal layer hyperpigmentation and capillary proliferation in the dermis, sometimes accompanied by a subtle perivascular inflammatory infiltrate.1 No epidermal alterations are present and the number of mast cells and melanocytes is normal (as can be confirmed by immunohistochemistry for c-kit and Fontana-Masson staining, respectively).
In the case series described by Park et al., the lesions did not improve spontaneously in any of the patients after a mean follow-up period of 4 years. In the case of our patient, we did not prescribe treatment because the lesions were asymptomatic and stable. No significant changes were observed during 14 months of follow-up.
The differential diagnosis includes the following:
- −
Telangiectasia macularis eruptiva perstans2,3: Indolent cutaneous mastocytosis characterized by brownish erythematous macules that are generally asymptomatic. The lesions tend to be negative for the Darier sign. Unlike acquired bilateral telangiectatic macules, this entity also tends to affect the trunk. Histologically, it is characterized by an increase in the number of mast cells.
- −
Acquired brachial cutaneous dyschromatosis4: This recently described entity affects postmenopausal women and is characterized by greyish-brown asymptomatic macules on the extensor surface of the arms. Histologically, it is characterized by epidermal atrophy, basal layer hyperpigmentation, and solar elastosis. Its appearance has been associated with UV radiation and the ingestion of angiotensin-converting enzyme inhibitors.
- −
Generalized essential telangiectasia5: This entity typically occurs in women 40 to 50 years of age. It manifests as asymptomatic telangiectasias on the lower limbs that subsequently become generalized and is not associated with systemic diseases.
- −
Hereditary benign telangiectasia6: This rare entity is more frequent in women and children and is characterized by punctate telangiectasias surrounded by a pale halo on the upper third of the trunk, the arms, and the head. The lesions are asymptomatic and are not associated with systemic disease.
- −
Drug-induced hyperpigmentation: Various drugs—including antimalarial agents, chemotherapeutic agents, antibiotics, amiodarone, phenytoin, and heavy metals—have been associated with pigmentary alterations. In order to diagnose this entity, a good medical history must be taken and a temporal relationship must be established between the administration of the drug and the appearance of the lesions.
Therefore, differences in sex and age at onset, the absence of systemic symptoms, the site of the lesions, and histologic findings allow us to rule out other diseases and confirm the diagnosis of acquired bilateral telangiectatic macules.
In conclusion, we have presented a new case of acquired bilateral telangiectatic macules, a recently described entity characterized by asymptomatic pigmented lesions on the arms that occurs in grown men and follows a chronic indolent clinical course.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: de Asís-Cuestas S. Máculas hiperpigmentadas bilaterales en brazos de un varón joven. Actas Dermosifiliogr. 2016;107:683–684.