Hidradenitis suppurativa is a chronic recurrent systemic inflammatory disease that mainly involves large skin folds. It develops when pilosebaceous units become blocked, leading to the formation of painful nodules, abscesses, fistulas, and scarring. The impact of this disease on quality of life is great.
ObjectivesTo describe the prevalence and clinical features of hidradenitis suppurativa in patients treated at Hospital Italiano de Buenos Aires and determine the frequency of comorbidities and time to diagnosis in this population.
Material and methodsRetrospective descriptive cross-sectional study. Information was extracted from the computerized clinical records of all patients with a diagnosis of hidradenitis suppurativa managed in Hospital Italiano de Buenos Aires between July 2012 and October 2017.
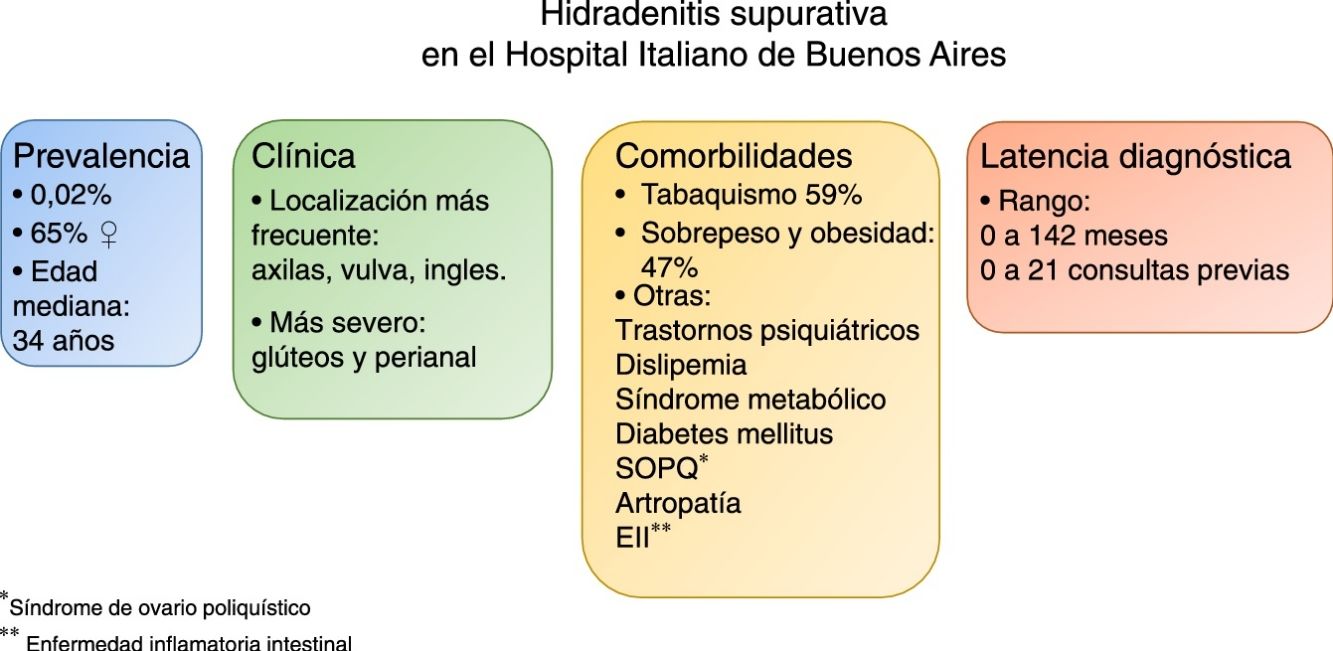
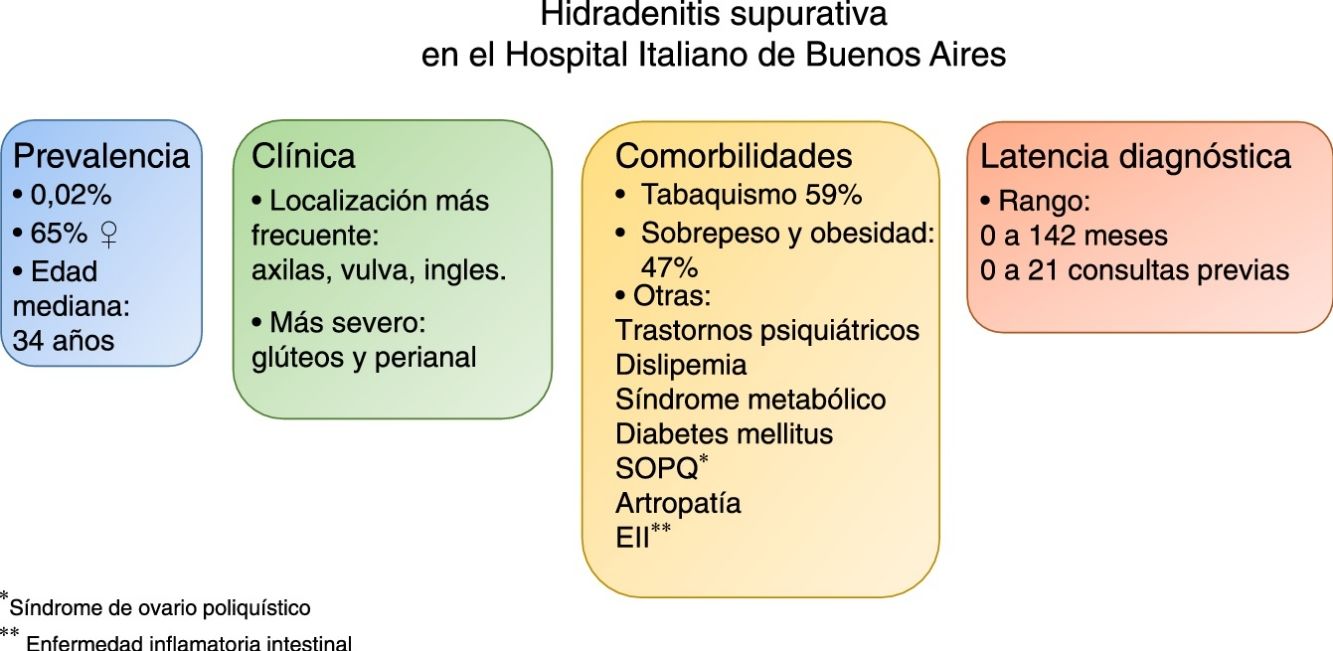
ResultsOur initial search of the records yielded 180 cases; the diagnosis was confirmed in 66 cases. Sixty-five percent of the patients were women, and the mean age was 37 years. The prevalence of this diagnosis was 0.02%.
The armpits, vulva, and groin were the locations most frequently affected. Smoking, overweight, and obesity were the most commonly recorded concomitant conditions.
Male sex and perianal and gluteal locations were associated with severity.
Time until diagnosis varied widely, ranging from diagnosis at the first visit in some cases to as long as 142 months and 21 visits.
ConclusionsOur findings are consistent with the literature on hidradenitis suppurativa. This is the first Argentinian study to describe the prevalence of this disease as well as the concomitant conditions found and the rate of diagnostic error.
La hidradenitis supurativa es una enfermedad sistémica inflamatoria crónica y recurrente, que afecta, principalmente, los grandes pliegues. Se origina por la oclusión de las unidades pilosebáceas, con la consecuente formación de nódulos dolorosos, abscesos, fístulas y cicatrices, con un alto impacto en la calidad de vida.
ObjetivosDescribir prevalencia, características clínicas, frecuencia de comorbilidades y latencia diagnóstica, en pacientes con hidradenitis supurativa atendidos en el Hospital Italiano de Buenos Aires.
Materiales y métodosEstudio retrospectivo descriptivo de corte transversal. Se relevó la información de las historias clínicas electrónicas de todos los pacientes con diagnóstico de hidradenitis supurativa atendidos en el Hospital Italiano de Buenos Aires entre julio de 2012 y octubre de 2017.
ResultadosLa búsqueda inicial en nuestra base de datos arrojó 180 historias clínicas. En 66 casos se confirmó el diagnóstico. Un 65% eran mujeres. La edad media fue 37 años. La prevalencia fue de 0,02%.
Las áreas más afectadas fueron las axilas, la vulva y las ingles. El tabaquismo y el sobrepeso u obesidad fueron las comorbilidades más frecuentes.
El sexo masculino y las localizaciones perianal y glútea, se asociaron a casos más graves.
El lapso al diagnóstico tuvo un intervalo muy amplio, desde un diagnóstico en la primera consulta, hasta una demora de 142 meses y 21 consultas previas.
ConclusionesNuestros resultados se encuentran dentro de los valores de la literatura. Este es el primer trabajo de Argentina que describe la prevalencia, las comorbilidades y el error diagnóstico en la hidradenitis supurativa.
Hidradenitis suppurativa (HS) is a chronic recurrent systemic inflammatory disease that mainly affects large skinfolds. It is caused by obstruction of the pilosebaceous units, which in turn leads to the formation of painful nodules, abscesses, fistulas, and scars. The impact on quality of life is considerable.
Diagnosis is often late owing to the course of the disease, which is characterized by flares and remissions. In addition, HS is rarely seen outside the field of dermatology.
Epidemiology findings suggest that patients with HS have a greater prevalence of comorbid conditions than the general population. The most frequent are smoking and obesity.1,2
Most published studies on the prevalence of HS and its associated conditions analyzed European or North American populations. It is well known that data on health care statistics are lacking in Latin America, and the case of HS is no exception. The only research on prevalence was in a recently published survey in Brazil.3
Therefore, the objectives of the present study were to examine the prevalence of HS, describe the clinical characteristics of the disease, investigate the presence of comorbid conditions, and calculate the time to diagnosis.
Materials and MethodsWe performed a retrospective, descriptive, cross-sectional study. The study population comprised patients seen at Hospital Italiano de Buenos Aires (HIBA), Buenos Aires, Argentina.
The Argentinian health system is divided into 3 main sectors: the public sector, the private sector (medical prepayment companies), and the social security sector (insurance plans). The last two cover a population of approximately 18 million people distributed over around 300 organizations. In this context, HIBA provides medical and health care services via 2 main hospitals and 24 peripheral centers to patients belonging to HIBA's own prepayment system (Plan de Salud del HIBA [HIBA Health Plan]), which currently has some 160 000 members, and to members of more than 200 insurance plans and prepayment companies. The population seen at HIBA comprises mainly the inhabitants of urban areas of the city of Buenos Aires. The city covers an area of 202km2 and has a subtropical climate. It is located on the west bank of the Río de la Plata and has a population of 2 890 151 inhabitants (2010 census). White people of European descent make up 92% of the population; the remainder is comprised of a mix of indigenous and other ethnic groups.
After receiving the approval of the Research Protocol Ethics Committee of HIBA, we asked the management area for data on all patients who were diagnosed with hidradenitis suppurativa (or hidrosadenitis suppurativa, or acne inversa) between July 2012 and October 2017. As the electronic clinical history system of HIBA is problem-oriented, we requested a search for patients whose problems included these terms.
The diagnosis of HS was validated in 2 circumstances: cases where it had been confirmed by a dermatologist; and cases where the clinical description was accurate and corresponded to HS. In doubtful cases, the electronic clinical history was reviewed, and the diagnosis was confirmed by the principal investigator.
For each patient we collected demographic and clinical variables, the presence or absence of comorbid conditions, and the interval between the first contact with the hospital and diagnosis, as well as the number of visits.
Statistical AnalysisWe calculated the prevalence based on the number of patients who were members of the Health Plan with a confirmed diagnosis of HS over the total number patients who were active members of the Health Plan during the study period.
We reported the clinical characteristics and the presence of comorbid conditions for all patients with HS seen at HIBA. Data were reported as absolute and relative frequencies.
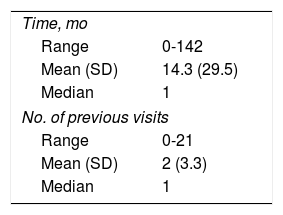
We measured the time to and number of visits before diagnosis for all patients seen at HIBA. Data were reported as the interval and mean (SD).
We also performed bivariate analyses using sex and specific locations as the independent variables and severity as the dependent variable.
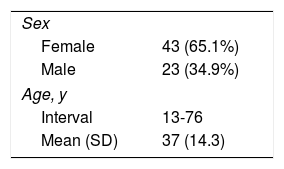
ResultsThe initial search of our database yielded 180 clinical histories that fulfilled the search criteria (see above). A diagnosis of HS was confirmed in 66 cases. The remainder mainly had acute infectious processes such as furuncles or abscesses in skinfolds that were wrongly classified as HS. In other words, in the electronic clinical history, classifying hidradenitis suppurativa (or hidrosadenitis suppurativa) as a problem had a positive predictive value of 37% (66/180). Of the 66 cases of confirmed HS, 65% affected women. All of the patients were white, with a mean age at diagnosis of 37 years. Of the 143 245 active members in October 2017, 29 were members of the HIBA Health Plan. The prevalence of HS was 2.02 cases per 10 000 (95% CI, 1.35-2.9) (Table 1).
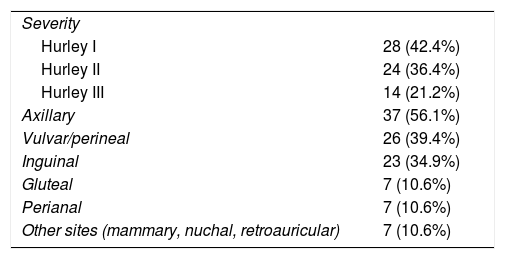
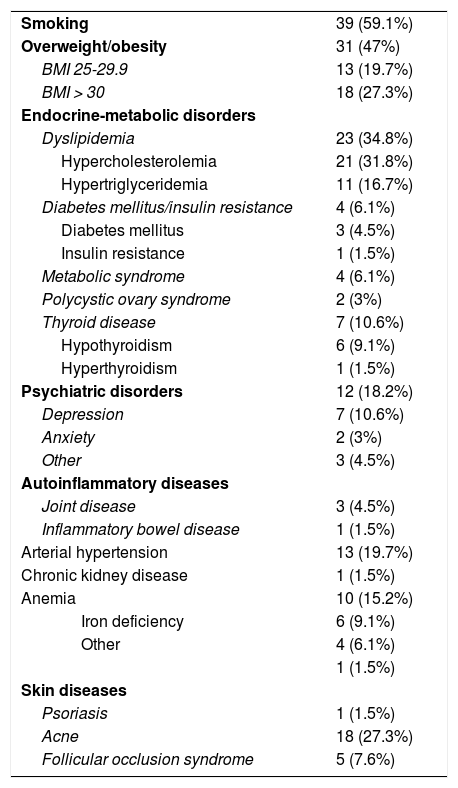
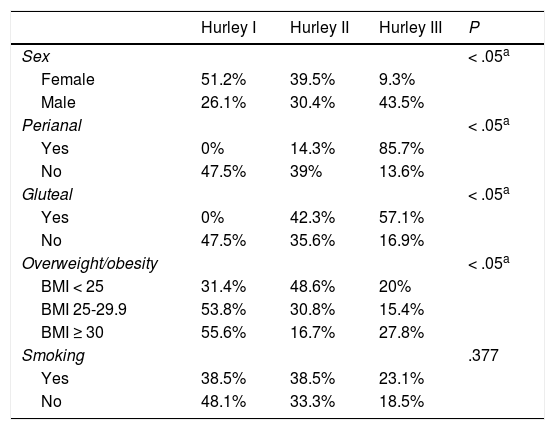
As for severity, most cases were mild (Hurley I). The most affected areas were the axillas, vulva, and groin, in that order (Table 2). One-third of patients (22) were affected at multiple sites. Table 3 summarizes the associated comorbid conditions. The most common were smoking and overweight or obesity. No patients had liver disease, pyoderma gangrenosum, autoinflammatory syndromes (synovitis, acne, pustulosis, hyperostosis, and osteitis; pyoderma gangrenosum, acne, and hidradenitis suppurativa; and pyogenic arthritis, pyoderma gangrenosum, acne, and hidradenitis suppurativa), Down syndrome, or cancer (lymphoma, squamous cell carcinoma). The most severe cases were associated with male sex and perianal and gluteal location (P < .05) (Table 4).Table 5 shows the time to diagnosis.
Comorbidities (N = 66).
| Smoking | 39 (59.1%) |
| Overweight/obesity | 31 (47%) |
| BMI 25-29.9 | 13 (19.7%) |
| BMI > 30 | 18 (27.3%) |
| Endocrine-metabolic disorders | |
| Dyslipidemia | 23 (34.8%) |
| Hypercholesterolemia | 21 (31.8%) |
| Hypertriglyceridemia | 11 (16.7%) |
| Diabetes mellitus/insulin resistance | 4 (6.1%) |
| Diabetes mellitus | 3 (4.5%) |
| Insulin resistance | 1 (1.5%) |
| Metabolic syndrome | 4 (6.1%) |
| Polycystic ovary syndrome | 2 (3%) |
| Thyroid disease | 7 (10.6%) |
| Hypothyroidism | 6 (9.1%) |
| Hyperthyroidism | 1 (1.5%) |
| Psychiatric disorders | 12 (18.2%) |
| Depression | 7 (10.6%) |
| Anxiety | 2 (3%) |
| Other | 3 (4.5%) |
| Autoinflammatory diseases | |
| Joint disease | 3 (4.5%) |
| Inflammatory bowel disease | 1 (1.5%) |
| Arterial hypertension | 13 (19.7%) |
| Chronic kidney disease | 1 (1.5%) |
| Anemia | 10 (15.2%) |
| Iron deficiency | 6 (9.1%) |
| Other | 4 (6.1%) |
| 1 (1.5%) | |
| Skin diseases | |
| Psoriasis | 1 (1.5%) |
| Acne | 18 (27.3%) |
| Follicular occlusion syndrome | 5 (7.6%) |
Abbreviation: BMI, body mass index.
Severity According to Sex, Location, and Comorbidity (N = 66).
| Hurley I | Hurley II | Hurley III | P | |
|---|---|---|---|---|
| Sex | < .05a | |||
| Female | 51.2% | 39.5% | 9.3% | |
| Male | 26.1% | 30.4% | 43.5% | |
| Perianal | < .05a | |||
| Yes | 0% | 14.3% | 85.7% | |
| No | 47.5% | 39% | 13.6% | |
| Gluteal | < .05a | |||
| Yes | 0% | 42.3% | 57.1% | |
| No | 47.5% | 35.6% | 16.9% | |
| Overweight/obesity | < .05a | |||
| BMI < 25 | 31.4% | 48.6% | 20% | |
| BMI 25-29.9 | 53.8% | 30.8% | 15.4% | |
| BMI ≥ 30 | 55.6% | 16.7% | 27.8% | |
| Smoking | .377 | |||
| Yes | 38.5% | 38.5% | 23.1% | |
| No | 48.1% | 33.3% | 18.5% |
Abbreviation: BMI, body mass index.
Our study provides new data on the prevalence, clinical characteristics, comorbidities, and time to diagnosis of HS in a representative closed health system in the city of Buenos Aires. The prevalence was 0.02%, which is consistent with reports from other series throughout the world (0.00033 to 4.1%).4,5 It is important to note that this wide range is due to variability in study design and quality and to racial heterogeneity (greater prevalence in African Americans).6 Furthermore, we believe that the prevalence we report could be underestimated, because the cases we recorded were those where HS is entered into the electronic clinical history by the physician as a problem, and it is not uncommon for health professionals to fail to record this.
Almost 60% of the study patients were smokers; the percentage of smokers ranges from 30% to 92% in the literature.1,2,4,7–9 Smoking increases the risk of developing HS by 2- to 12-fold.10 Some authors have even demonstrated an association between smoking and the severity of HS,11 although this remains open to debate, given that other studies found no such association.12,13 In fact, we were unable to verify this association in our study (Table 4).
More than half of the study patients were overweight or obese. The frequency of obesity is reported to be between 12% and 88%.1,7–9,12,14 It has been suggested that obesity is associated with severity. However, our bivariate analysis showed overweight and obesity to be associated with less severe cases (Table 4). We postulate that this phenomenon arises from the fact that severe forms manifest in patients with a marked genetic predisposition, who would go on to develop the disease irrespective of the associated risk factors; milder forms, on the other hand, would in fact be triggered by risk factors (in this case obesity and friction) where genetic predisposition is not predominant and, therefore, patients are not likely to develop such severe forms. In any case, our study population was small and uncontrolled, thus making it risky to draw conclusions. Other studies should evaluate our hypothesis.
Approximately one-third of the patients had dyslipidemia. Previous studies report variable parameters that sometimes differed from ours; the frequency of altered values (high low-density lipoprotein cholesterol, low high-density lipoprotein cholesterol, hypertriglyceridemia) ranged between 10% and 54%, and these were not always significant when compared with controls.4,7–9,14 In our study, the percentage of patients with diabetes mellitus was at the lower limit of values reported in the literature (5%-20%),1,4,7–9,14 and that of metabolic syndrome was lower (10%-51%).8,9,14 These differences may have been due to the characteristics of the study population, since most studies are from North America, where the prevalence of obesity, metabolic syndrome, and diabetes mellitus is greater. The percentage of polycystic ovary syndrome was similar to that described by another original study (4%), in which the prevalence was 13-fold greater than in the control group.4
In our series, 1 in every 5 patients had an associated psychiatric disorder, mainly depression or anxiety. Similarly, the most common psychiatric comorbid condition in the literature is depression (6%-43%),15–17 followed by anxiety and alcoholism (4%),4,16 and, to a lesser extent, schizophrenia and bipolar disorder.18 A key finding in one study was that 57% of patients had psychiatric comorbid conditions.4
While the design of the present study is not the most appropriate for determining associations with other comorbid conditions, our data suggest that the prevalence of some highly prevalent conditions such as arterial hypertension, thyroid disease, anemia, acne, and psoriasis would be no different in patients with HS than in the general population, as reported in the literature.7–9,14,19,20 The frequency of acne in our study was similar to that of the general population, although the percentage of patients with follicular occlusion syndrome (whose manifestations include acne conglobata) was, in fact, higher, probably owing to the pathophysiology of the disease.21
An association with Down syndrome has been reported,21,22 as has an increase in the incidence of cancers such as squamous cell carcinoma and lymphoma23,24; however, these comorbidities were not recorded in our series.
Our study is limited by the lack of a control group, which would have proved useful for comparing the prevalence of comorbidities between the groups and for determining the degree of association between each of them and the study disease.
Time to diagnosis was very variable, and in many cases, it was difficult to determine owing to the retrospective design of the study. It is interesting to note that few studies analyze this aspect and instead measure the time between onset of symptoms and diagnosis, with a mean of 7 years.25 In our case, we measured the time and number of visits from the first consultation associated with the problem and diagnosis, which refers to the delay on the part of the physician and excludes the delay resulting from the patient's decision to consult a health professional.
ConclusionsHS is frequently subject to diagnostic delay. It is characterized by a chronic course and has a marked effect on quality of life. Prognosis can be improved with early intervention. We propose strategies for early diagnosis and treatment of HS, such as educational campaigns for physicians and patients. Of note, this is the first study in Argentina to report the prevalence, comorbid conditions, and diagnostic error in HS.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Zimman S, Comparatore MV, Vulcano AF, Absi ML, Mazzuoccolo LD. Hidradenitis supurativa: una aproximación a su prevalencia, características clínicas, comorbilidades y tiempo al diagnóstico, en un hospital universitario de Buenos Aires, Argentina. Actas Dermosifiliogr. 2019;110:297–302.