Sarcoid dactylitis is a rare manifestation, observed in 0.2% of cases of sarcoidosis. It usually courses with swelling of the fingers or toes, mainly affecting the middle phalanges and, less often, the distal phalanges.1
A 38-year-old woman visited our department with inflammation and pain in the toes of the right foot, accompanied by abnormal nails, which had appeared 3 months earlier. The patient presented erythematous, lupoid facial lesions that had appeared a year earlier and were associated with bilateral enlarged cervical lymph nodes. Examination revealed erythema with edema and swelling in the first 3 toes of the right foot, associated with dystrophic toenails, and erythematous lesions with adhered crusts on the nose, forehead, and cheeks (Fig. 1).
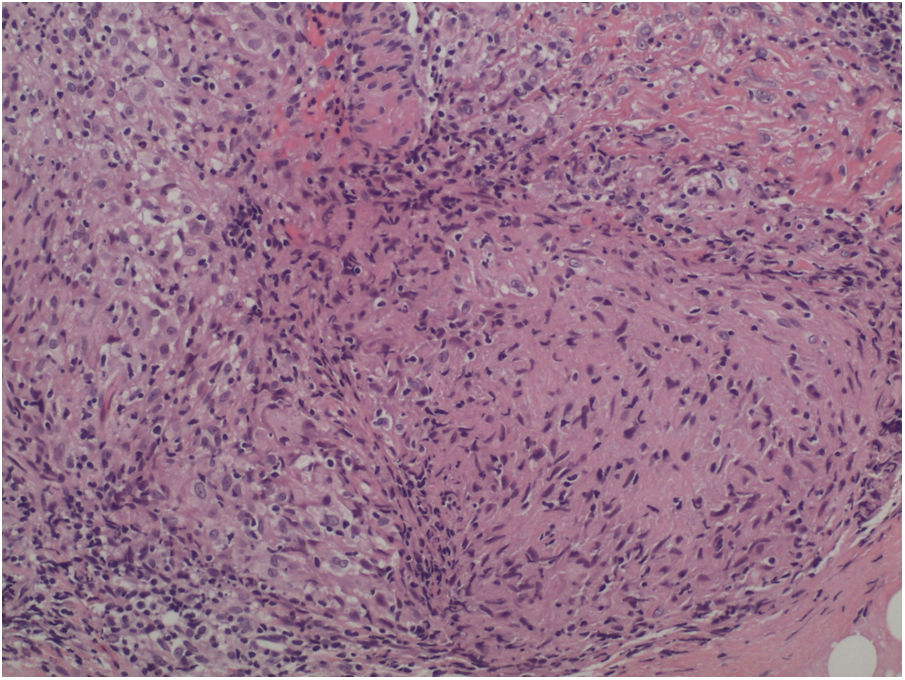
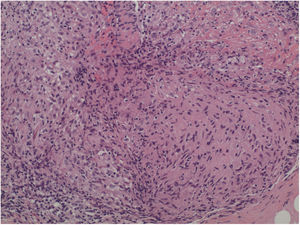
The biopsy of the cervical lymph nodes revealed a sarcoid granulomatous lymphadenitis, with negative staining for Ziehl-Neelsen, Grocott, and PAS. Blood cultures and urine tests were negative for aerobes, anaerobes, and Mycobacterium species were negative. The histologic study of the skin lesions on the face and right foot revealed the existence of naked granulomas, with no central necrosis or lymphocytic corona, in the deep and middle dermis (Fig. 2).
Blood tests showed increased levels of angiotensin-converting enzyme and acute phase reactants, and serology for syphilis was negative.
The x-ray study revealed destruction of the distal phalanx of the first toe, with signs of bone resorption and tendinitis.
The CT scan showed a small number of enlarged hilar, subcarinal mediastinal, and retroperitoneal lymph nodes associated with bilateral micronodules in the upper third of the lung fields.
A diagnosis of sarcoid dactylitis in the context of systemic sarcoidosis was made and treatment was initiated with oral corticosteroids associated with hydroxychloroquine; a slight improvement was achieved and this treatment was therefore suspended. Treatment was begun with 150 mg/d of azathioprine. After 6 months of treatment, the swelling of the toes had been reduced and the crusts of the facial lesions had disappeared (Fig. 3). After a year of treatment only the erythematous lesions persist, with no crust or swelling.
Bone involvement in sarcoidosis usually manifests in the form of joint pain, whereas deforming arthritis is rare.2 Two patterns of appearance of sarcoid joint disease exist: an early form of presentation that occurs in the first 6 months and is usually observed in Löfgren syndrome, and a late-onset form that affects multiple joints, generally those of the small bones of the hands and feet and which appears after 6 months.3 They are often associated with nail disorders, acropachy with racket nails, or acrosclerosis.
Radiologically, sarcoid dactylitis is characterized by trabecular abnormalities with a honeycomb or barred pattern, which may be associated with cystic formations and a periosteal reaction.4
Histologically, in bone lesions, noncaseating granulomas are found that invade the phalanges and the surrounding soft tissue. This granulomatous dactylitis is associated with a worse outcome and greater risk of systemic involvement and of lupus pernio in chronic sarcoidosis.5
Lupus pernio is one of the most characteristic lesions of sarcoidosis, which is more frequent in Caucasian women with long-term disease, as in our case.1 It is characterized by pink or violaceous papular lesions on the nose, cheeks, ears, lips, or scalp. It tends to be associated with chronic sarcoidosis and involvement of the upper respiratory apparatus. If the lupus pernio lesions are located on the fingers or toes, cystic bone lesions on the phalanges of the affected members are often observed.6
Bone involvement tends to be associated with a fourfold higher mortality; however, patients do not usually have symptoms, despite the presence of abnormal radiologic findings.2
Treatment of sarcoid dactylitis requires the use of high-dose corticosteroids associated with antimalarial drugs and methotrexate. In our patient, we ruled out the use of methotrexate owing to the patient’s stated desire to have children and we therefore used azathioprine for some time, and we even considered the use of adalimumab, but this was refused by the patient. The use of anti-TNF-α agents, infliximab, or adalimumab is considered third-line treatment in sarcoidosis, and is useful in refractory cases or cases with ocular or systemic involvement.7
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: García Morales I, Sánchez García E, Crespo Cruz A, Escudero J. Dactilitis granulomatosa como manifestación inusual de la sarcoidosis. Actas Dermosifiliogr. 2021;112:851–853.