Transitional cell carcinoma of the bladder is an aggressive tumor with a high potential for malignant progression. Bacille Calmette-Guérin (BCG) has been used to treat malignant diseases for more than 20 years, and bladder cancer has been treated with it longer, since 1976.1–3 BCG is an attenuated strain of Mycobacterium bovis; instilled in solution to treat bladder cancer, it delays recurrence and prevents the implantation of tumor cells.4,5 Most patients tolerate intravesical irrigation with BCG well, but complications are not unusual. Side effects consist mainly of local irritation and flu-like symptoms and are usually mild. Various systemic and local infections have also been reported following instillation of BCG, which is a live organism. Such infections have included pneumonitis, hepatitis, granulomatous prostatitis, epididymitis, and renal parenchymal abscess.1–4,6
We present a case of granulomatous balanoposthitis that followed intravesical BCG therapy to prevent recurrence after transurethral resection of a transitional cell carcinoma.
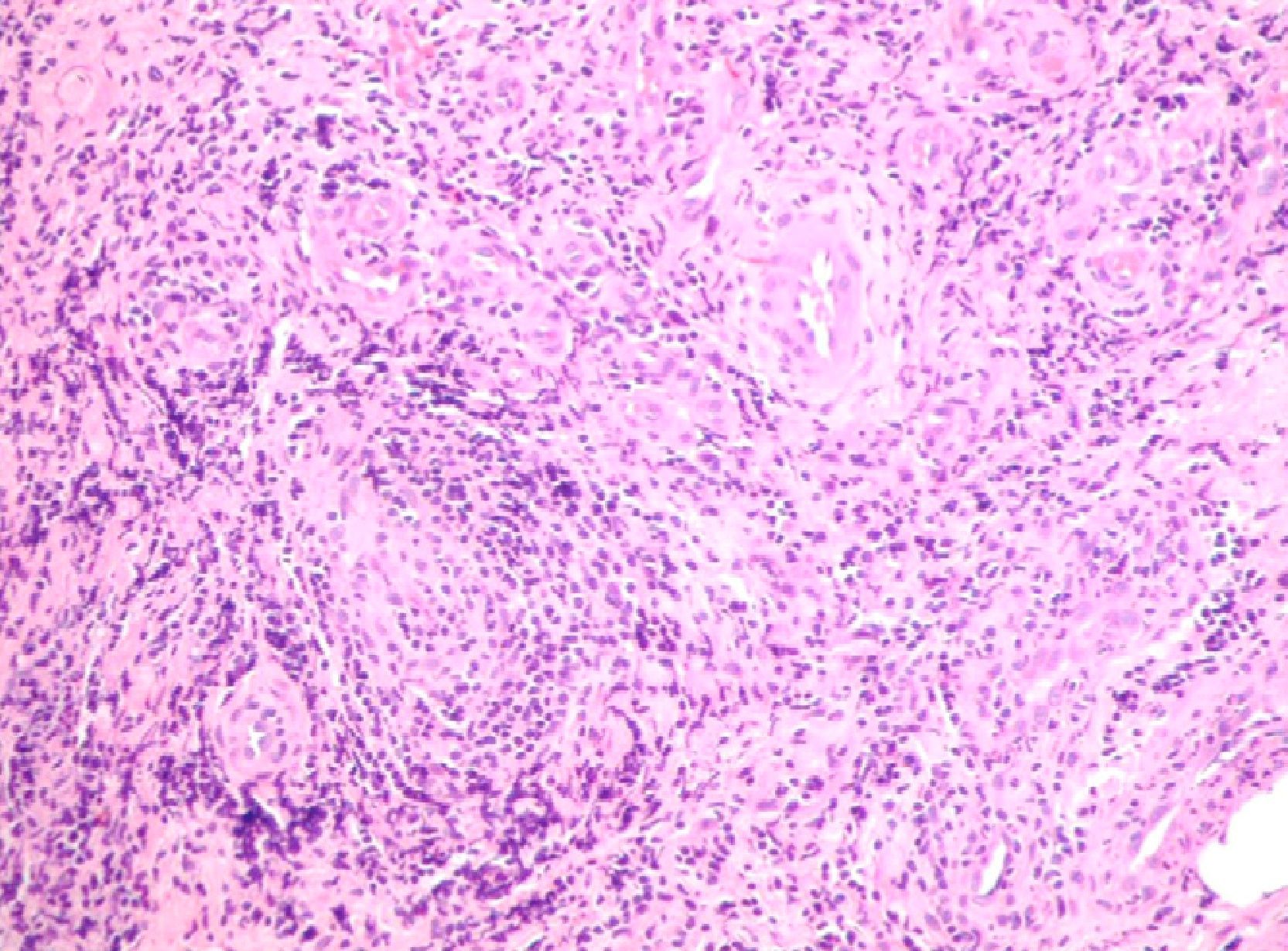
A 40-year-old man received intermittent cycles of intravesical BCG therapy to treat transitional cell carcinoma of the bladder starting in 2009. At 48hours from the sixth instillation, which involved a difficult catheterization with slight extravasation of the product, the patient presented with yellowish papular lesions on the glans penis, large painful lymph nodes in the right groin, and dysuria (Fig. 1). A biopsy was performed and cultures were ordered. In the differential diagnosis, we considered infectious diseases (herpetic primo-infection, syphilis, fungal infection, skin infection due to BCG) and neutrophilic diseases (pyoderma gangrenosum, Behçet disease).
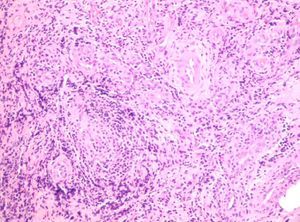
Histology showed a substantial neutrophilic infiltrate in the dermis with no granulomas or multinucleated giant cells (Fig. 2). Ziehl-Neelsen and periodic acid-Schiff staining were negative for micro-organisms. The culture, which was negative for fungi, grew only Streptococcus salivarius (a saprophyte). Despite the negative results of the acid-fast staining, BCG infection was suspected because the other candidate diagnoses were unlikely. Empirical treatment with isoniazid and rifampicin was ordered and by 15 days had reduced the spread of the lesions. At this time, isoniazid-resistant M bovis was isolated in the initial culture in Lowenstein medium. Rifampicin, ethambutol, and moxifloxacin were then prescribed and the lesions had improved considerably after 2 weeks of treatment (Fig. 3).
Intravesical BCG treatment is recognized as an effective therapy for superficial bladder cancer, although numerous side effects have been reported.5 The most common reactions are minor and include cystitis, hematuria, low-grade fever, general malaise, and nausea. More serious side effects include fever, granulomatous pneumonitis, hepatitis, renal abscess, and even fatal sepsis.2,3,7 Granulomatous reactions associated with BCG therapy can occur in the bladder, epididymis, prostate, kidney, lungs, and liver. However, involvement of the glans penis and urethra is quite rare: only 12 cases have been reported to date.3,8 In each case, pathology showed granulomas and, usually, caseating necrosis. These findings were not present in our patient, perhaps because the biopsy was performed promptly.
A recently published study showed that polymorphonuclear cells play an essential role in the antitumor effect of BCG treatment. Instillation of BCG starts a primarily neutrophilic inflammatory reaction that triggers the migration of effector cells (lymphocytes and monocytes or macrophages) to the bladder.3,5
Patients who are immunocompromised, have mucosal barrier disruption due to injury, or have positive reactions on tuberculin skin testing are at higher risk of presenting BCG side effects.3,4,6,7
Given the small number of published cases, no standard treatment has emerged. Some reviews recommend starting the treatment of prostatitis and granulomatous orchiepididymitis with 300mg of oral isoniazid and 600mg of rifampicin and continuing it for 3 to 6 months while discontinuing BCG therapy and testing for antibiotic resistance.3,7 Other authors recommend corticosteroid therapy at the start of treatment.2
This rare case of balanitis due to BCG demonstrates the need to consider this possible side effect when patients are undergoing BCG therapy.
Please cite this article as: García Baldoví M, et al. Balanitis granulomatosa tras terapia intravesical con bacilo de Calmette- Guérin. Actas Dermosifiliogr. 2013;104:251–2.