A 9-year-old girl with a history of obesity came to our clinic for evaluation of pruritic skin lesions that had appeared over 3 months earlier on the trunk and limbs. She had not received any pharmacological treatments or vaccinations and no infections or family history of skin diseases were reported.
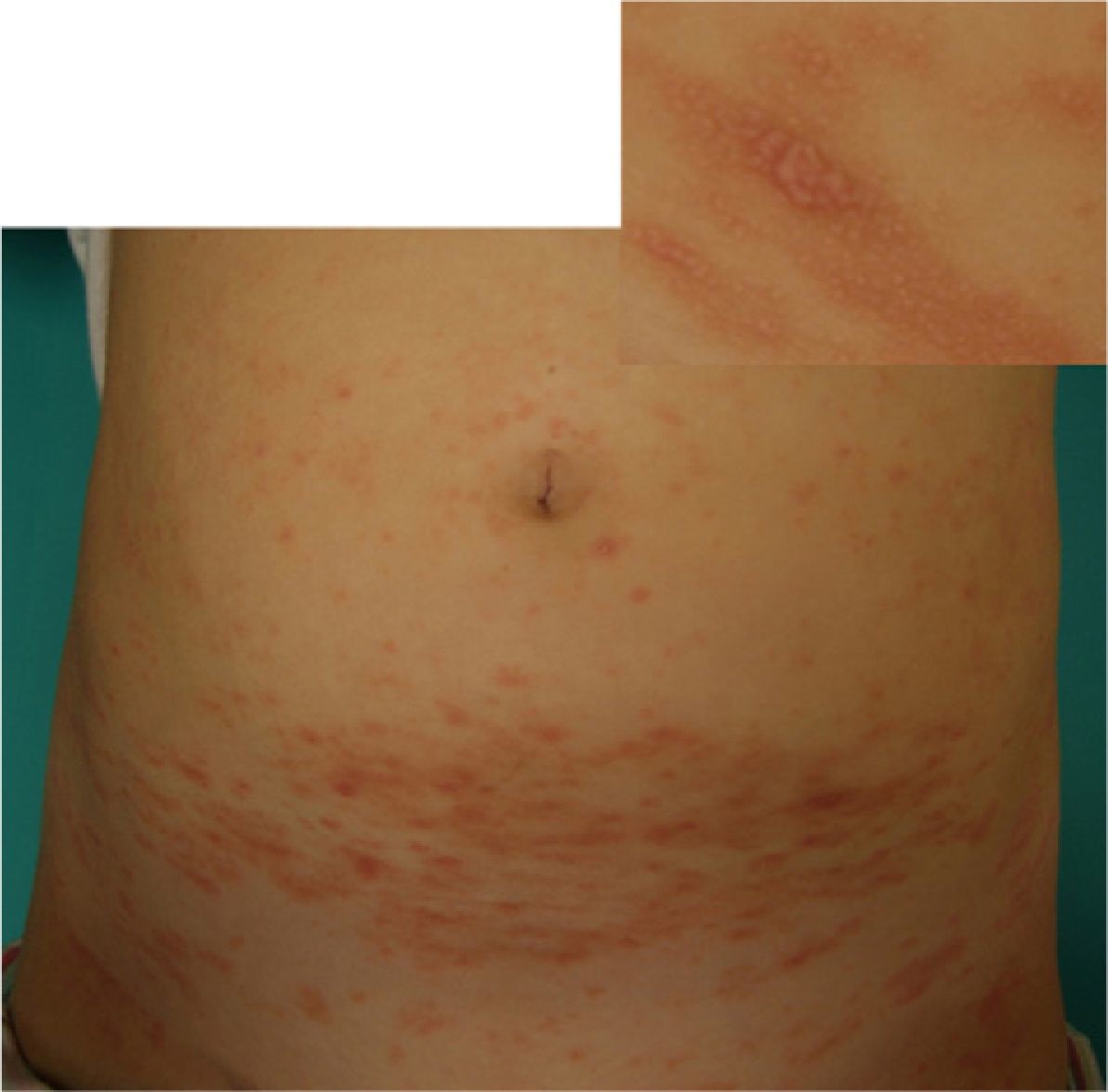
Physical ExaminationWe observed flat, pink polygonal papules and plaques with fine superficial scaling in the form of whitish lines. These lesions affected the ankles, upper limbs, trunk (Fig. 1), and palms and soles (Fig. 2). In addition, the fingernails showed longitudinal ridges and some of them showed fraying of the distal edges. There was no involvement of the scalp or mucous membranes. A Koebner phenomenon was observed on scratched skin.
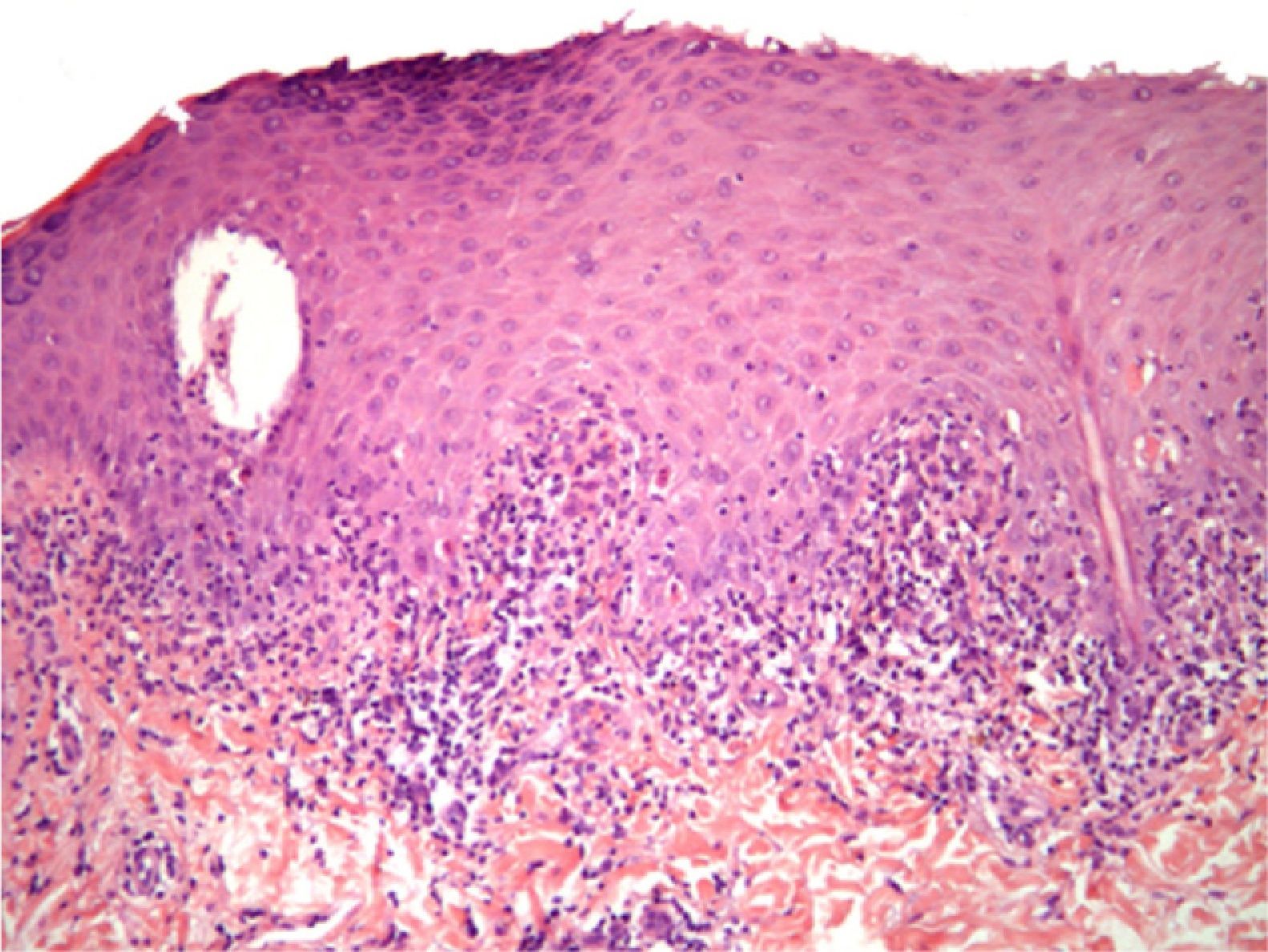
HistologyHistology revealed acanthosis, hypergranulosis, and lichenoid infiltrate with marked damage to basal keratinocytes (Fig. 3).
Additional TestsLaboratory tests (routine blood and urine tests, biochemistry, and hepatitis serology) revealed no pathological findings.
What is your diagnosis?
DiagnosisChildhood lichen planus.
Clinical Course and TreatmentThe patient was treated with oral antihistamines and medium-potency topical corticosteroids for 2 weeks and subsequently with a 0.1% tacrolimus ointment. In 2 months she achieved complete remission.
CommentLichen planus, first described by Wilson in 1869,1 is a chronic inflammatory dermatosis that affects the skin, mucous membranes, and skin appendages and is more common in adults. Cases of this disease in children account for 1–4% of the total, although the incidence appears to be higher in darkly pigmented races. Lichen planus affects men and women equally and is extremely rare in children under 4 years of age. In the literature there are very few reports of childhood lichen planus with involvement of palms and soles.
The typical presentation of lichen planus is as small, flat, violaceous polygonal papules that cause severe itching. The lesions appear as a symmetrical eruption that may be generalized or affect a few areas. They are located mainly on the anterior face of the wrists, the backs of the hands, the lumbar region, and the pretibial area, with exceptional involvement of the face, scalp, and palms and soles. In children the lesions are frequently eruptive and involvement of the trunk is more frequent than in adults.
Cases of lichen planus occurring after hepatitis B vaccination have been reported. In these cases the lesions usually appear a median of 40 days after vaccination. They tend to start on the limbs and cases with a bullous component are not infrequent.
The duration of the disease varies from a few weeks to several years. Although lichen planus is usually a skin disease without other systemic involvement, it can sometimes be associated with autoimmune diseases and chronic hepatitis, especially hepatitis C virus in some areas where it has a high prevalence, such as Spain, Italy, and France.2
Involvement of palms and soles, which is uncommon in adults,3 is even more uncommon in children.4–6 Recently, Handa and Sahoo5 found 2 cases (2.3%) of lichen planus with involvement of palms and soles in their study of 87 children with lichen planus. On the palms and soles the lesions do not have the typical clinical presentation of lichen planus, so diagnosis is difficult. Furthermore, Wickham striae are not observed, probably because of the greater thickness of the stratum corneum. However, the histopathologic characteristics are similar to those of other locations.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Martí N, et al. Erupción generalizada en una niña. Actas Dermosifiliogr. 2012;103:153–6.