The term comes from James Ewing (1866-1943) who was the first to describe the tumor, establishing that the disease was different from lymphoma and described it first as malignant bone endothelioma.1,2
Angervall and Enzinger identified that the tumor could occur in deep soft tissue, and rarely in the skin.5 Later, cytogenetic studies confirmed that these tumors belong to the same family as Ewing's Sarcoma that arises from the bone, commonly called tumors of the Ewing's Sarcoma family (ESFT).7 Until 2001, only 78 cases were described in the literature; Most patients are white, female (2: 1) and in the second decade of life (average age of 16-17 years old). Translocation in the EWSR1 gene on chromosome 22q12 has been demonstrated, as well as in situ fluorescence hybridization / EWSR1 with a positive break for the translocation of EWSR1.1,2,6
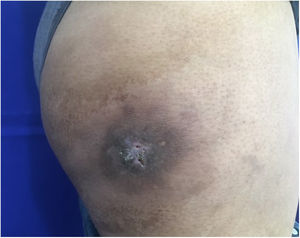
Clinical caseA 25-year old female with 22-days postpartum consulted presenting a 7-month history of a rapidly growing mass on the right thigh. The patient indicates fatigue and associated pain and bleeding of the mass. Physical examination revealed a 5-cm firm erythematous mass, with hematic crust on the surface surrounded with a peau d'orange erythematous halo. (Fig. 1).
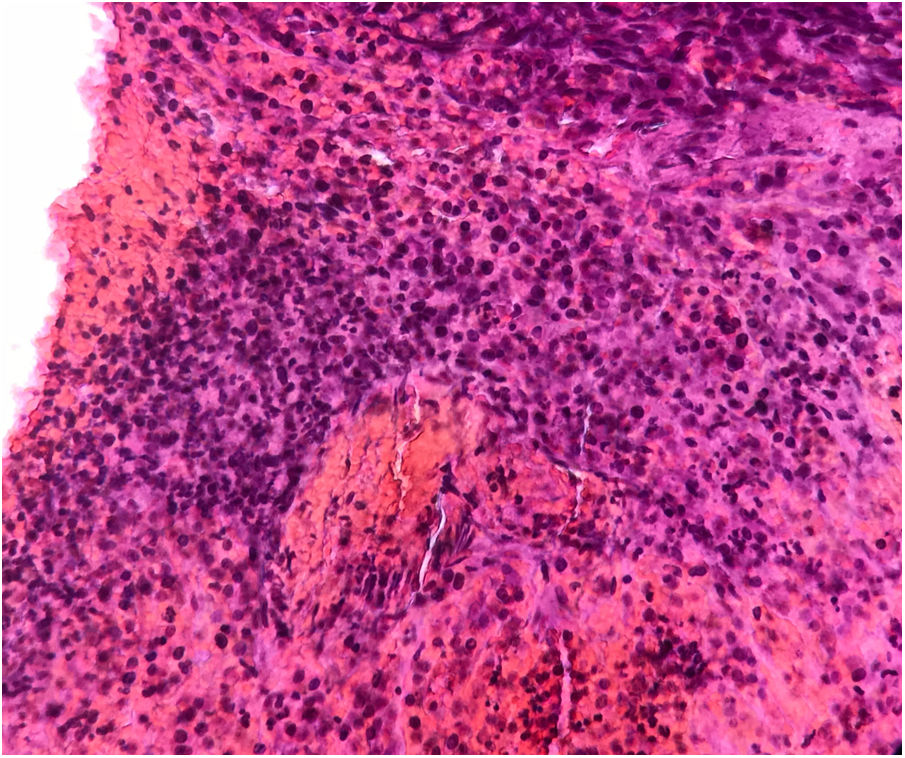
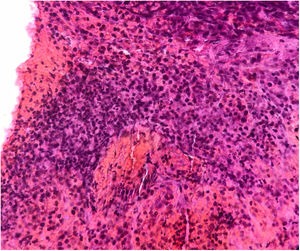
A punch biopsy was performed showing a basophilic small-cell tumor, with scarce cytoplasm, prominent nucleus, and chromatin, cells arranged in blankets throughout the thickness of the dermis without epidermal compromise (Fig. 2). Immunohistochemical study was positive for CD99, PKC, and Vimentin; and negative for actin, desmin, S100, chromogranin, CD20, CD3 and CK20. Thoracic CT revealed a 5 mm solid non-calcic nodule at the base of the left lung, suspected as metastasis, and left pachypleuritis. Abdominal CT showed hepatomegaly at the expense of the right lobe, without dilatation of bile ducts, no solid or cystic masses in the parenchyma where shown. Splenomegaly with a hypodense heterogeneous image, no greater than 25 mm was found, also suspected as metastasis. A diagnosis of Primitive Neuroectodermal Tumor: Ewing's Primary Cutaneous Sarcoma was given. The patient was referred to a social-security hospital where she received one induction cycle with vincristine and doxorubicin obtaining 50% reduction of the mass. Following two cycles without vincristine because supplies ran out. Bleeding presented with the third cycle, therefore radiotherapy was indicated (linear accelerator). Six months later, there is a 90% reduction in the skin lesion (Fig. 3). Lamentably, the patient died two weeks after the last dermatology appointment.
DiscussionThe Ewing's Sarcoma tumor family conventionally includes three significant entities: Ewing's sarcoma, Askin's tumor of the chest wall, and PNET.1,7
Ewing's Sarcoma is a primitive neuroectodermal tumor that rarely occurs in the skin and subcutaneous tissue. 85% of tumors present EWSR1 gene fusion with an erythroblastosis virus-transforming gene (FLI1); the fusion of exon 7 from EWSR1 to exon 6 of FLI1 translocation is specific to Ewing's Sarcoma.1 In general, it is better known as a primary bone tumor with a higher incidence in children than in adults. It is the second most common primary bone tumor in children and adolescents.2,7 Ewing's sarcoma has a low frequency, described mostly in the deep soft tissues of the paraspinal region, the chest wall or the lower extremities. The most superficial cases, called cutaneous, are sporadic and the vast majority of these have been reported as a single, small mass.1,2
Histologically, these sarcomas are composed mainly of small, round tumoral cells that generally express CD99 and weak positivity for synaptophysin markers.3–6,8 Some small round cell pediatric tumors with skin involvement can be easily ruled out by immunohistochemistry. Rhabdomyosarcoma may show positivity for CD99, but it also stains muscle markers such as desmin, myogenin, and myo-D1, while tumors of the Ewing's Sarcoma family do not.6–8 Lymphoblastic lymphoma may have skin involvement and often shows CD99 immunostaining but also Tdt stain, whereas the Tumor of the Ewing's Sarcoma family is always negative.2,4,6,7
Primary Cutaneous Ewing Sarcoma is a rare entity, currently treated in the same way as Ewing's Sarcoma of bone using extensive surgery, radiotherapy, and multi-drug chemotherapy.1,4 The cutaneous disease presents a slow course and a favorable prognosis, with a survival rate of 91% in ten years, compared with Ewing sarcoma of bone or soft tissue, which have a worse prognosis. The less aggressive behavior of the cutaneous clinical picture probably occurs due to superficial location, smaller tumors, and easy access; allowing detection through routine clinical examination or by the patient providing early diagnosis and complete surgical resection, avoiding the onset of metastasis.1,2,4,7 If the disease is detected early and managed with local excision and systemic chemotherapy, the result is favorable. Nowadays there is no scientific literature that proves a direct and causal relation between Primary Cutaneous Ewing's Sarcoma and Pregnancy. Unfortunately, as the case we present, 11% of cases of primary cutaneous Ewing sarcoma have described metastatic disease during the presentation.6–8
Please cite this article as: Posada M, Villalta G, Roldán MS, Sarti H. Sarcoma de Ewing Cutáneo Primario en una Paciente Embarazada: informe de un caso caso. Actas Dermosifiliogr. 2021;112:382–383.