A 68-year-old man presented with scaly lesions on an erythematous base on the cheeks, nose, and forehead.
Physical ExaminationPhysical examination revealed lesions consistent with actinic keratoses in the aforementioned areas, notably an erythematous plaque with atrophic areas and superficial telangiectasias on the right side of the nose (Fig. 1). The patient stated that several years earlier he had been treated in that area with topical imiquimod for a lesion whose diagnosis we were unable to ascertain because the treatment had been administered at a different healthcare facility. The patient reported itching and a burning sensation in the area, which worsened with sun exposure.
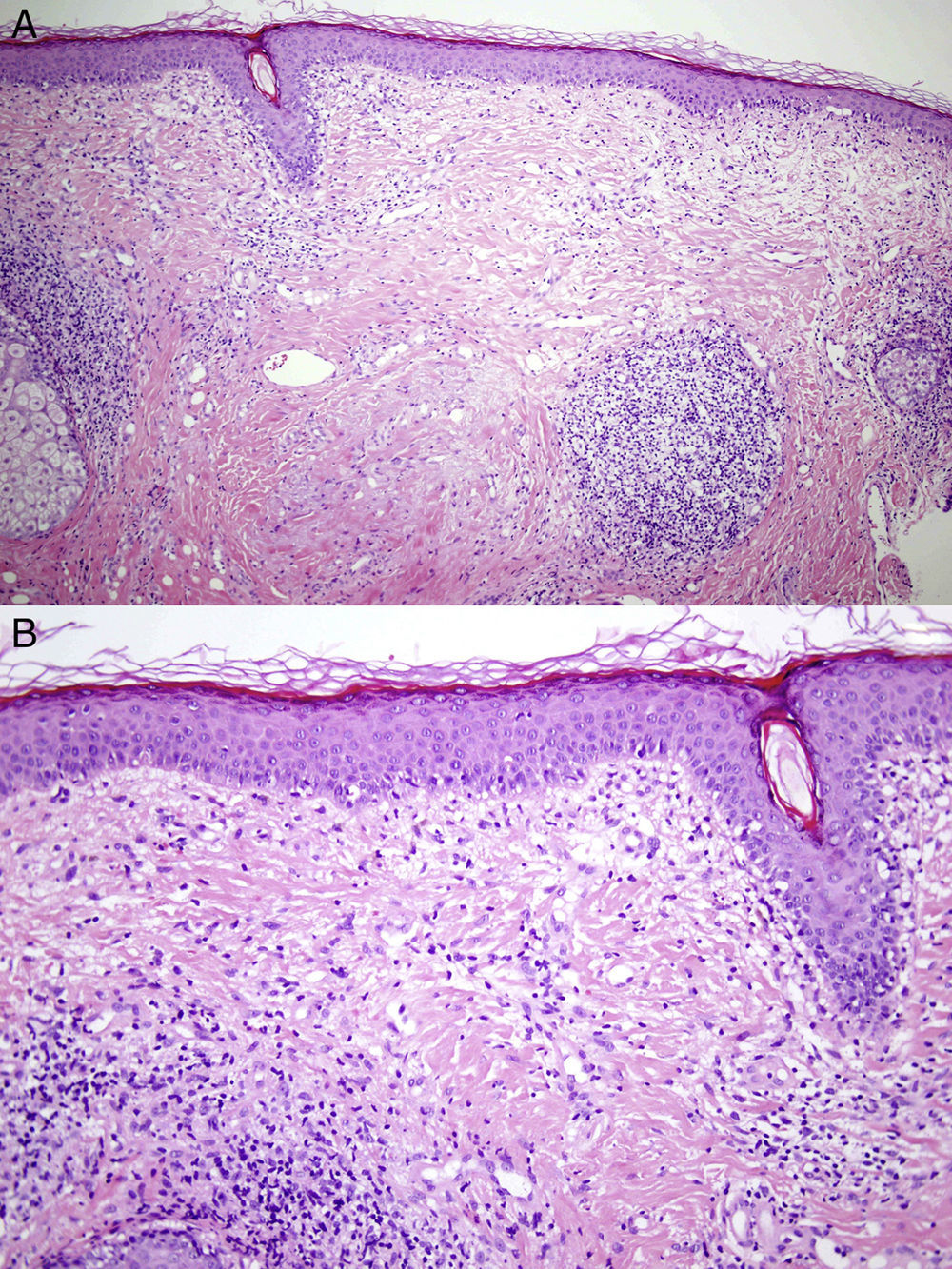
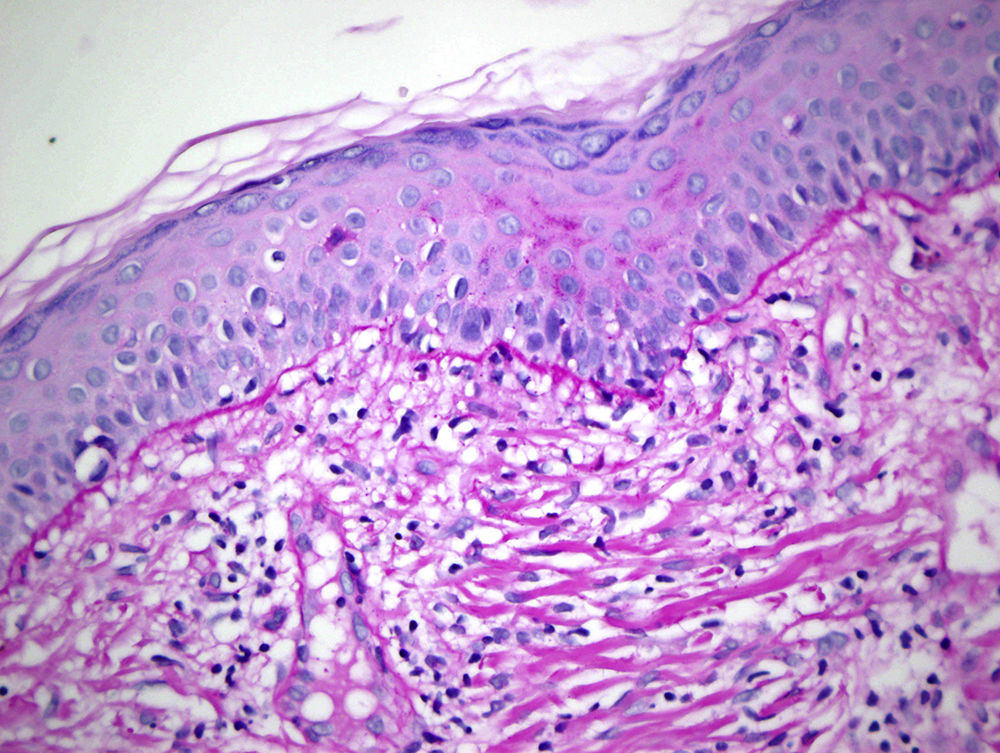
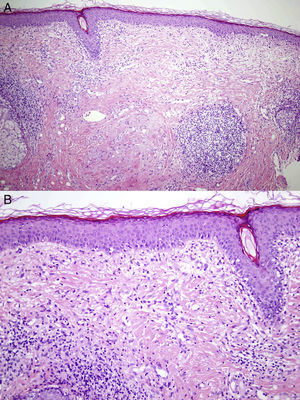
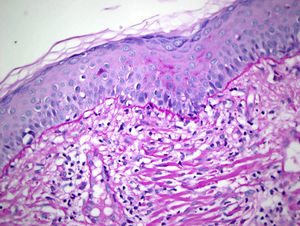
HistopathologyBiopsy revealed a flattened epidermis that had an atrophic appearance in some areas, with vacuolar degeneration of the basal layer, which contained necrotic keratinocytes. The dermis was edematous, with a proliferation of capillaries and activated fibroblasts. A perivascular and periadnexal lymphohistiocytic infiltrate was observed in both the superficial and deep layers (Figs. 2A and 2B). Colloidal iron staining showed no mucin deposits and periodic acid–Schiff staining revealed a moderate thickening of the basement membrane (Fig. 3). The results of the complete blood count, coagulation study, blood biochemistry including glucose, kidney function, liver function, acute phase reactants, and antinuclear antibodies were within the normal range.
What Is Your Diagnosis?
DiagnosisLupus-like reaction in imiquimod-treated skin.
Clinical Course and TreatmentSun protection measures were recommended and treatment was started with topical mometasone, applied once daily for 3 weeks, after which maintenance therapy with 0.1% topical tacrolimus was started, with clinical and symptomatic improvement.
DiscussionImiquimod is a topical immunomodulator approved for the treatment of condylomata acuminata, actinic keratoses, and superficial basal cell carcinomas. It is also used off-label in Bowen disease and lentigo maligna. Various clinical and histologic skin reactions such as lichenoid reactions, psoriasiform reactions, vitiligo, alopecia, and urticaria have been described.1 To date, there have been 3 reports of histologic lupus-like reaction in imiquimod-treated skin, but clinically the lesions did not resemble lupus lesions at all.2,3 After the imiquimod penetrates the epidermis, it binds to macrophages and dermal dendritic cells via toll-like receptor 7 and releases interferon alfa, tumor necrosis factor, and interleukins 2, 6, and 8, among other proinflammatory cytokines. It has been postulated that interface dermatitis could be caused by an interferon alfa–mediated cytotoxic attack on the basal keratinocytes,3 and there have been numerous reports of lupus-like lesions at the injection sites of subcutaneous interferon alfa treatment.4,5 The term interface dermatitis refers to a process in which an inflammatory infiltrate composed mainly of lymphocytes develops at the dermoepidermal junction. Other typical findings are vacuolar changes along the dermoepidermal junction, the presence of necrotic keratinocytes, and spongiosis (usually mild). Interface dermatitis can be classified according to the density of the infiltrate: in vacuolar interface dermatitis the inflammation is mild, whereas in lichenoid interface dermatitis a dense band-like infiltrate is present. Erythema multiforme is considered the prototype of vacuolar interface dermatitis, but the differential diagnosis should also include autoimmune connective tissue diseases such as systemic lupus erythematosus, dermatomyositis, and mixed connective tissue disease, as well as graft-versus-host disease, certain viral rashes, and some drug-induced reactions. One clue to distinguishing a lupus-like reaction in imiquimod-treated skin from true systemic lupus erythematosus is that no mucin deposits are present in the former.1,2 Each case of lupus-like reaction in imiquimod-treated skin reported to date has had a different set of clinical characteristics, but our case is the only one that clinically resembles cutaneous lupus erythematosus (in fact, lupus pernio and lupus vulgaris were considered in the differential diagnosis).
We present a case of a clinically and histologically lupus-like reaction in imiquimod-treated skin. This reaction is a rare side effect of topical imiquimod that must be taken into account in order to avoid the misdiagnosis of cutaneous lupus erythematosus.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Fernández DG, López SR, Pineda FV. Lesión eritematosa nasal. Actas Dermosifiliogr. 2018;109:173–174.