Confluent and reticulated papillomatosis, also known as Gougerot-Carteaud Syndrome, is a rare chronic disease typically affecting young adults. Of unknown etiology, the condition is characterised by oval grayish-brown or erythematous papules that coalesce to form a reticular pattern, usually on the trunk, especially in the intermammary or interscapular region and on the neck. Diagnosis is primarily clinical, based on the appearance of the lesions, the areas affected, and the response to treatment with minocycline. We report 20 cases of patients with histologically confirmed confluent and reticulated papillomatosis who presented linear pseudo-striae, a little known diagnostic sign.
La papilomatosis confluente y reticulada, o síndrome de Gougerot y Carteaud, es una enfermedad infrecuente, crónica, de etiología desconocida, que se presenta habitualmente en adultos jóvenes y se caracteriza por placas pardo-eritematosas ovales, que confluyen en un patrón reticulado y afectan el tronco, particularmente la región intermamaria e interescapular, y el cuello. Su diagnóstico es fundamentalmente clínico, se basa en la localización y el aspecto de las lesiones, así como en la respuesta al tratamiento con minociclina. Presentamos 20 casos de papilomatosis confluente y reticulada, confirmados por histopatología, en quienes se identificó la presencia de pseudoestrías lineales, un hallazgo semiológico poco reconocido.
Confluent and reticulated papillomatosis is an uncommon chronic disease of unknown etiology. It has been reported in various populations and races, with a slight predominance in women (1.4:1) and individuals with dark skin types.1,2 In general, the disease first appears during young adulthood, although it can appear at any age.3–5 Between the years 2011 and 2015, we diagnosed 93 new cases of this disease (incidence, 0.03 cases per 100 new patients per year) at a reference dermatology center in Bogotá, Colombia. The city of Bogotá is situated at an altitude of 2630m and has an average temperature of 14°C with a cold tropical savanna climate. Patients in the case series had fine shiny plaques with areas of “cigarette paper–like” skin that gave the impression of linear pseudo-striae, which play an important role in guiding clinical diagnosis.
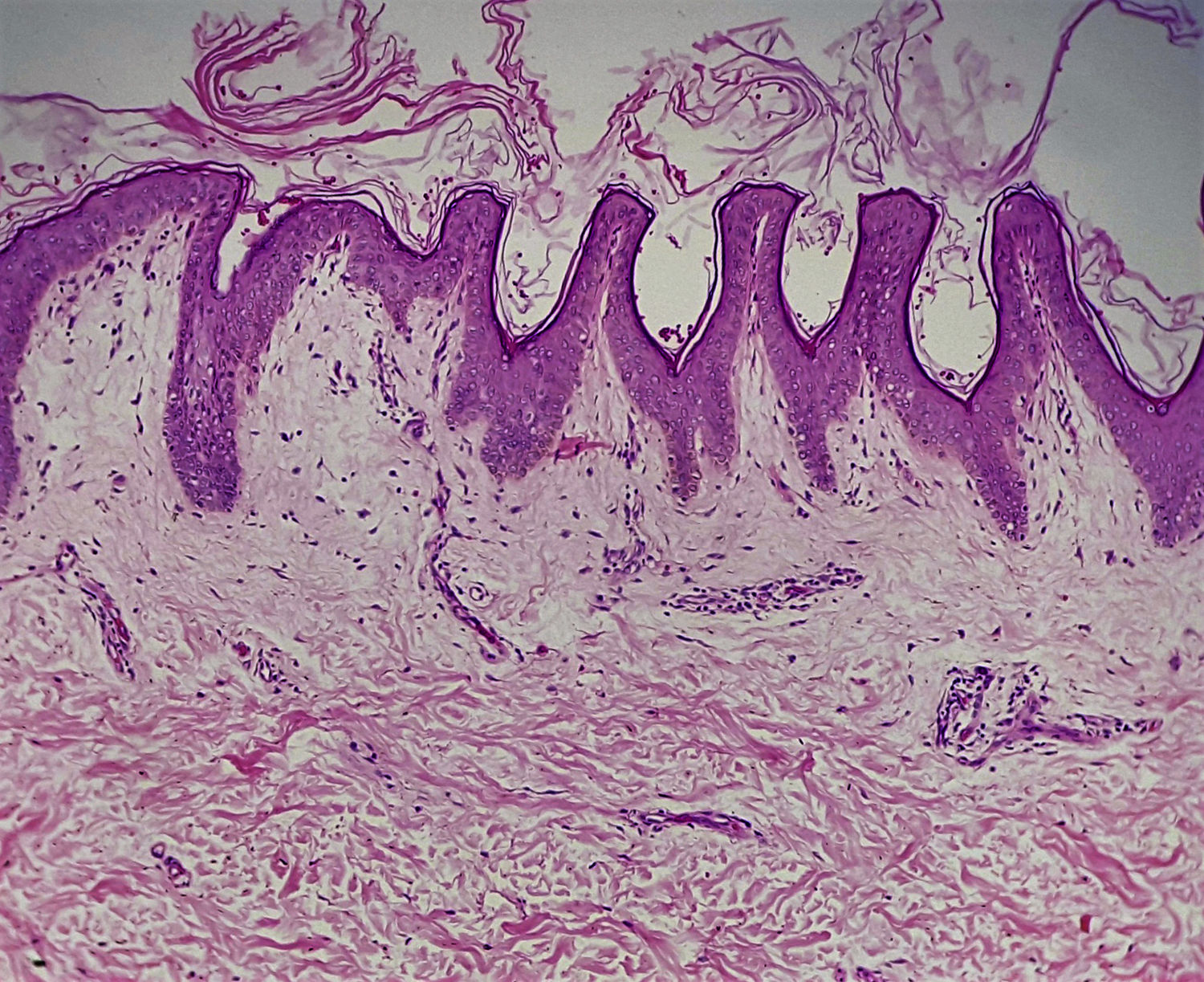
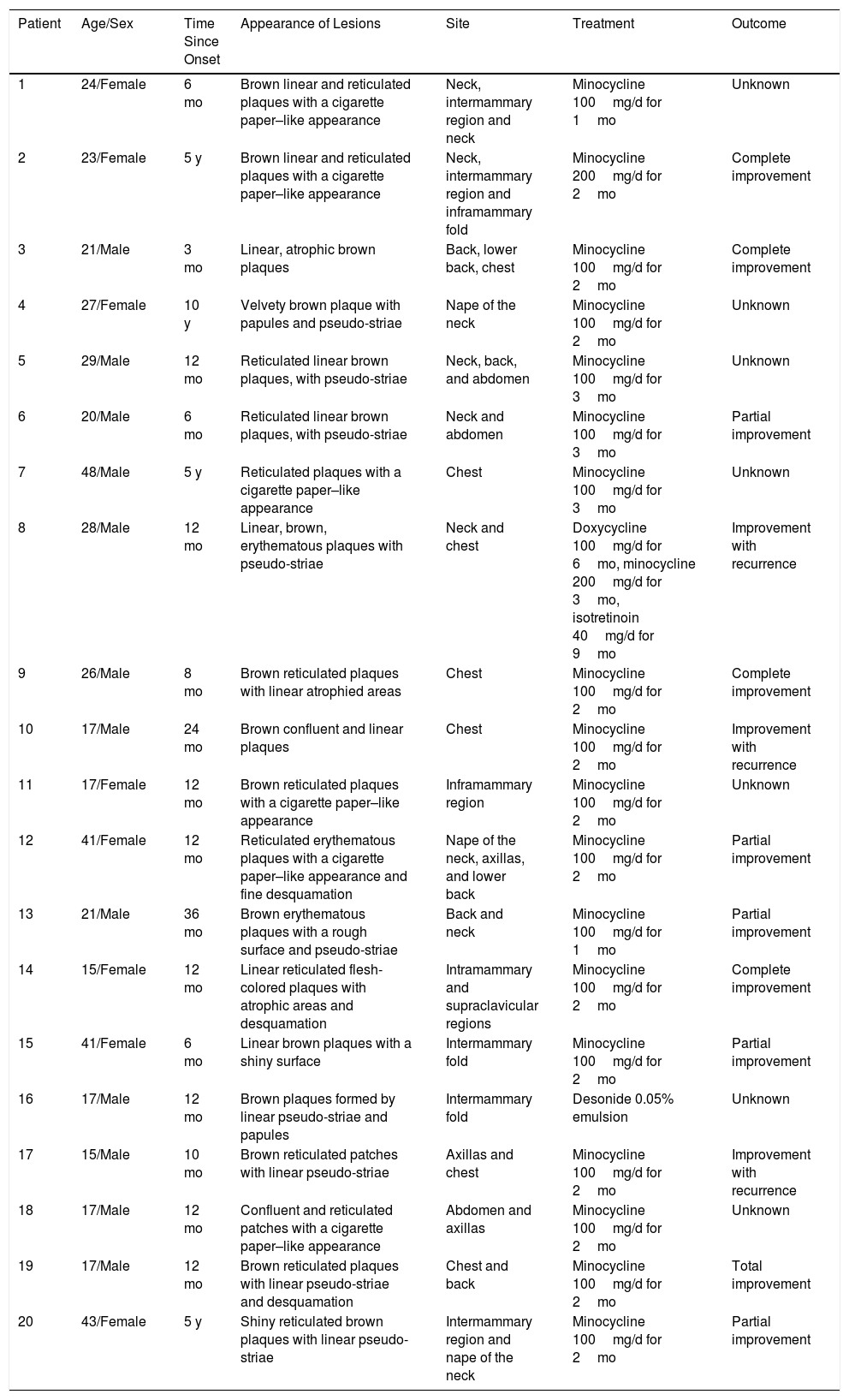
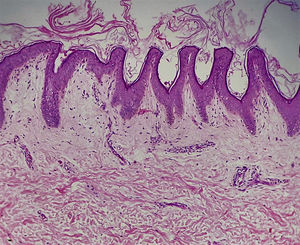
Case DescriptionsThe series comprised 9 females (45%) and 11 males (55%) of mixed ethnicity who were from Bogotá. They were aged 15 to 48 years (mean, 24 years) and had asymptomatic lesions on the chest (75%) and neck (45%) that had first appeared an average of 2 years previously. In addition to the brown plaques that are characteristic of the disease (100%), the patients also had linear pseudo-striae (Table 1). All patients underwent skin biopsy, which made it possible to confirm the diagnosis. The most frequent findings were epidermis with hyperkeratosis, melanin deposits in the basal layer, acanthosis, and papillomatosis of the rete ridges, with perivascular infiltration of the dermis.
Epidemiological Characteristics, Clinical Manifestations, and Treatment.
| Patient | Age/Sex | Time Since Onset | Appearance of Lesions | Site | Treatment | Outcome |
|---|---|---|---|---|---|---|
| 1 | 24/Female | 6 mo | Brown linear and reticulated plaques with a cigarette paper–like appearance | Neck, intermammary region and neck | Minocycline 100mg/d for 1mo | Unknown |
| 2 | 23/Female | 5 y | Brown linear and reticulated plaques with a cigarette paper–like appearance | Neck, intermammary region and inframammary fold | Minocycline 200mg/d for 2mo | Complete improvement |
| 3 | 21/Male | 3 mo | Linear, atrophic brown plaques | Back, lower back, chest | Minocycline 100mg/d for 2mo | Complete improvement |
| 4 | 27/Female | 10 y | Velvety brown plaque with papules and pseudo-striae | Nape of the neck | Minocycline 100mg/d for 2mo | Unknown |
| 5 | 29/Male | 12 mo | Reticulated linear brown plaques, with pseudo-striae | Neck, back, and abdomen | Minocycline 100mg/d for 3mo | Unknown |
| 6 | 20/Male | 6 mo | Reticulated linear brown plaques, with pseudo-striae | Neck and abdomen | Minocycline 100mg/d for 3mo | Partial improvement |
| 7 | 48/Male | 5 y | Reticulated plaques with a cigarette paper–like appearance | Chest | Minocycline 100mg/d for 3mo | Unknown |
| 8 | 28/Male | 12 mo | Linear, brown, erythematous plaques with pseudo-striae | Neck and chest | Doxycycline 100mg/d for 6mo, minocycline 200mg/d for 3mo, isotretinoin 40mg/d for 9mo | Improvement with recurrence |
| 9 | 26/Male | 8 mo | Brown reticulated plaques with linear atrophied areas | Chest | Minocycline 100mg/d for 2mo | Complete improvement |
| 10 | 17/Male | 24 mo | Brown confluent and linear plaques | Chest | Minocycline 100mg/d for 2mo | Improvement with recurrence |
| 11 | 17/Female | 12 mo | Brown reticulated plaques with a cigarette paper–like appearance | Inframammary region | Minocycline 100mg/d for 2mo | Unknown |
| 12 | 41/Female | 12 mo | Reticulated erythematous plaques with a cigarette paper–like appearance and fine desquamation | Nape of the neck, axillas, and lower back | Minocycline 100mg/d for 2mo | Partial improvement |
| 13 | 21/Male | 36 mo | Brown erythematous plaques with a rough surface and pseudo-striae | Back and neck | Minocycline 100mg/d for 1mo | Partial improvement |
| 14 | 15/Female | 12 mo | Linear reticulated flesh-colored plaques with atrophic areas and desquamation | Intramammary and supraclavicular regions | Minocycline 100mg/d for 2mo | Complete improvement |
| 15 | 41/Female | 6 mo | Linear brown plaques with a shiny surface | Intermammary fold | Minocycline 100mg/d for 2mo | Partial improvement |
| 16 | 17/Male | 12 mo | Brown plaques formed by linear pseudo-striae and papules | Intermammary fold | Desonide 0.05% emulsion | Unknown |
| 17 | 15/Male | 10 mo | Brown reticulated patches with linear pseudo-striae | Axillas and chest | Minocycline 100mg/d for 2mo | Improvement with recurrence |
| 18 | 17/Male | 12 mo | Confluent and reticulated patches with a cigarette paper–like appearance | Abdomen and axillas | Minocycline 100mg/d for 2mo | Unknown |
| 19 | 17/Male | 12 mo | Brown reticulated plaques with linear pseudo-striae and desquamation | Chest and back | Minocycline 100mg/d for 2mo | Total improvement |
| 20 | 43/Female | 5 y | Shiny reticulated brown plaques with linear pseudo-striae | Intermammary region and nape of the neck | Minocycline 100mg/d for 2mo | Partial improvement |
Potassium hydroxide 10% (KOH solution) staining for fungi was carried out in 4 cases (20%) and yielded a negative result.
Treatment with minocycline was successful in 13 patients (65%), 3 of whom (23%) relapsed when the medication was suspended.
CommentConfluent and reticulated papillomatosis was described in 1927 by Henri Gougerot and Alexander Carteaud.1,3 Its etiology remains unclear, although several theories have been put forward, including keratinization disorders,1,4 abnormal response to infection by yeasts of the genus Malassezia furfur,1,2,6 endocrinopathies,2,4 bacterial infection by a species of the genus Dietzia,7 and genetic factors.4
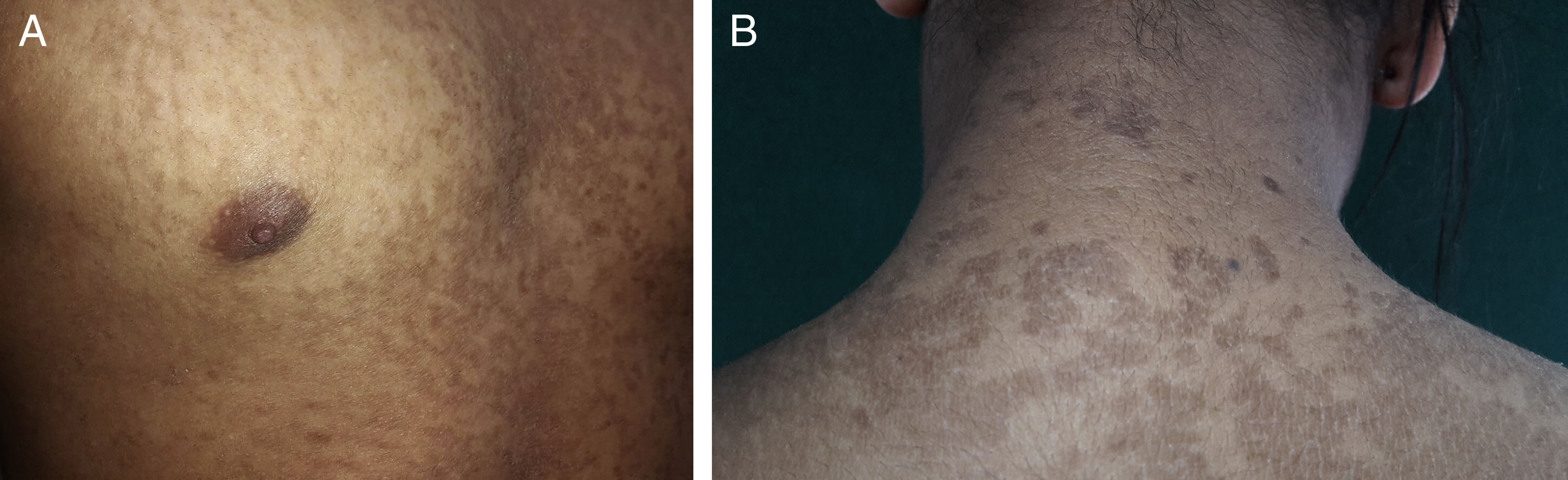
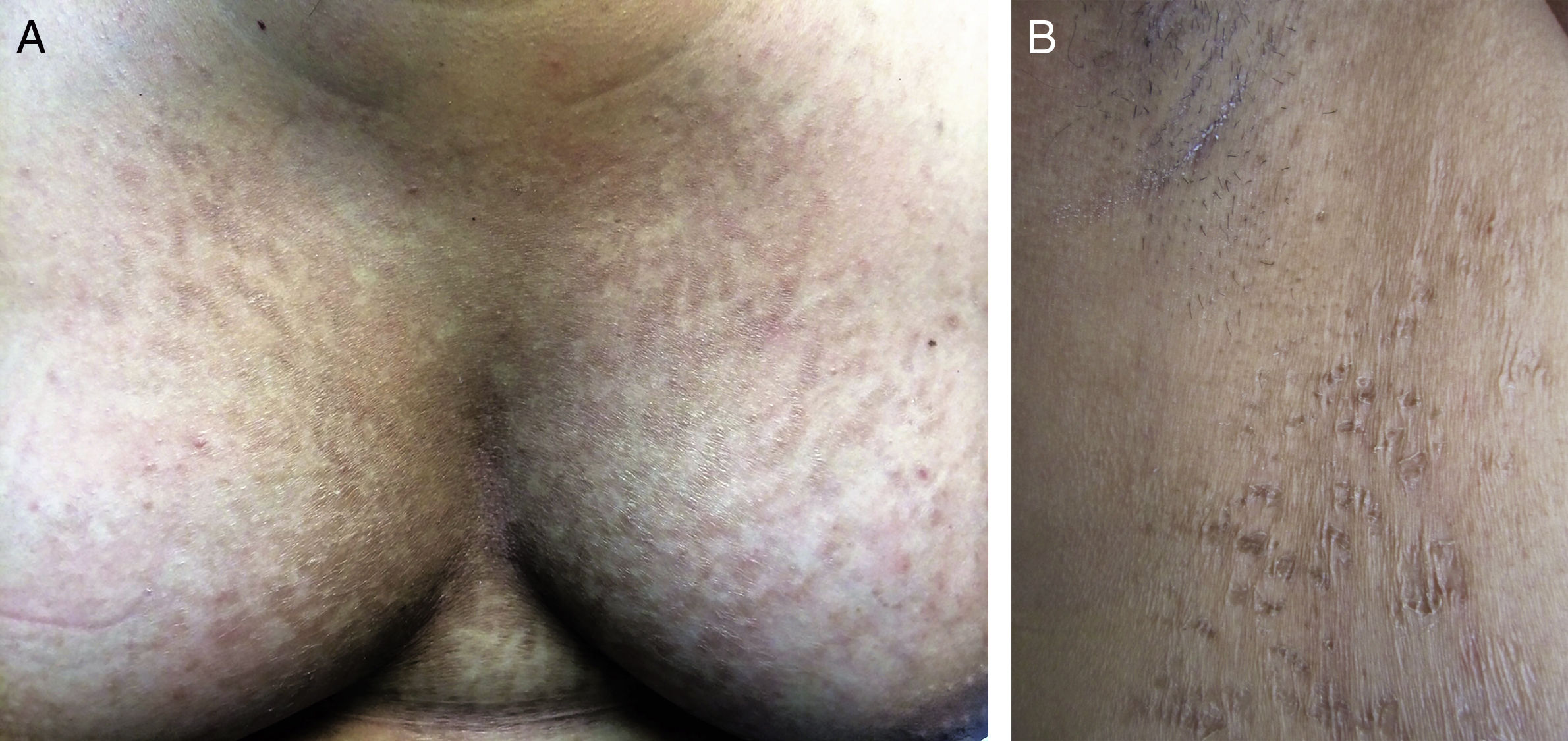
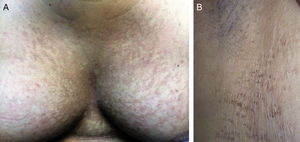
Clinically, the condition presents as erythematous papules measuring 1-2mm in diameter that can reach 5mm. They subsequently turn brown and coalesce to form plaques with a reticular pattern on the periphery,1,2,5 such as those observed in the series reported here (Fig. 1). They are usually found on the intermammary and interscapular regions, followed by the neck, abdomen, and axillas,4 and exceptionally on the forehead, elbows, knees, and ankles.8,9 In the present series, the lesions were observed on the nape of the neck and on the lower back, in addition to the usual sites (Table 1). However, the main finding was the presence of thin shiny plaques with wrinkled cigarette paper–like appearance that gave the impression of linear pseudo-striae (Fig. 2), which play an important role in guiding clinical diagnosis. Despite being described in the literature,1,10 this finding is unknown by most clinicians.
Histologically, as reported in the present series, common findings include hyperkeratosis, papillomatosis, hypogranulosis, and a stratum spinosum with involvement ranging from acanthosis to atrophy3–5 (Fig. 3), thus explaining the formation of pseudo-striae. We also observed increased melanin deposits in the basal layer and perivascular lymphohistiocytic infiltration in the superficial dermis, which has been reported in the literature.11
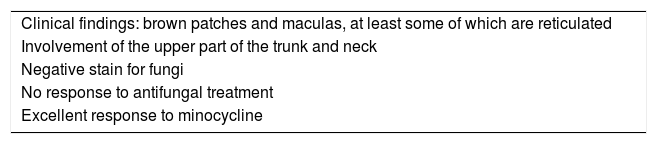
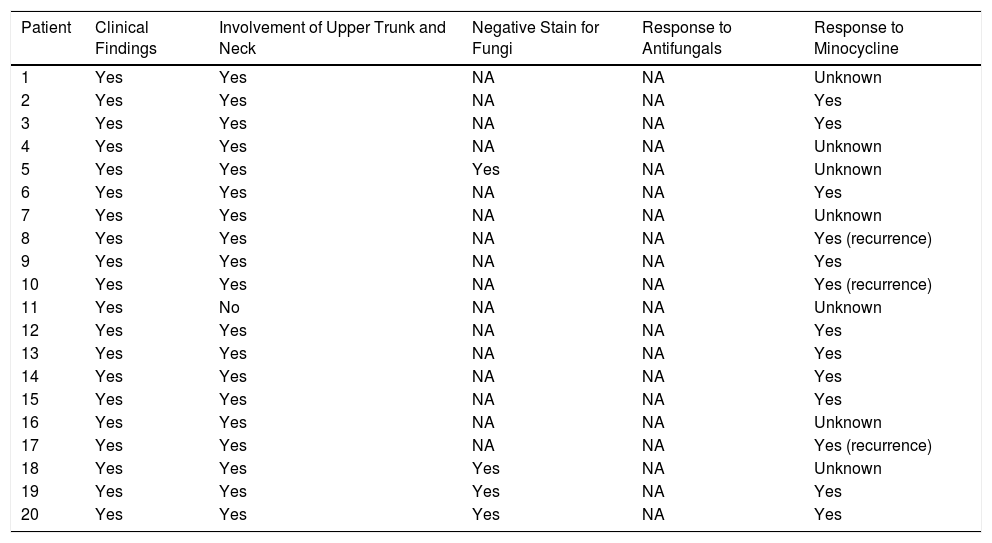
In 2006, Davis et al.,12 suggested a series of diagnostic criteria for confluent and reticulated papillomatosis (Table 2), which have been accepted by several authors.5,12,13 The first 2 criteria—reticulated brown patches and macules and involvement of the upper trunk and neck—were fulfilled in all the cases in the present series, with the exception of 1 patient, whose brown patches were observed only on the inframammary fold (Table 3). Plaques were the predominant lesion, probably because the average time since onset was 2 years at consultation. The third criterion—negative staining for fungi—was only reported in 4 patients with suspected pityriasis versicolor, one of the main differential diagnoses in cases of hypopigmented lesions5,14 or furfuraceous desquamation. Other differential diagnoses include acanthosis nigricans,5,15 ichthyosis vulgaris, seborrheic dermatitis, Darier disease, ashy dermatitis, pigmented contact dermatitis, livedo reticularis, and prurigo pigmentosa.1
Diagnostic Criteria Proposed by Davis et al12
| Clinical findings: brown patches and maculas, at least some of which are reticulated |
| Involvement of the upper part of the trunk and neck |
| Negative stain for fungi |
| No response to antifungal treatment |
| Excellent response to minocycline |
Characteristics of Patients From the Series According to the Diagnostic Criteria of Davis et al12
| Patient | Clinical Findings | Involvement of Upper Trunk and Neck | Negative Stain for Fungi | Response to Antifungals | Response to Minocycline |
|---|---|---|---|---|---|
| 1 | Yes | Yes | NA | NA | Unknown |
| 2 | Yes | Yes | NA | NA | Yes |
| 3 | Yes | Yes | NA | NA | Yes |
| 4 | Yes | Yes | NA | NA | Unknown |
| 5 | Yes | Yes | Yes | NA | Unknown |
| 6 | Yes | Yes | NA | NA | Yes |
| 7 | Yes | Yes | NA | NA | Unknown |
| 8 | Yes | Yes | NA | NA | Yes (recurrence) |
| 9 | Yes | Yes | NA | NA | Yes |
| 10 | Yes | Yes | NA | NA | Yes (recurrence) |
| 11 | Yes | No | NA | NA | Unknown |
| 12 | Yes | Yes | NA | NA | Yes |
| 13 | Yes | Yes | NA | NA | Yes |
| 14 | Yes | Yes | NA | NA | Yes |
| 15 | Yes | Yes | NA | NA | Yes |
| 16 | Yes | Yes | NA | NA | Unknown |
| 17 | Yes | Yes | NA | NA | Yes (recurrence) |
| 18 | Yes | Yes | Yes | NA | Unknown |
| 19 | Yes | Yes | Yes | NA | Yes |
| 20 | Yes | Yes | Yes | NA | Yes |
Abbreviation: N/A, not available.
Furthermore, given the histologic confirmation of confluent and reticulated papillomatosis, no patients were treated with antifungal agents; therefore, this criterion could not be evaluated.
Although several therapeutic options have been proposed, oral antibiotics are the treatment of choice.13 Therapy has been successful with at least 1 cycle of azithromycin, clarithromycin, and tetracyclines,3 although minocycline is the treatment preferred by various authors.2,3,5,13 When minocycline is administered orally at 100mg/d, an improvement of more than 70% is reported, with resolution of lesions at 1 or 2 months.2 Of the 13 cases in the present series that responded to minocycline, 5 had a 100% improvement, 5 a partial improvement, and 3 a relapse after suspending therapy (Table 1). Given that recurrences are frequent, some authors recommend larger doses in several cycles.2,12
In 2014, Jo et al.13 updated the Davis criteria by including flexural involvement and response not only to minocycline, but to all antibiotics.
ConclusionConfluent and reticulated papillomatosis is an uncommon condition that is easily confused with other skin complaints that have similar clinical manifestations, such as acanthosis nigricans and pityriasis versicolor. We present a series of cases in which the identification of linear pseudo-striae, a characteristic yet little known clinical diagnostic sign, which was subsequently confirmed by skin biopsy.
Ethical DisclosuresProtection of humans and animalsThe authors declare that no tests were carried out in humans or animals for the purposes of this study.
Confidentiality of dataThe authors declare that they have followed their institutional protocols on publication of patient data.
Right to privacy and informed consentThe authors obtained the informed consent of the patients and/or participants referred to in the present article. The signed forms are in the possession of the corresponding author.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Morales-Cardona CA, Tejada-Figueroa C, Méndez-Velasco DM. Papilomatosis confluente y reticulada con pseudoestrías lineales: descripción de 20 casos. Actas Dermosifiliogr. 2018;109:e7–e11.