Platelet rich plasma (PRP) is a source of growth factors recently introduced to treat androgenetic alopecia (AGA) with conflicting results. Our aims are to assess the efficacy of PRP in increasing hair density in males with AGA, and to investigate a correlation between positive response and each of patient's age and type and duration of AGA.
Materials & MethodsThis before and after study included 30 males with no history of hair treatments for at least 3 months prior to our study. Each patient received 3 injections at one-month intervals. Scalp hair density of each subject was measured manually by a dermatoscope before and following 2 and 6 months of the first intervention. Data were compared to evaluate efficacy.
ResultsHair density was increased by 19.17% following our intervention (172.46 ± 59.04 hairs/cm2 before treatment to 205.53 ± 68.20 hairs/cm2 after 6 months) with minimal short-term side effects. Type III vertex was the least responsive pattern and no correlation was observed between positive response and either patient's age or duration of AGA.
ConclusionPRP injections for men with AGA has a positive effect on hair density.
el plasma rico en plaquetas (PRP) es una fuente de factores de crecimiento utilizada recientemente en el tratamiento de la alopecia androgenética (AGA); sin embargo, la eficacia de este tratamiento sigue siendo controversial. Los objetivos del presente estudio son evaluar la eficacia del PRP en el incremento de la densidad capilar en varones con AGA, así como, determinar si existe una correlación entre la respuesta favorable a dicho tratamiento, con la edad del paciente, con el tipo de AGA y con el tiempo de evolución de esta.
Materiales y métodosSe diseño un estudio de “antes/después” y se incluyeron 30 varones. Estos pacientes no habían recibido ningún tratamiento para la AGA al menos en los 3 meses previos al estudio. Cada paciente recibió 3 inyecciones en intervalos de un mes. La densidad capilar de cada sujeto se midió manualmente mediante un dermatoscopio antes de la primera intervención y también a los 2 y 6 meses. Para determinar la eficacia del tratamiento se realizó un análisis comparativo.
ResultadosLa densidad capilar se incrementó en un 19.17% después de la intervención (172.46 ± 59.04 cabellos / cm2 antes del tratamiento a 205.53 ± 68.20 cabellos / cm2 después de los 6 meses); los efectos secundarios fueron mínimos en el seguimiento a corto plazo. El patrón de alopecia de tipo vertex III fue el patrón que presentó una menor respuesta. No se objetivó ninguna correlación entre la respuesta favorable al tratamiento y la edad del paciente o la duración de la AGA.
Conclusiónlas inyecciones de PRP en pacientes varones con AGA tendrán un efecto favorable sobre la densidad capilar.
Androgenetic alopecia (AGA) is characterized by progressive miniaturization of hair follicles in the scalp. In men, it is due mainly to androgens and genetic predisposition. Progressive hair loss leading to bald patches on the scalp occurs in 50% to 60% of men at the age of 70 years.1 AGA can lead to anxiety and depression, as baldness is associated with decreased physical attractiveness in some societies.1–2 Oral finasteride and topical minoxidil are the currently approved therapeutic options. However, both are associated with noteworthy side effects, and so there is a need to find other safer therapeutic options.3 The use of platelet rich plasma (PRP) for management of androgenetic alopecia has recently gained in popularity. PRP is a source of growth factors derived from a platelet concentrate obtained by centrifugation.4 However, the effectiveness of PRP in the treatment of androgenetic alopecia is still subject of debate, given that several studies have concluded that there is no scientific evidence to support PRP efficacy in the treatment of this condition.5 Therefore, in the present study, we investigated the actual efficacy of PRP injections as monotherapy in men diagnosed with AGA. Likewise, we sought to determine whether there is a correlation between favorable response to this treatment and patient age and type and duration of AGA.
Material and methodsTo answer the research question, a before and after study was designed. Thirty patients under 45 years of age were screened with diagnosis of AGA and no known history of malignant neoplasms, acquired immunodeficiency syndrome, hepatitis B, hepatitis C, or susceptibility to keloid scarring. Furthermore, none of the patients were receiving longstanding nonsteroidal antiinflammatory drugs or had active skin lesions in the areas affected by AGA. Our cohort of patients included all stages of alopecia according to the Norwood scale, except stage 6, 7, and 5a. Likewise, none of the patients had received any capillary treatment in the 3 months prior to the study. Finally, the baseline platelet count in patients had to be greater than 140,000 platelets per microliter (μL). After obtaining written informed consent, in accordance with the Ethics Committee of the University of Tishreen, Syria, an analysis of whole blood counts, liver enzymes, erythrocyte sedimentation rate, hepatitis B surface antigen, and hepatitis C antibodies was undertaken.
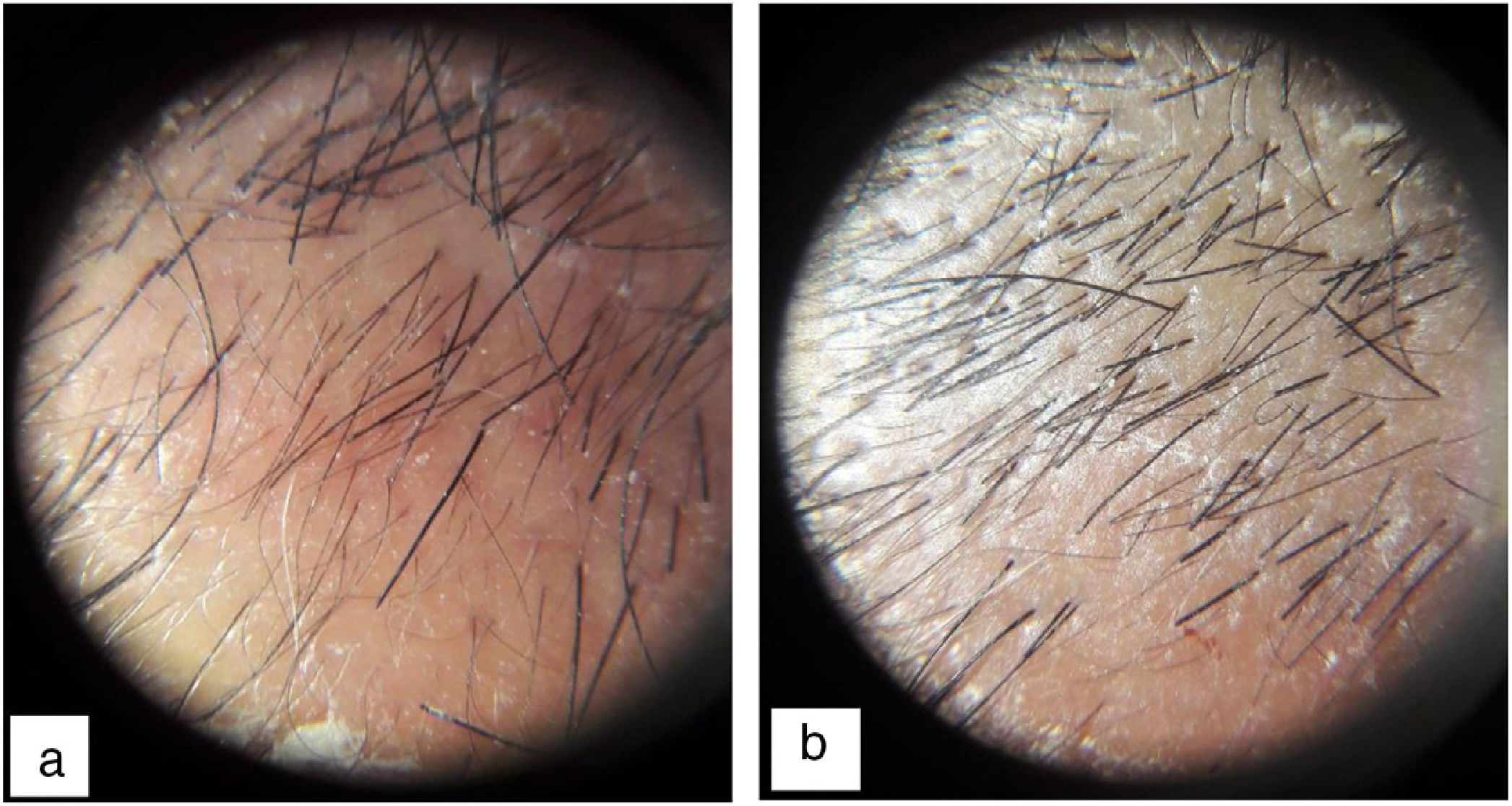
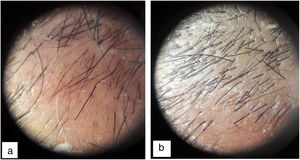
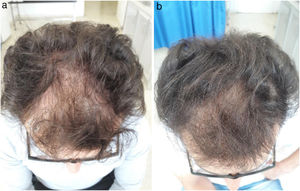
Each patient was examined to locate the area with lowest hair density. An area 1 cm2 was marked and the hair in that area shaved. A metric tape measure graduated in centimeters was used to mark the square centimeter and the longitudinal distance from the corresponding end of the eyebrow or nasal root was measured. The image of the area was then amplified using a dermatoscope (Heine mini 3000® LED Dermatoscope, Germany) and a photograph was taken before each injection. This photograph was transferred to the Microsoft program (Paint; version 6.1) and then amplified to permit manual counting by 3 observers. To avoid counting a given follicle twice, a red dot was placed on each hair immediately after counting.
PRP preparationPRP was prepared under sterile conditions, taking an 18 mL sample of peripheral blood. The sample was then divided into 2 parts. Each part (9 mL of blood) was transferred to a tube that contained 1 mL of sodium citrate 3.8% and then centrifuged at 800 revolutions per minute (rpm) for 15 min (Scilogex DM0412, New York, United States). Six milliliters of each supernatant layer, which contained 2.25 times the baseline platelet concentration, were extracted using a 20 caliber needle and placed in 6 insulin syringes.
Intradermal injections of PRP in the affected areas of the scalp were performed with the patients in sitting position. An area of 1 cm was left between each application. Local anesthetic was not needed. In total, 3 sessions were performed with an interval of 1 month between each one. Patients were assessed using dermatoscopy before each injection, as well as 2 and 6 months after the first injection, measuring capillary density manually, that is, hair follicle units were counted in the 1 cm2 marked previously. Response to treatment was considered positive if hair density had increased by more than 10 hairs/cm2 after 2 months.
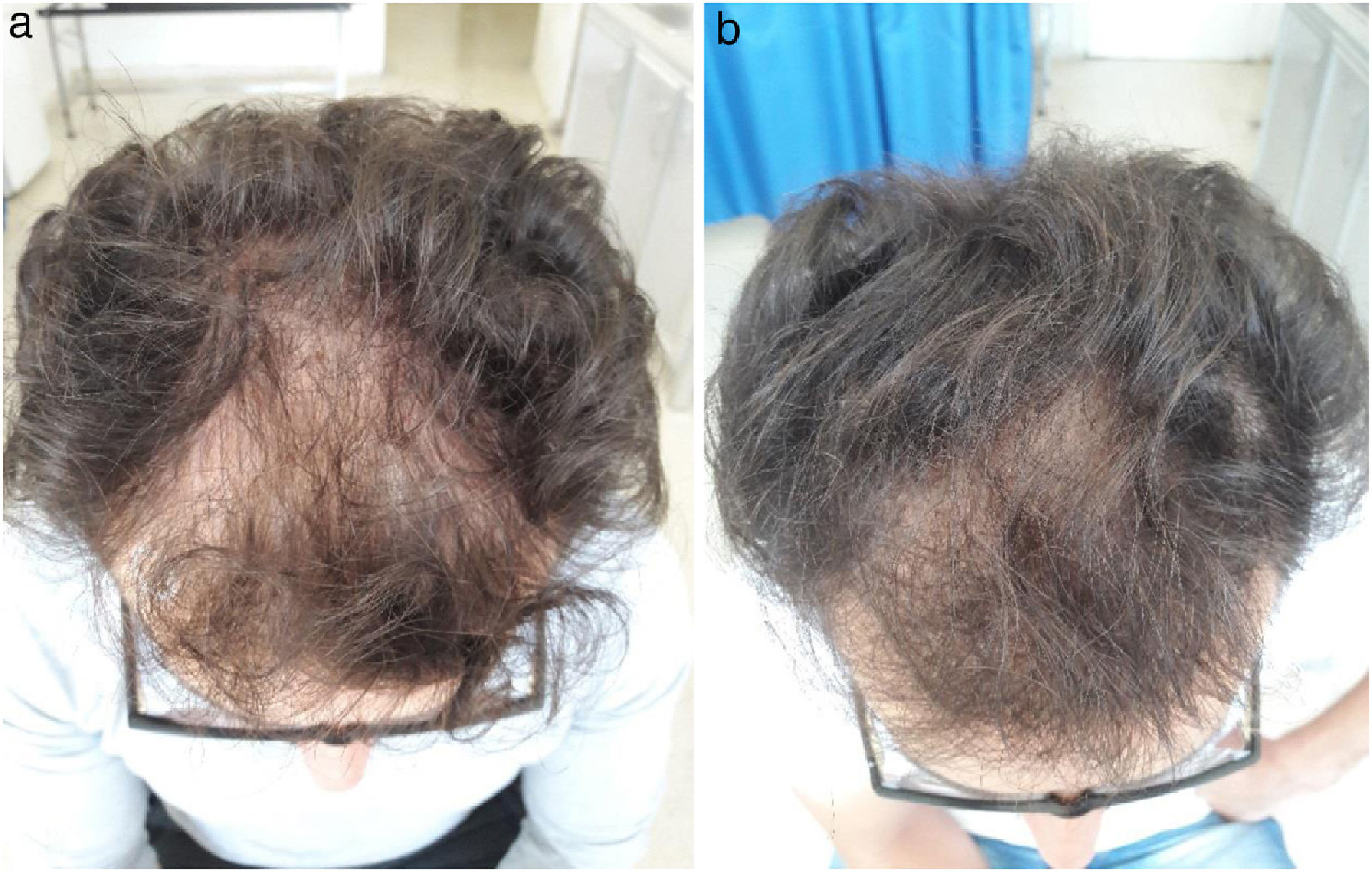
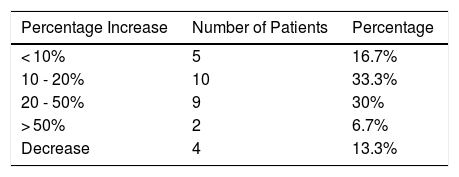
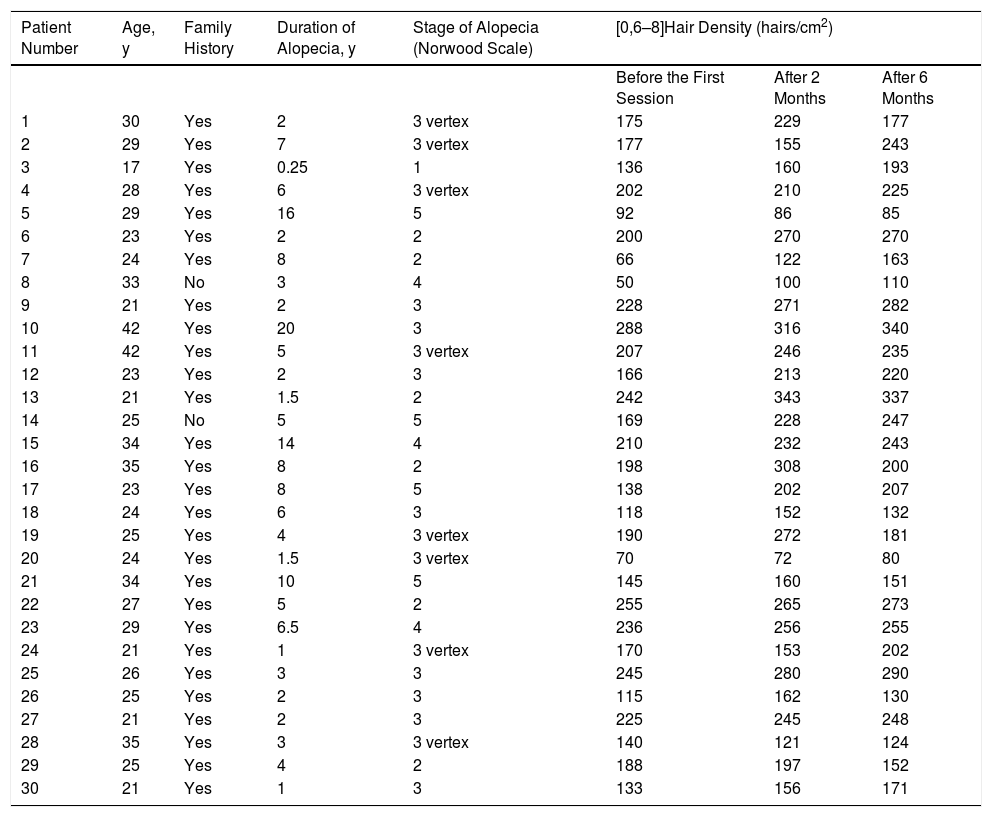
ResultsThirty-two men with diagnosis of AGA were selected between September 2017 and December 2018. Two patients were excluded, 1 because he was taking sodium diclofenac (NSAID) during the study period and the other because hepatitis C antibodies were detected in serum. Finally, a total of 30 patients were enrolled in the study. Our study cohort comprised patients aged between 17 and 42 years (mean 26.7 ± 4.7 years). Stage 3 and 3 vertex, according to the Norwood scale, were the most frequent patterns (8 patients each, that is, 26.7%). Twenty-eight patients (93.3%) had a family history of AGA. Hair density increased by 19.17% at 2 months after applying PRP (172.46 ± 59.04 hairs/cm2 before treatment to 206.06 ± 70.77 hairs/cm2 after 2 months). This increase was significant and maintained 6 months after receiving treatment (mean 205.53 ± 68.20 hairs/cm2, Friedman test, P < .0001) (Figs. 1 and 2). As side effects during each injection, minimal bleeding was observed along with pain described as tolerable by the patients; likewise, after each session, some patients reported headache which was also well tolerated and resolved rapidly, even without the need to administer acetaminophen. In our cohort, an increase in hair density by 10% to 20% was the outcome observed with greatest frequency (in 33% of patients [10/30]). In addition, in 6.7% of patients (2/30), an increase of more than 50% in hair density was observed. However, at 6 months after performing the PRP injection, a decrease was demonstrated in hair density in 13.3% of patients (4/30) (Table 1). In addition, we observed a correlation between efficacy of the application of PRP and type of AGA (Fisher exact test, P = .04). The pattern with least response was stage 3 vortex (only 37.5% of patients responded positively). However, the efficacy rate was 100% for stages 1, 3, and 4; 83.33% for stage 2; and 75% for stage 5. There was no correlation between a favorable response and patient age (Fisher exact test, P = .5) or duration of AGA (Fisher exact test, P = .7) (Table 2).
Baseline characteristics and hair density values in 30 male patients with androgenetic alopecia treated with 3 sessions of platelet rich plasma 1 month apart.
| Patient Number | Age, y | Family History | Duration of Alopecia, y | Stage of Alopecia (Norwood Scale) | [0,6–8]Hair Density (hairs/cm2) | ||
|---|---|---|---|---|---|---|---|
| Before the First Session | After 2 Months | After 6 Months | |||||
| 1 | 30 | Yes | 2 | 3 vertex | 175 | 229 | 177 |
| 2 | 29 | Yes | 7 | 3 vertex | 177 | 155 | 243 |
| 3 | 17 | Yes | 0.25 | 1 | 136 | 160 | 193 |
| 4 | 28 | Yes | 6 | 3 vertex | 202 | 210 | 225 |
| 5 | 29 | Yes | 16 | 5 | 92 | 86 | 85 |
| 6 | 23 | Yes | 2 | 2 | 200 | 270 | 270 |
| 7 | 24 | Yes | 8 | 2 | 66 | 122 | 163 |
| 8 | 33 | No | 3 | 4 | 50 | 100 | 110 |
| 9 | 21 | Yes | 2 | 3 | 228 | 271 | 282 |
| 10 | 42 | Yes | 20 | 3 | 288 | 316 | 340 |
| 11 | 42 | Yes | 5 | 3 vertex | 207 | 246 | 235 |
| 12 | 23 | Yes | 2 | 3 | 166 | 213 | 220 |
| 13 | 21 | Yes | 1.5 | 2 | 242 | 343 | 337 |
| 14 | 25 | No | 5 | 5 | 169 | 228 | 247 |
| 15 | 34 | Yes | 14 | 4 | 210 | 232 | 243 |
| 16 | 35 | Yes | 8 | 2 | 198 | 308 | 200 |
| 17 | 23 | Yes | 8 | 5 | 138 | 202 | 207 |
| 18 | 24 | Yes | 6 | 3 | 118 | 152 | 132 |
| 19 | 25 | Yes | 4 | 3 vertex | 190 | 272 | 181 |
| 20 | 24 | Yes | 1.5 | 3 vertex | 70 | 72 | 80 |
| 21 | 34 | Yes | 10 | 5 | 145 | 160 | 151 |
| 22 | 27 | Yes | 5 | 2 | 255 | 265 | 273 |
| 23 | 29 | Yes | 6.5 | 4 | 236 | 256 | 255 |
| 24 | 21 | Yes | 1 | 3 vertex | 170 | 153 | 202 |
| 25 | 26 | Yes | 3 | 3 | 245 | 280 | 290 |
| 26 | 25 | Yes | 2 | 3 | 115 | 162 | 130 |
| 27 | 21 | Yes | 2 | 3 | 225 | 245 | 248 |
| 28 | 35 | Yes | 3 | 3 vertex | 140 | 121 | 124 |
| 29 | 25 | Yes | 4 | 2 | 188 | 197 | 152 |
| 30 | 21 | Yes | 1 | 3 | 133 | 156 | 171 |
In some previous studies, PRP has been found to be a useful alternative in the treatment of AGA2–4,6; however, other studies have questioned its effectiveness.5 In the present study, we noted that PRP improved hair density by 19.17% in men with AGA at 2 months after application, and this improvement was sustained at 4 months. Our findings are consistent with those of Ho et al.7 in 2018, who used PRP injections in combination with other capillary treatments, whereas PRP was applied as monotherapy in this study. In the study by Alves and Grimalt6 in 2016, the mean increase in hair density at 6 months of treatment was 7.6%, whereas we observed an increase of 19.17%. This discrepancy could in part be attributed to the inclusion of patients of both sexes in the study by Alves and Grimalt, whereas our study was limited only to male patients. In 2016, Puig et al.8 reported no significant improvement after the use of PRP in female patients diagnosed with AGA. However, these findings do not rule out a potential positive effect in male patients. After application of PRP injections, both patients and physicians look for an increase in hair density of more than 50%. This was achieved in only 6.7% of our patients; whereas in most cases, the increase in hair density was only between 10% and 20% (33.3% of patients). As a result, we confirm that the efficacy of treatment with PRP will vary considerably among patients, and this should be born in mind in clinical practice. The variation of PRP efficacy will depend on differences in preparation and application. However, to date, there is no standard protocol for the technique.3 Finally, 13.3% of our cohort demonstrated a decrease in hair density after therapy with PRP. These findings could be explained by progression of AGA, which cannot be controlled through PRP injections alone. Furthermore, our results show that there is a correlation between efficacy of the PRP injections and AGA stage. However, a more extensive statistical analysis would be needed before confirming this correlation. To the best of our knowledge, there are no previous studies that report the correlation between response to treatment with PRP and patient age or duration of alopecia. In the present study, we observed that PRP use was effective regardless of patient age or duration of alopecia. However, we believe that there is a need to conduct a study in a larger cohort to confirm these findings. The limitations of this study are the small sample size, the short follow-up period, and the lack of data on the diameter of the hair follicle due to lack of the necessary equipment in our clinics.
ConclusionPRP injections have a favorable effect on hair density in male patients diagnosed with AGA, with minimal short-term side effects.
Conflicts of interestThe authors declare that they have no conflicts of interest.
We would like to thank Iman Shryki for language support and Dr. Haitham Yazji (Head of Analysis Department in the Tishreen University Hospital) for providing the necessary material for PRP preparation.
Please cite this article as: Khaled Yaseer S, Jamil Hassan F, Badi Suleiman H. Eficacia del tratamiento con inyecciones intradérmicas de plasma rico en plaquetas para la alopecia androgenética en varones: estudio de «antes-después». Actas Dermosifiliogr. 2020;111:574–578.