Eczema and urticaria are both inflammatory skin diseases. The prevalence of both diseases varies worldwide and the reasons are unknown. We aimed to investigate the eczema and urticaria prevalence in the Portuguese adult (≥16 years-old) population.
Materials and methodsA telephone interview survey was performed in the last quarter of 2017. To calculate the prevalences, subjects should have been previously diagnosed with eczema/urticaria by a health professional, be aged ≥16 years-old, and reside in Portugal. The sample had a proportion that was approximately representative by population, region, gender, and age group. Odds ratios were performed to measure associations with prevalences. SPSS statistics and values of p<0.05 with 95% confidence intervals were considered statistically significant.
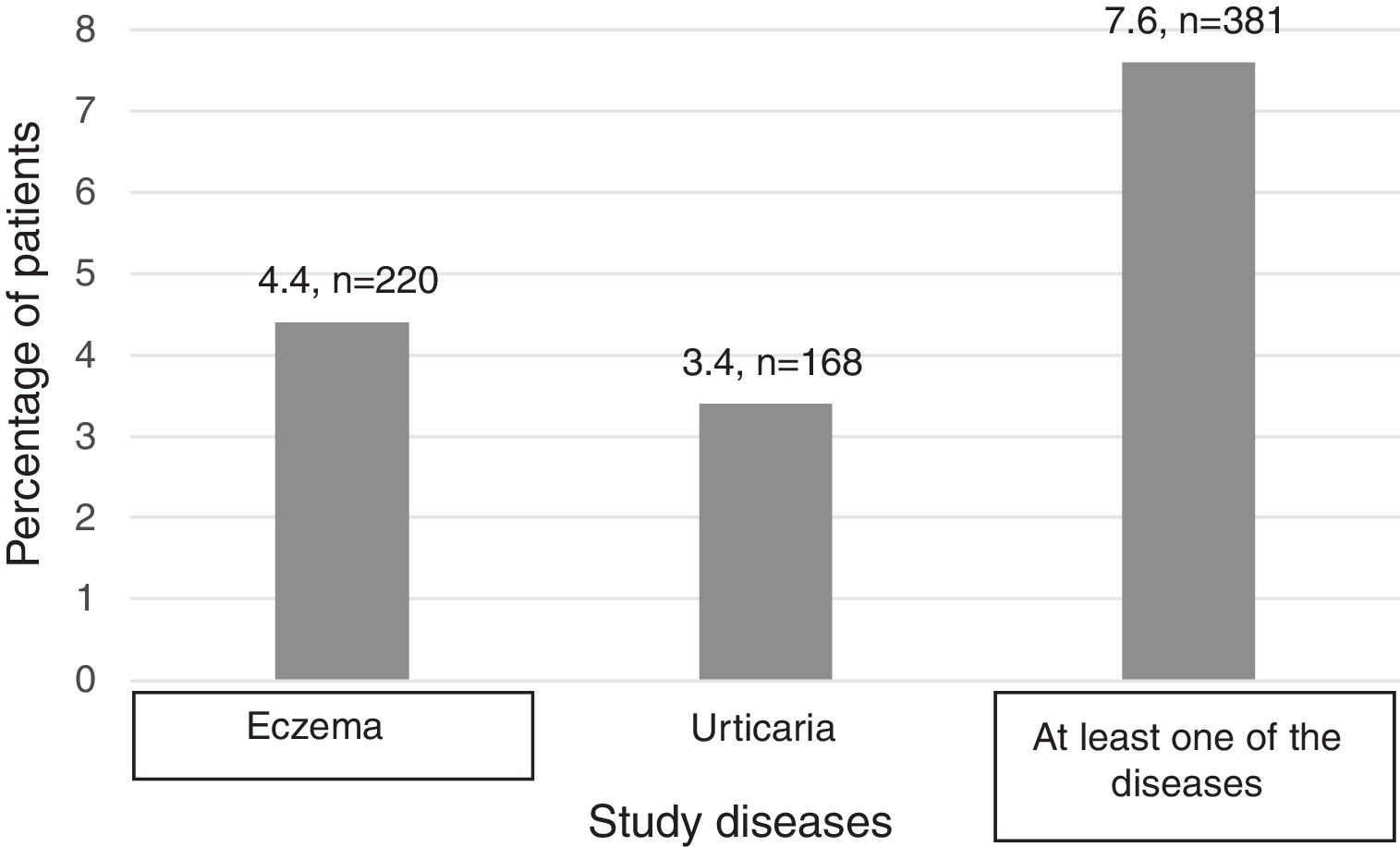
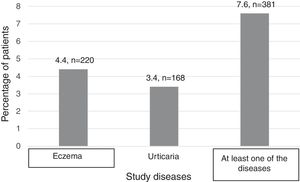
Results5,000 phone calls were analysed. The prevalence of eczema and urticaria in Portugal is 4.4% and 3.4%, respectively. Algarve is the region with the highest prevalence for both diseases. Being a female is the factor that most influenced these diseases with an OR=1.99 (p<0.001; CI 1.49-2.66) for eczema and 1.73 (p=0.001; CI 1.25 – 2.40) for urticaria, with also higher prevalences (5.7% and 4.2%, respectively).
ConclusionsThe prevalences found are higher than in previous studies in Portugal and comparable to results from other countries. Comparisons among prevalence of eczema are affected by several obstacles. Regarding urticaria, our results seem to be in the same line as others. Being female with eczema and urticaria is more common and represents a higher risk factor than male subjects. According to Harrop et al., 2007, in Europe, atopic eczema is 0.14-0.60% of general eczema. In this way, we can estimate that prevalence of atopic eczema in Portugal is around 0.61-2.64%.
Tanto el eccema como la urticaria son enfermedades inflamatorias de la piel. La prevalencia de ambas varía a lo largo de todo el mundo y se desconocen las razones de este hecho. Nuestro objetivo es investigar la prevalencia del eccema y la urticaria en la población portuguesa adulta (≥16 años).
Materiales y métodosSe realizó una encuesta telefónica en el último trimestre de 2017. Para calcular las prevalencias, los individuos debían haber sido diagnosticados previamente, por un profesional sanitario, de eccema/urticaria, ser mayores de 16 años y residir en Portugal. La muestra era aproximadamente representativa de la población, región, sexo y grupo de edad. La ratio de odds se empleó para medir las asociaciones con la prevalencia. Se utilizó el software SPSS Statistics, y aquellos datos con un valor p<0,005 con un intervalo de confianza del 95% fueron considerados estadísticamente significativos.
ResultadosSe analizaron 5.000 llamadas telefónicas. La prevalencia en Portugal del eccema y la urticaria es del 4,4% y 3,4%, respectivamente. El Algarve es la región en la que la prevalencia de ambas enfermedades es más alta. Ser mujer es el factor que más influyó en estas enfermedades, con una OR=1,99 (p<0,001; IC: 1,49-2,66) para el eccema y OR=1,73 (p=0,001; IC: 1,25-2,40) para la urticaria, siendo las prevalencias también más altas (5,7% y 4,2%, respectivamente).
ConclusionesLas prevalencias encontradas son más altas que las observadas en estudios anteriores en Portugal y comparables a los resultados procedentes de otros países. Las comparativas de la prevalencia en el eccema se ven afectadas por varios obstáculos. En cuanto a la urticaria, nuestros resultados parecen estar en consonancia con otros. Ser mujer con eccema y urticaria es más frecuente y representa un factor de riesgo más alto que el ser hombre. De acuerdo con Harrop et al., 2007, en Europa, el eccema atópico supone el 0,14-0,60% del eccema total. En este sentido, podemos estimar que la prevalencia del eccema atópico en Portugal ronda el 0,61-2,64%.
Both eczema and urticaria are common skin diseases. Eczema is an umbrella term for a group of conditions in which the skin becomes red, itchy and inflamed in a characteristic pattern.1–3 There are different types of eczema: atopic dermatitis (AD), contact dermatitis, hand dermatitis and others,1–3 which can affect different anatomical areas of the skin.
Although eczema can appear at any time during life, about 60% of AD cases, for example, are thought to be present during the first year.4 Once the illness has occurred in the paediatric age, exacerbations may disappear or continue over the years. Approximately 40-60% of adult patients already experienced the disease in the past.5,6 However, few studies describe eczema epidemiologically in adults and the differences between prevalence definitions makes the comparison of results more complex, due to the methodological heterogeneity.
The prevalence of atopic eczema varies between 15-30% in children and 2-20% in adults, globally.7–9 A single study in Portugal reports a prevalence of atopic eczema in adults aged <15 years of 1.1%.10 However, the reasons for this variability are not known.8,9
Urticaria is a heterogeneous group of diseases. Almost all types of urticaria present with a common and distinctive clinical pattern, i.e., the development of itchy evanescent wheals and/or angioedema.11 The existing epidemiological data about the prevalence of urticaria, relate mostly, to the various subtypes of individual urticaria.
It is estimated that approximately 10-20% of the world's population will experience an episode of acute urticaria or angioedema at some point in life.7,12,13 Concerning the prevalence of general urticaria, around 15% of the population is affected worldwide.14
Both for eczema and urticaria, genetics is an important determinant of prevalence variability. Nevertheless, genetics is not alone. Other factors may influence, age and gender are reported to have an important role in the disease cycle.7,9,15–17
Due to the lack of information regarding prevalence of these diseases in Portugal, this study sought to determine the prevalence in the Portuguese adult population.
Material and methodsThere is no listing or database in Portugal concerning the population studied. As so, telephone interviews were conducted in order to collect the data. The interviews were conducted in the last quarter of 2017 by a market research company: Consulmark®, certified by the International Standards Organization (ISO) 9001:2008. The interview was carried out with the person who answered the phone. This study was previously approved by the Portuguese commission of data protection (CNPD) in 2016.
All the individuals who answered and agreed to respond were included in the study. To calculate the prevalences, subjects were considered if:
They had current eczema or urticaria. In case of affirmative answer to the questions ‘Do you have atopic dermatitis or eczema or urticaria, confirmed by a doctor?’, and ‘Did you have the last symptom less than 5 years ago?’
Aged 16 years or more, having Portuguese nationality, and residing in Continental Portugal.
Individuals who, in the question “Who made the diagnosis” answered someone other than a health professional (a physician, a nurse or a pharmacist), were excluded. People with eczema included AD, contact dermatitis or hand eczema. People with urticaria included chronic or acute urticaria.
There is no data regarding the prevalence of these diseases in Portugal. For sample size purposes, we estimated a conservative average prevalence for both diseases together due to three factors: 1) because the prevalence in 6-7 and 13-14 years old is 14.1% and 12.7% respectively,18 2) the prevalence in adults is lower, and 3) the prevalence in the closest country, Spain, ranges 4-7%.6,19 The Portuguese population in the last quarter of 2017 was 10,047,621,20 and for an estimated 10% of prevalence, a margin of error less than 1% to improve precision and 95% confidence interval, a sample size of 4,267 was calculated. In this way we rounded off to 5000 phone calls.
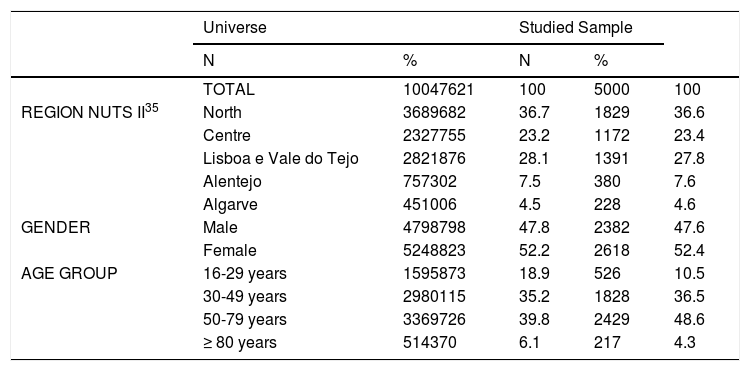
The sample had a proportion that was approximately representative by population, region, gender, and age group with proximal distribution (Table 1). Although the percentages concerning age group were not as similar as expected, they are similar in terms of means: 48.70 vs 51.57, universe vs population, respectively.
Sample representative distribution for region, gender and age.
| Universe | Studied Sample | ||||
|---|---|---|---|---|---|
| N | % | N | % | ||
| TOTAL | 10047621 | 100 | 5000 | 100 | |
| REGION NUTS II35 | North | 3689682 | 36.7 | 1829 | 36.6 |
| Centre | 2327755 | 23.2 | 1172 | 23.4 | |
| Lisboa e Vale do Tejo | 2821876 | 28.1 | 1391 | 27.8 | |
| Alentejo | 757302 | 7.5 | 380 | 7.6 | |
| Algarve | 451006 | 4.5 | 228 | 4.6 | |
| GENDER | Male | 4798798 | 47.8 | 2382 | 47.6 |
| Female | 5248823 | 52.2 | 2618 | 52.4 | |
| AGE GROUP | 16-29 years | 1595873 | 18.9 | 526 | 10.5 |
| 30-49 years | 2980115 | 35.2 | 1828 | 36.5 | |
| 50-79 years | 3369726 | 39.8 | 2429 | 48.6 | |
| ≥ 80 years | 514370 | 6.1 | 217 | 4.3 | |
Data were collected through a structured questionnaire consisting of eight questions developed specifically for the study objectives, covering topics such as gender, age, and region; number of people in household; having or not eczema or urticaria; time since diagnosis; who diagnosed; having the disease in childhood, and if another person in the family has the same disease.
Since the study was performed for two different diseases, the analyses were performed individually (having eczema or urticaria) and having at least one of these diseases. For prevalence purposes, the numbers of subjects with each disease were divided by the population who was interviewed by telephone.
The descriptive analyses were performed for qualitative variables (frequencies and percentages, with 95% of confidence interval) and quantitative variables (mean, median, standard deviation [SD], minimum, and maximum). The associations between prevalence and different regions, gender, and age group were made by chi-square test.
Odds Ratios with 95% CI were performed to measure associations with prevalences. Also, a multivariate analysis was executed with the following variables: disease (as dependent), age, region, and gender, with a 95% CI.
To infer about prevalence consistency, a secondary prevalence was computed by the sum of individuals in the households with disease divided by the sum of all households’ individuals. Therefore, the prevalence based on the number of individuals who answered the phone is designated “main primary prevalence”. The one that was calculated with households, is designated “secondary prevalence”.
Statistical tests were 2-tailed considering a significance level of 5%. Statistical analysis was conducted through the software IBM® SPSS® Statistics 22.
ResultsSociodemographic characteristicsTo reach the number of intended phone responses, 13,065 telephone calls were made, of which 7,238 (55.4%) were refusals to participate, and 819 (6.3%) included situations that did not advance to the questionnaire. Of these calls, 5,009 were completed and validated.
Nine subjects with eczema and urticaria (0.18%) were excluded due to their responses to the question “who made the diagnosis”. In this way, 5,000 individuals were analysed and distributed as shown in Figure 1.
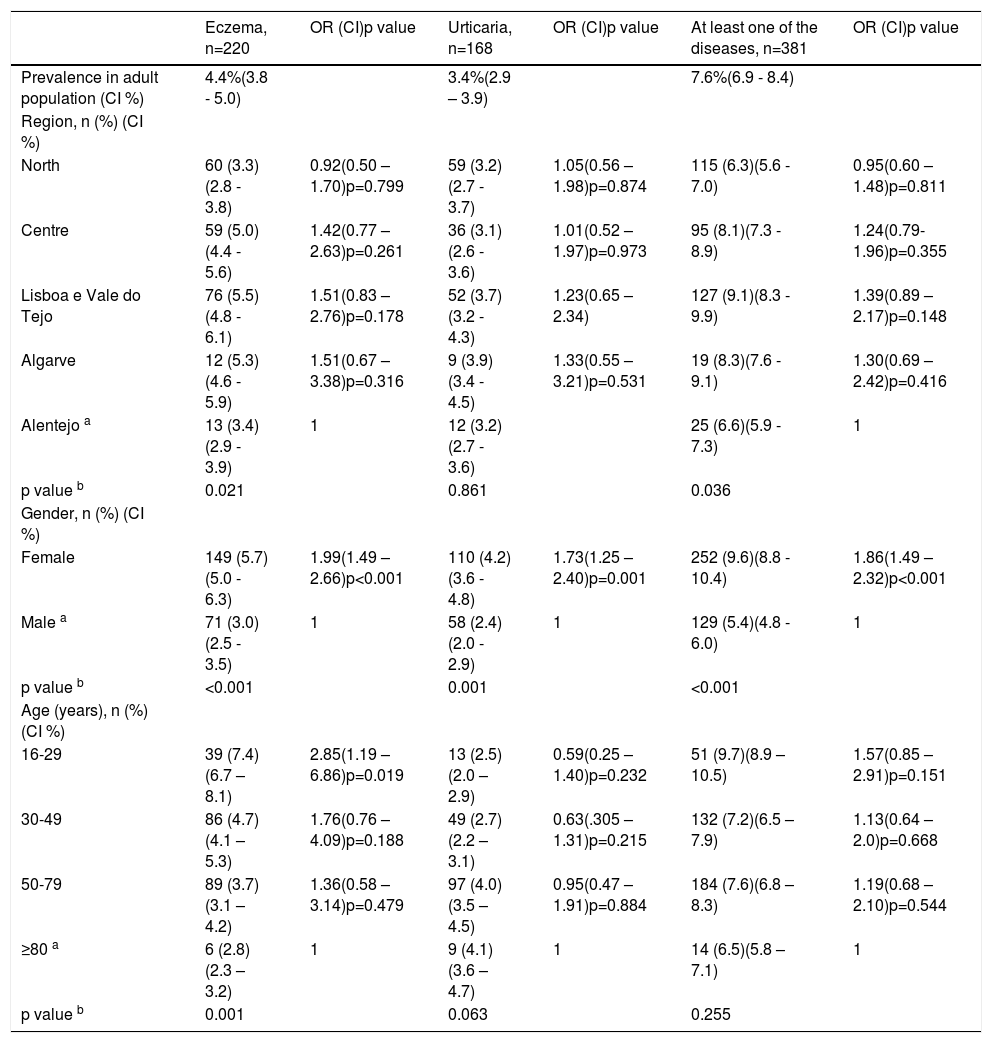
As described in the methods section, it is possible to verify that the main prevalence of eczema in Portugal is 4.4% and the main prevalence of urticaria is 3.4%. 7.6% of Portuguese population have at least one of these diseases (Table 2). Seven patients were found to have both diseases.
Main prevalence of eczema and urticaria and respective risk factors: region, gender and age.
| Eczema, n=220 | OR (CI)p value | Urticaria, n=168 | OR (CI)p value | At least one of the diseases, n=381 | OR (CI)p value | |
|---|---|---|---|---|---|---|
| Prevalence in adult population (CI %) | 4.4%(3.8 - 5.0) | 3.4%(2.9 – 3.9) | 7.6%(6.9 - 8.4) | |||
| Region, n (%) (CI %) | ||||||
| North | 60 (3.3)(2.8 - 3.8) | 0.92(0.50 – 1.70)p=0.799 | 59 (3.2)(2.7 - 3.7) | 1.05(0.56 – 1.98)p=0.874 | 115 (6.3)(5.6 - 7.0) | 0.95(0.60 – 1.48)p=0.811 |
| Centre | 59 (5.0)(4.4 - 5.6) | 1.42(0.77 – 2.63)p=0.261 | 36 (3.1)(2.6 - 3.6) | 1.01(0.52 – 1.97)p=0.973 | 95 (8.1)(7.3 - 8.9) | 1.24(0.79- 1.96)p=0.355 |
| Lisboa e Vale do Tejo | 76 (5.5)(4.8 - 6.1) | 1.51(0.83 – 2.76)p=0.178 | 52 (3.7)(3.2 - 4.3) | 1.23(0.65 – 2.34) | 127 (9.1)(8.3 - 9.9) | 1.39(0.89 – 2.17)p=0.148 |
| Algarve | 12 (5.3)(4.6 - 5.9) | 1.51(0.67 – 3.38)p=0.316 | 9 (3.9)(3.4 - 4.5) | 1.33(0.55 – 3.21)p=0.531 | 19 (8.3)(7.6 - 9.1) | 1.30(0.69 – 2.42)p=0.416 |
| Alentejo a | 13 (3.4)(2.9 - 3.9) | 1 | 12 (3.2)(2.7 - 3.6) | 25 (6.6)(5.9 - 7.3) | 1 | |
| p value b | 0.021 | 0.861 | 0.036 | |||
| Gender, n (%) (CI %) | ||||||
| Female | 149 (5.7)(5.0 - 6.3) | 1.99(1.49 – 2.66)p<0.001 | 110 (4.2)(3.6 - 4.8) | 1.73(1.25 – 2.40)p=0.001 | 252 (9.6)(8.8 - 10.4) | 1.86(1.49 – 2.32)p<0.001 |
| Male a | 71 (3.0)(2.5 - 3.5) | 1 | 58 (2.4)(2.0 - 2.9) | 1 | 129 (5.4)(4.8 - 6.0) | 1 |
| p value b | <0.001 | 0.001 | <0.001 | |||
| Age (years), n (%) (CI %) | ||||||
| 16-29 | 39 (7.4)(6.7 – 8.1) | 2.85(1.19 – 6.86)p=0.019 | 13 (2.5)(2.0 – 2.9) | 0.59(0.25 – 1.40)p=0.232 | 51 (9.7)(8.9 – 10.5) | 1.57(0.85 – 2.91)p=0.151 |
| 30-49 | 86 (4.7)(4.1 – 5.3) | 1.76(0.76 – 4.09)p=0.188 | 49 (2.7)(2.2 – 3.1) | 0.63(.305 – 1.31)p=0.215 | 132 (7.2)(6.5 – 7.9) | 1.13(0.64 – 2.0)p=0.668 |
| 50-79 | 89 (3.7)(3.1 – 4.2) | 1.36(0.58 – 3.14)p=0.479 | 97 (4.0)(3.5 – 4.5) | 0.95(0.47 – 1.91)p=0.884 | 184 (7.6)(6.8 – 8.3) | 1.19(0.68 – 2.10)p=0.544 |
| ≥80 a | 6 (2.8)(2.3 – 3.2) | 1 | 9 (4.1)(3.6 – 4.7) | 1 | 14 (6.5)(5.8 – 7.1) | 1 |
| p value b | 0.001 | 0.063 | 0.255 |
For both diseases, the region with the highest prevalence is the Algarve (5.3% for eczema and 3.9% for urticaria). Another point that can be highlighted is the homogeneity of prevalence in all regions for urticaria (except for the Algarve), which is not the case for eczema, which presents different percentages for each region.
Gender revealed to be the factor that most affects the occurrence of both eczema and urticaria. A higher prevalence among females is observed for both diseases (5.7% for eczema and 4.2% for urticaria). Being female was also a statistically significant risk factor for these diseases independent of patients’ age and place residence (univariate analysis: OR=1.96 [p<0.001; CI 1.47 – 2.62] and multivariate analysis: OR=1.99 [p<0.001; CI 1.49 – 2.66] for eczema and urticaria's univariate analysis: 1.76 [p=0.001; CI 1.27 – 2.43] and multivariate analysis: 1.73 [p=0.001; CI 1.25 – 2.40] (Table 2). Concerning age, only the group 16-29 years old showed a statistically significant risk factor for eczema, OR=2.85 (p=0.019; CI [1.19 – 6.86]).
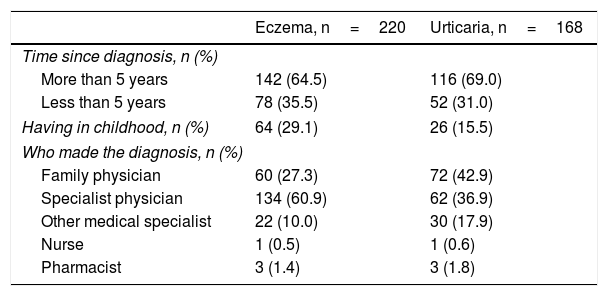
Regarding other questions asked, for the eczema subgroup it was possible to observe that 142 (64.5%) had the disease (or the disease was diagnosed) for more than five years. Of these patients, at the moment of the interview all had some symptoms or signs of the disease. However, only 64 (29.1%) individuals had the disease in childhood (Table 3). In the same table are presented the results related to the subgroup of urticaria. The majority of patients admitted having the diagnosis for more than five years (116; 69%), 26 of which admitted suffering from the disease during childhood.
Clinical characteristics.
| Eczema, n=220 | Urticaria, n=168 | |
|---|---|---|
| Time since diagnosis, n (%) | ||
| More than 5 years | 142 (64.5) | 116 (69.0) |
| Less than 5 years | 78 (35.5) | 52 (31.0) |
| Having in childhood, n (%) | 64 (29.1) | 26 (15.5) |
| Who made the diagnosis, n (%) | ||
| Family physician | 60 (27.3) | 72 (42.9) |
| Specialist physician | 134 (60.9) | 62 (36.9) |
| Other medical specialist | 22 (10.0) | 30 (17.9) |
| Nurse | 1 (0.5) | 1 (0.6) |
| Pharmacist | 3 (1.4) | 3 (1.8) |
The question if there were someone in the family with eczema or urticaria was also asked to individuals who did not have the disease, i.e. it was included in the 5,000 participants in the phone calls. In this way, it was possible to construct more subgroups for analysis: having eczema, urticaria or at least one of the diseases, from households’ population. Of the 220 individuals with eczema, 40 (18.2%) reported having someone in the family with the disease as well. Of the 168 individuals with urticaria, 22 (13.1%) reported having someone in the family with the disease.
In a population with an average 1.8 (min: 0 – max: 11) of households, there are 0-3 people in the family with eczema and/or urticaria. In total, among all households in the sample of this study, 467 subjects showed having eczema, and 146 presented urticaria.
As explained in the methods, secondary prevalence was calculated for this new population, revealing a prevalence of 5.2% for eczema and 2.8% for urticaria. It is also possible to observe that 7.9% of this population had at least one of the diseases.
DiscussionThe population studied is not part of a set of observation units for which there is a listing or a data base in Portugal. Thus, to investigate the prevalence, the data collection was by telephone interviews. There are several studies in which the same methodology was used, namely a Portuguese study of the National Health Observatory in 2004, which objective was to evaluate the self-reported prevalence of certain chronic diseases, as psoriasis.21 As early as 1994, the use of telephone sampling was advocated for epidemiology and health-related research, usually based on random number generation.22 Prevalence studies for different diseases used a similar methodology,23–25 as well as in dermatology.19,26–28
Eczema represents a group of diseases with similar clinical characteristics, and there is not a clinical standard for the definition of the disease.28,29 In this study, our approach captured different subsets of the eczema and our definition of eczema, which was based on self-reported doctor diagnosed ‘eczema or atopic dermatitis’, might have resulted in an overestimation of the prevalence, not being possible to be exact of the AD prevalence. In this way, we are aware that is might be a limitation. The diagnosis of eczema and urticaria, when made by a non-dermatologist or a non-allergist physician is of doubtful reliability, although all patients confirmed having had a second medical opinion, we consider this as a limitation of the study.
The main prevalence in adult population of both diseases was found to be 4.4% of eczema and 3.4% of urticaria. With the secondary prevalences calculations we observed again that eczema was more prevalent than urticaria with similar prevalences in having at least one of the diseases (7.6%-7.9%). These are higher than findings in previous studies in Portugal and comparable to results from other countries. But comparisons among prevalence of eczema are affected by several drawbacks. Most studies presenting data of eczema prevalence have been focused on either several atopic diseases or the whole spectrum of skin diseases. Considerably fewer studies, especially among adults, have been focused on eczema. The questions about eczema have varied considerably from self-reports of itchy rash and ever having had eczema to point prevalence of physician examinations of the skin; the latter results in several-fold lower estimates of prevalence.30 As an example, Portugal has one study reporting eczema prevalence as 1.1%, although well designed and a representative sample, the number of interviews was less and it sought to investigate other allergic diseases prevalence.10 Comparing to the closest country, Spain, when we talk about the all eczema, the prevalence seemed to be similar to ours, 4.2%.6 In ascending order, we can find the following prevalences of eczema, Germany with 5,1%, Belgium with 5.9% and France with 8%,6 while AD prevalences seem to be 1.4%, 2%, 2.4% and 3.5%, respectively.6,19 There is evidence that in Switzerland adult prevalence of eczema is lower, 2.2%.6 Italy presents a 6.6-8.1% of eczema prevalence.6,28
According to Harrop et al., 2007, in Europe, atopic eczema is 0.14-0.60% of general eczema.6 In this way, we can estimate that prevalence of EA, in Portugal is around 0.61-2.64%.
Regarding urticaria, to our knowledge, there are very few studies with evidence of general urticaria prevalence. Germany has a prevalence of 8.8% and Norway 9% for urticaria throughout life, most of which is acute or physical.31 In Poland, an occurrence of 11.2% of urticaria was reported in the population over 15 years of age.14
The region where patients live represents a risk factor for several allergic diseases,15 and so the main prevalence was also evaluated by region, we found the Portuguese areas with more prevalence of eczema to be Lisbon e Vale do Tejo (5.5%) and Algarve (5.3%). Lisbon has a few characteristics known to possibly exacerbate eczema: it is the capital, it is very polluted, and has a lot of traffic. To further understand the difference observed in Algarve, more studies should be performed. Nevertheless, a study in Italy showed that the prevalence of eczema and AD was higher in Mediterranean area than in sub-continental, 8.5 vs 7.4 and 3.8 vs 2.8, respectively.28 On the other hand, prevalence of urticaria seems to be similar across the country.
As uniformly reported in the literature, eczema is more common amongst female than male subjects.6,9,17,32 We showed a female prevalence of 5.7% against 3.0% in the male population with eczema. Also, being a woman is a significant risk factor for eczema (OR 1.99), similar to OR reported in other studies 1.84,30 2.44,17 or 1.33.6 As for eczema, urticaria shows a higher prevalence in females.16,31,33,34 We observed a female prevalence of 4.2% vs 2.4% (in male). Being a woman is also a significant risk factor for urticaria (OR 1.73), similar to other studies (OR 1.46).14
We found that more than half of respondents (64.5% with eczema and 69% with urticaria) have had the disease for more than five years. Among those with eczema, we found that 64 patients (29.1%) had the disease during childhood, while in a self-reported study, 13.7% declare having had eczema in childhood.32 Among those with urticaria, 26 patients (15.5%) had the disease during childhood.
We calculated OR and adjusted OR for the variables age, gender, and region, finding similar results. From this we conclude that these variables can influence both diseases individually and that they do not interact with each other.
Family history is an important factor in these diseases,6 and we observed that of the 220 individuals with eczema, 40 (18.2%) reported having someone in their household with the disease as well. Of the 168 individuals with urticaria, 22 (13.1%) reported having someone in their home with the disease. A limitation of our study is the fact we did not collect data on variables such as race or job, which could help us to understand better the influence of family history.
With households’ results, we were able to calculate a secondary prevalence. However, in contrast to the main prevalence of the study, this step was calculated with adult and child populations. This is due to the way the data were collected. Additionally and also in contrast to the main prevalence of the study, the sample of secondary prevalence was not proportionally representative. Thus, a direct comparison is not possible. Nevertheless, the difference between them is not so great.
ConclusionsThis study contributes with new data for the areas of Dermatology and Immunology in Portugal.
The prevalences found are higher than in previous studies in Portugal and comparable to results from other countries. Comparisons among prevalence of eczema are affected by several obstacles. Regarding urticaria, our results seem to be in the same line as others. Although there is only a few studies about prevalence of general urticaria. Being female with eczema and urticaria is more common and represents a higher risk factor than male subjects.
Financial disclosuresThis study was funding by LEOPharma.
The authors would like to thank LEOPharma for funding the project, and also to thank Consulmark® for the support and effort during the project. Finally, to John Stewart Huffstot, a director of English-language, who reviewed the language of the article.