Ectropion, or eyelid eversion, is the most common form of eyelid malposition. By impairing the eyelid’s protective function, ectropion can cause epiphora, lagophthalmos, keratinization, chronic irritation, pain, and ulceration. There are 5 types of ectropion, each with a different cause: congenital, paralytic, involutional, cicatricial, and mechanical. The most common presentation in dermatology is involutional eversion with a mechanical or tractional element. Several options exist for the surgical repair of ectropion and choice of technique will depend on the main pathogenic component. We review the basic anatomy of the eyelid and describe examination techniques for assessing risk and preventing ectropion and for identifying the main pathogenic component in order to select the most suitable repair technique.
El ectropion o eversión del párpado, es la malposición palpebral más frecuente. Al alterar la función protectora palpebral puede causar epífora, lagoftalmos, queratinización, irritación crónica, dolor o ulceración. Se distinguen 5 tipos de ectropion en función de su mecanismo causal: congénito, paralítico, involutivo, cicatricial y mecánico. Lo más habitual en dermatología, es la presencia de ectropión de tipo mixto, con elementos involutivos y mecánico-traccionales. Existen varias técnicas reparadoras de ectropion cuya indicación dependerá del componente patogénico principal. Revisamos la anatomía básica palpebral y exponemos la técnica exploratoria que nos permitirá analizar el riesgo de ectropion para prevenir su aparición o determinar la patogenia del ectropión ya establecido para definir la técnica reparadora más apropiada.
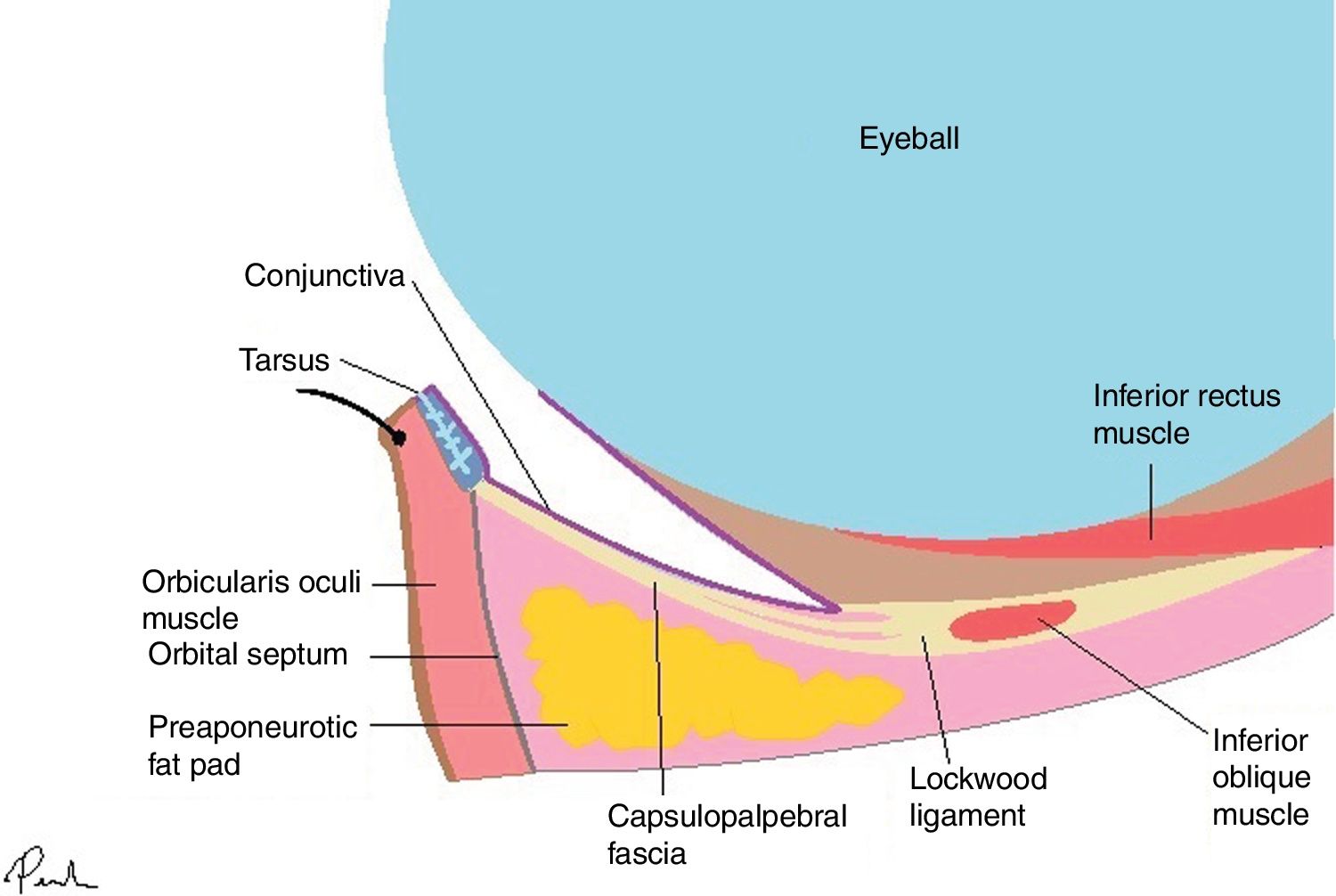
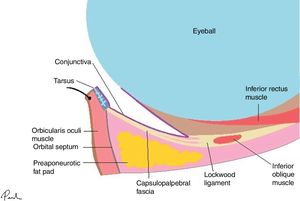
The lower eyelid is subdivided into the anterior lamella (skin and orbicularis oculi muscle), medial lamella (orbital septum, orbital fat), and the posterior lamella (capsulopalpebral fascia, tarsus, and conjunctiva)1 (Fig. 1). In its physiological position, it has a protective function and participates in tear film homeostasis.1–3 The free border of the lower eyelid should be level with the corneal limbus. The eyelid is kept in this position by the following supporting structures: medial and lateral canthal tendons, the elements comprising the medial lamella, and the posterior lamellar retractors (capsulopalpebral fascia, Lockwood ligament).1,2
Ectropion occurs on eversion of the eyelid, such that the internal surface is exposed, potentially giving rise to epiphora, lagophthalmos, chronic irritation, keratitis, pain, and ulceration. Ectropion is the most frequent eyelid malposition.4,5
There are 5 types of ectropion: congenital, paralytic, involutional, cicatricial, and mechanical. Congenital ectropion is extremely rare and usually occurs due to vertical skin foreshortening in blepharophimosis syndrome.1,2,6 Paralytic ectropion is caused by paresis of the orbicularis oculi muscle, generally as a result of facial nerve paralysis.5,6 Involutional or senile ectropion is the most frequent type,4,5 and is caused by laxity, atrophy, or disinsertion of the supporting structures (tarsus, orbital septum, ligaments, canthal tendons, and retractors), and loss of elasticity and decreased orbital and malar fat.5,6 Cicatricial and mechanical ectropion are due to a vertical vector that exerts a tractional force on the eyelid.2 In cicatricial ectropion, the most frequent cause is foreshortening of the anterior lamella due to mechanical, chemical, or thermal damage or postoperative cicatricial retractions. The most common causes of mechanical ectropion include periorbital edema and tumors.5
Periorbital tumors, in addition to causing mechanical ectropion, may indirectly give rise to cicatricial ectropion through reconstruction with excessive vertical tightening after excision.
Examination TechniquesAppropriate eyelid examination should be conducted prior to all types of periocular surgery. This will determine the risk of postoperative ectropion and enable compensatory elements to be included when planning the operation. When ectropion is already present, examination will serve to determine the predominant pathogenic component and enable the most appropriate repair technique to be chosen.
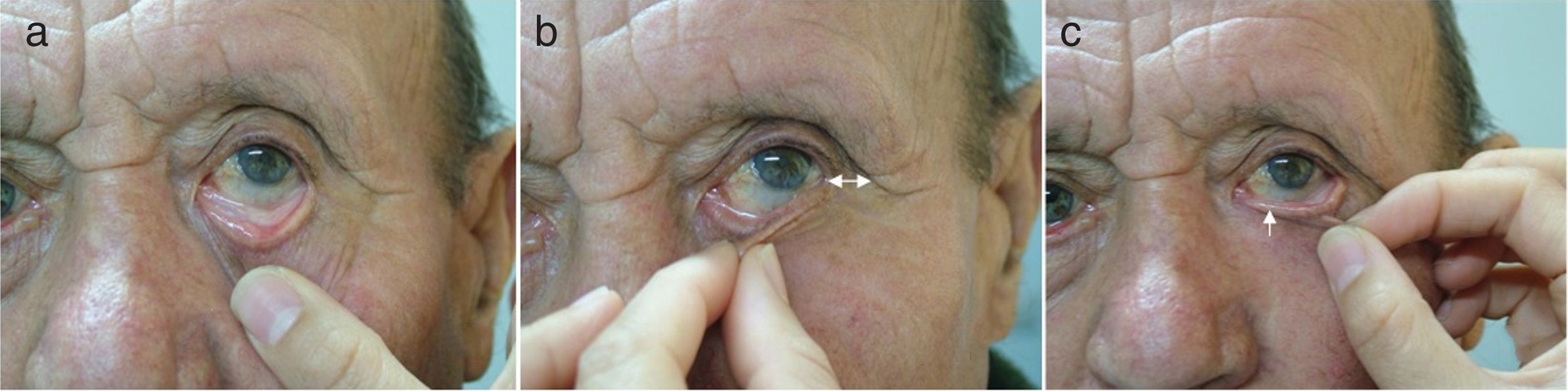
There are 4 simple tests to determine eyelid laxity, the snap back test and the vertical, lateral, and medial distraction tests (Fig. 1).7 Pulling the lower eyelid can evidence excessive laxity if there is a delay in the eyelid returning to its original position (snap back test) or if the eyelid separates more than 8 mm from the eyeball (vertical distraction test)8,9 (Fig. 2a). Medial distraction would reveal lateral canthal hyperlaxity in the event that the outer corner of the eye extends more than 2 mm (Fig. 2b) and, finally, lateral distraction would show hyperlaxity of the medial canthus if the lacrimal punctum is pulled than 2 mm8,9 (Fig. 2c).
Examination techniques. A, Snap back test and vertical distraction test: excessive laxity is observed if there is a delay in the eyelid returning to its original position or if the eyelid separates more than 8 mm from the eyeball with vertical pulling, respectively. B, Medial distraction test: lateral canthal hyperlaxity if the outer corner of the eye can be pulled more than 2 mm. C, Lateral distraction test: hyperlaxity of the medial canthus if the lacrimal punctum moves more than 2 mm. Source: Fernández-Canga et al.7
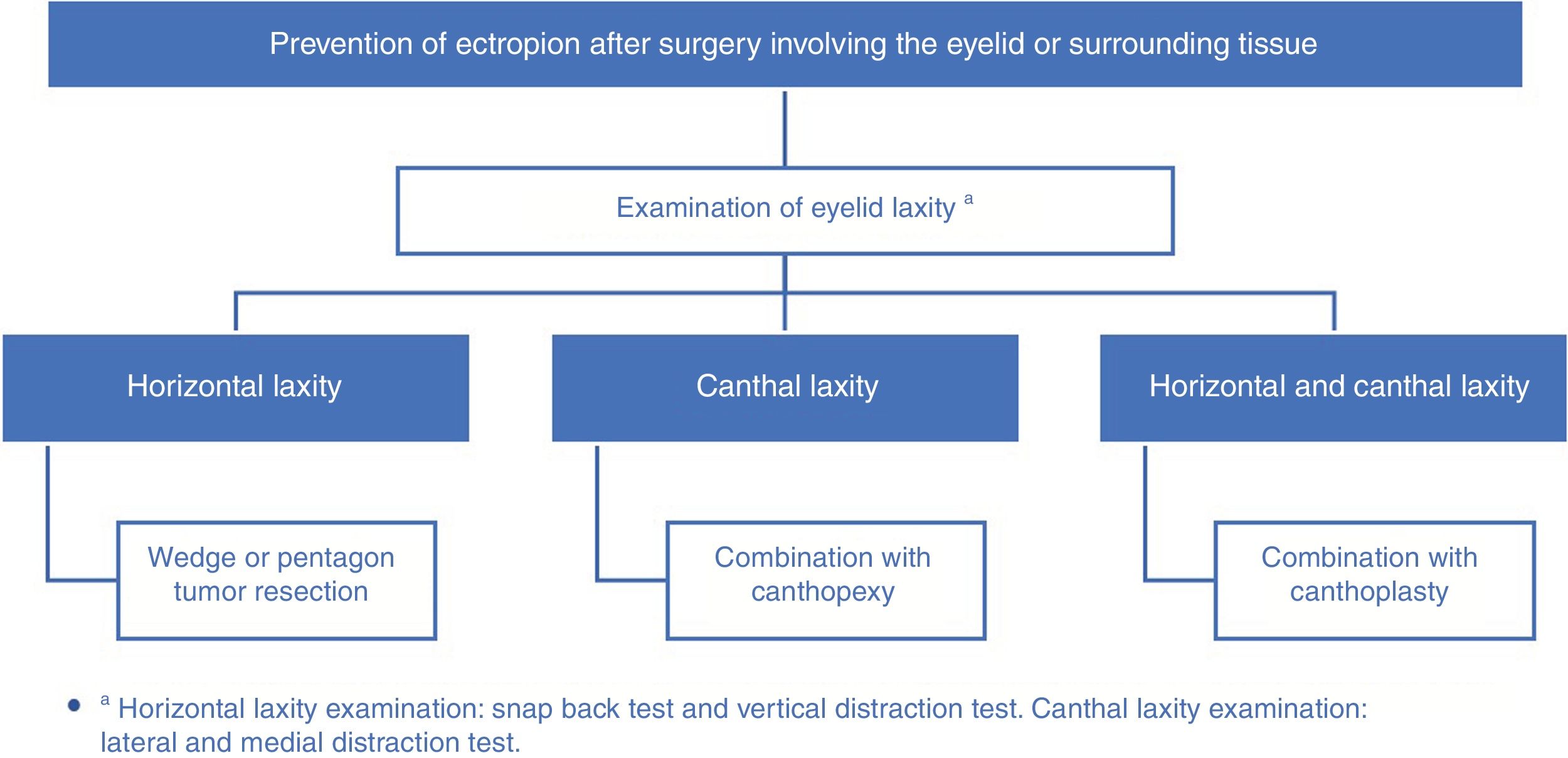
The predominant elements in the above tests would allow the most appropriate preventive or corrective surgical technique to be chosen.
Surgical Techniques to Prevent EctropionExcessive eyelid laxity is common in elderly individuals, with tumors being the most common underlying cause. Thus, when planning surgery for a tumor in the lower eyelid in patients with excessive eyelid laxity, reduction of the horizontal component or inclusion of corrective techniques should be contemplated, ideally at the same time as surgery, in order to prevent the onset of postoperative ectropion.
The Frost suspension suture, described in 1934,10 aims to bring the lower eyelid to its anatomical position in the immediate postoperative period. The technique consists of anchoring the inferior tarsus temporarily with a nonabsorbable suture that is fixed to the supraciliary space by simply stitches or with adhesive strips (enabling retightening during the healing process). This technique can prevent the formation of postoperative ectropion due to edema formation or hemorrhage in the immediate postoperative period. If the suture is centrally positioned, the eye should be kept occluded due to the risk of corneal abrasion and there is a risk of skin erosion with excessive tightening.11
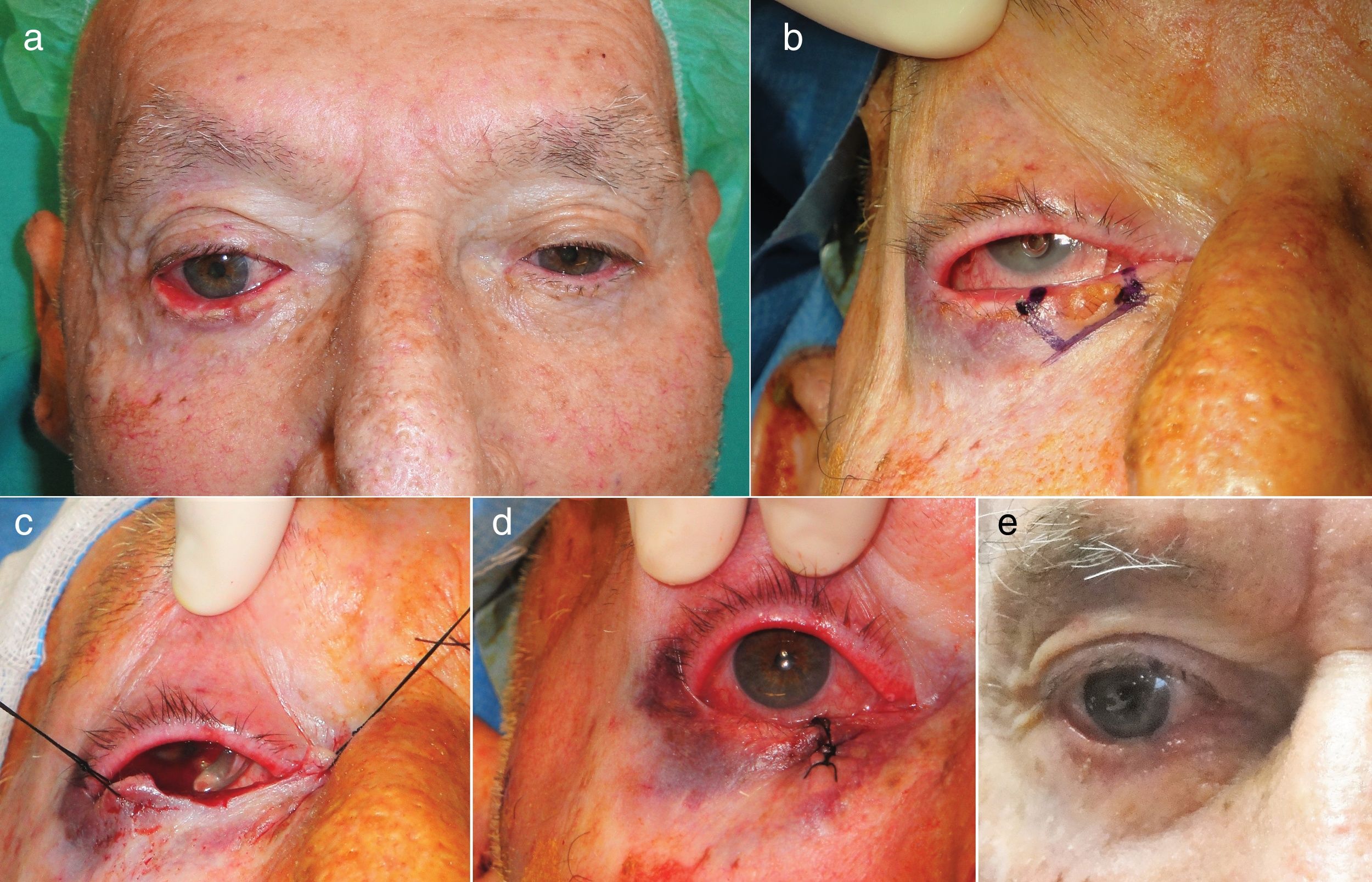
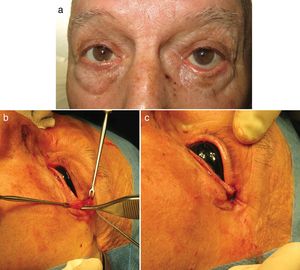
A tumor excision pattern in wedge or pentagonal form12 can shorten the lower eyelid at the same time as the tumor is removed, thereby achieving both the oncological and reconstructive goal, and avoiding ectropion (Fig. 3).
Pentagonal excision. A, Basal cell carcinoma in the lower right eyelid in an 85-year-old male patient with mixed ectropion (involutional and mechanical caused by the tumor). B and C, Pentagonal tumor resection was designed to achieve the oncological objective as well as the reconstructive one, by avoiding ectropion with a reduction in the horizontal component of the eyelid. Outcome of the technique immediately after the procedure (D) and at 8 weeks (E).
Repositioning of the central canthus is a key compensatory element that should be associated with any reconstructive procedure in the lower eyelid to help prevent ectropion formation. Two surgical techniques that can prevent or correct eyelid eversion by canthal repositioning are canthopexy and canthoplasty.13
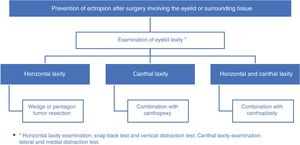
Fig. 4 shows the techniques that aim to prevent the formation of ectropion by cause.
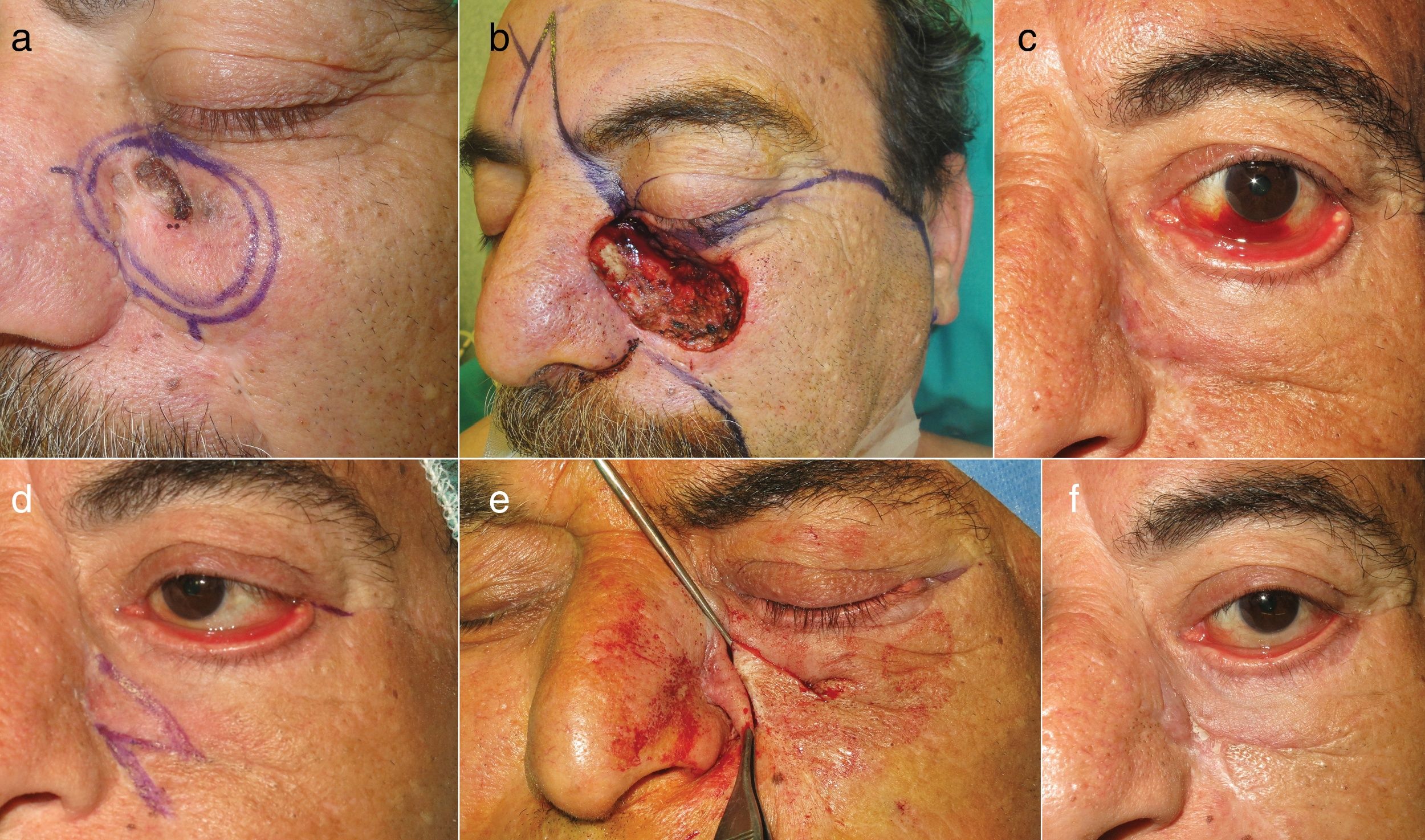
Surgical Techniques for Ectropion CorrectionThe aim of repair of cicatricial or mechanical ectropion is to eliminate cause of the tractional element. This is achieved using a Z-plasty or excising the lesion that is responsible for the vertical tensile force on the lower eyelid (Fig. 5).14
Z-plasty. A, 54-year-old patient with spindle-cell carcinoma in the infraorbital region. B, Surgical defect and reconstruction design with a glabellar and cheek combined flap. C, Multicomponent, severe postoperative ectropion, with cicatricial elements, loss of volume and involution. Symptoms of lagophthalmos and accompanying conjunctival hemorrhage. D and E, For correction, the vertical cicatricial tensile force was released by Z-plasty. F, Late postoperative outcome (at 8 weeks): repositioning of the lower eyelid.
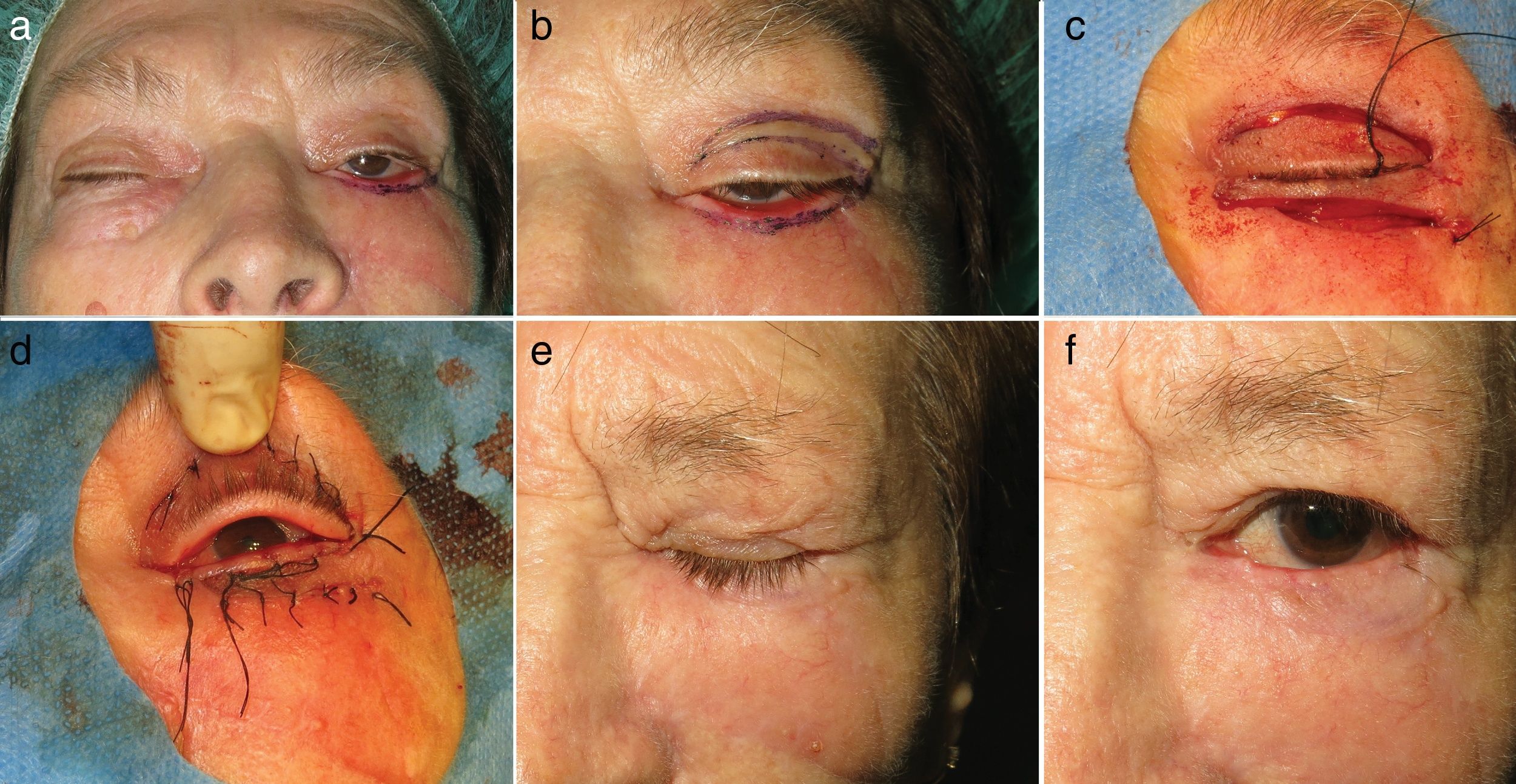
Ectropion resulting from loss of volume can be corrected by providing tissue in the form of a flap or graft, or with synthetic materials.4,9,14 One of the most widely used flaps is the Tripier flap, in which skin and muscle are taken from the upper eyelid (Fig. 6).15,16 In the case of grafting, the most appropriate areas for donor skin are the upper eyelid and the preauricular and retroauricular region, as the skin in those regions has a similar thickness and texture.3,6,17,18 Finally, synthetic materials are a valid alternative to autologous grafts, although they are less widely used given their high cost and greater risk of contraction.3
Tripier flap. A, Tractional postoperative ectropion with lack of volume in the lower eyelid. B, Design of a transposition flap from the upper eyelid or Tripier flap. C, Final positioning of the flap after making an incision immediately below the eyelash line in the lower eyelid, dissection and transposition of the flap. D, Immediate postoperative outcome. E and F, Late postoperative outcome at 8 weeks.
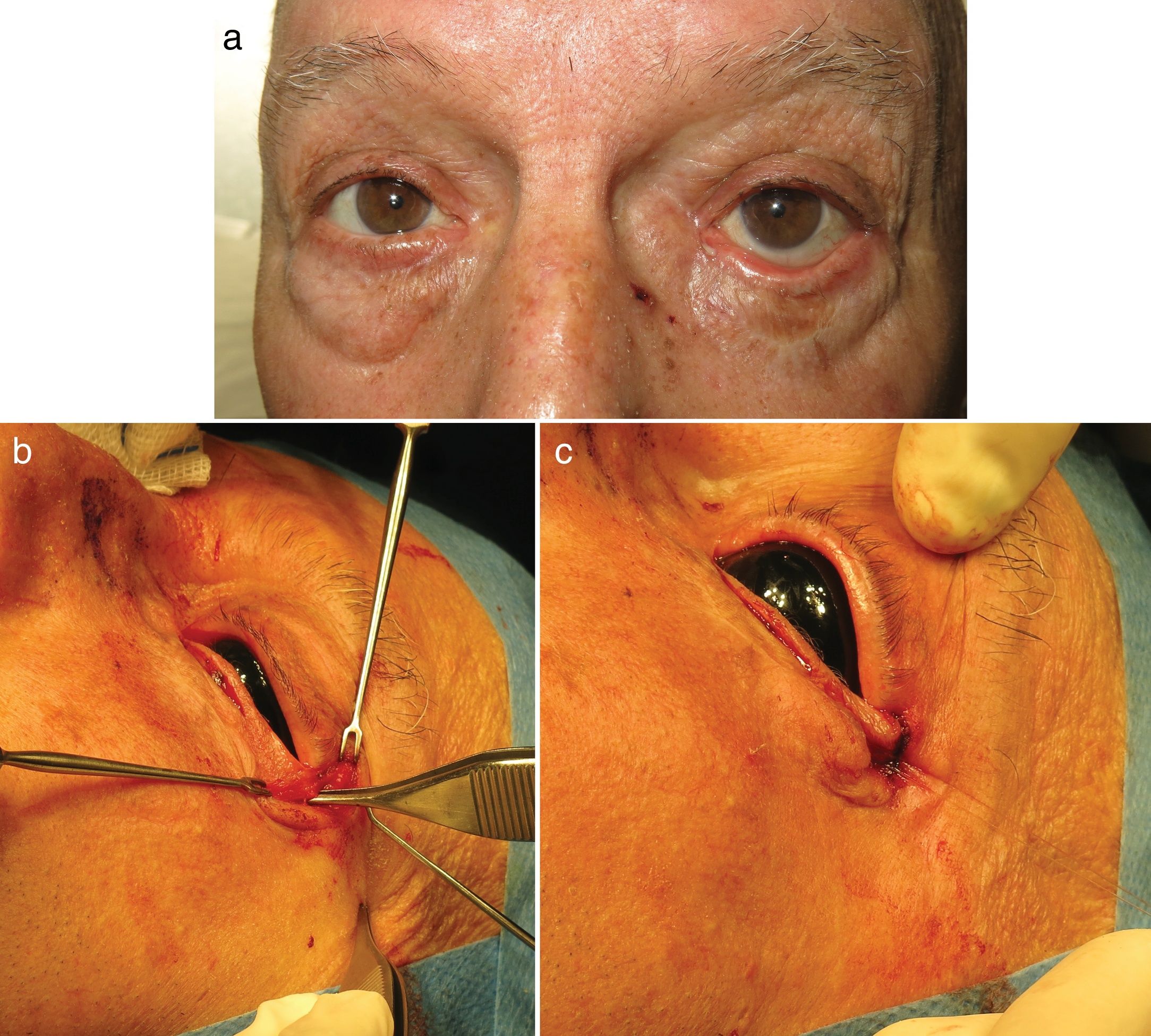
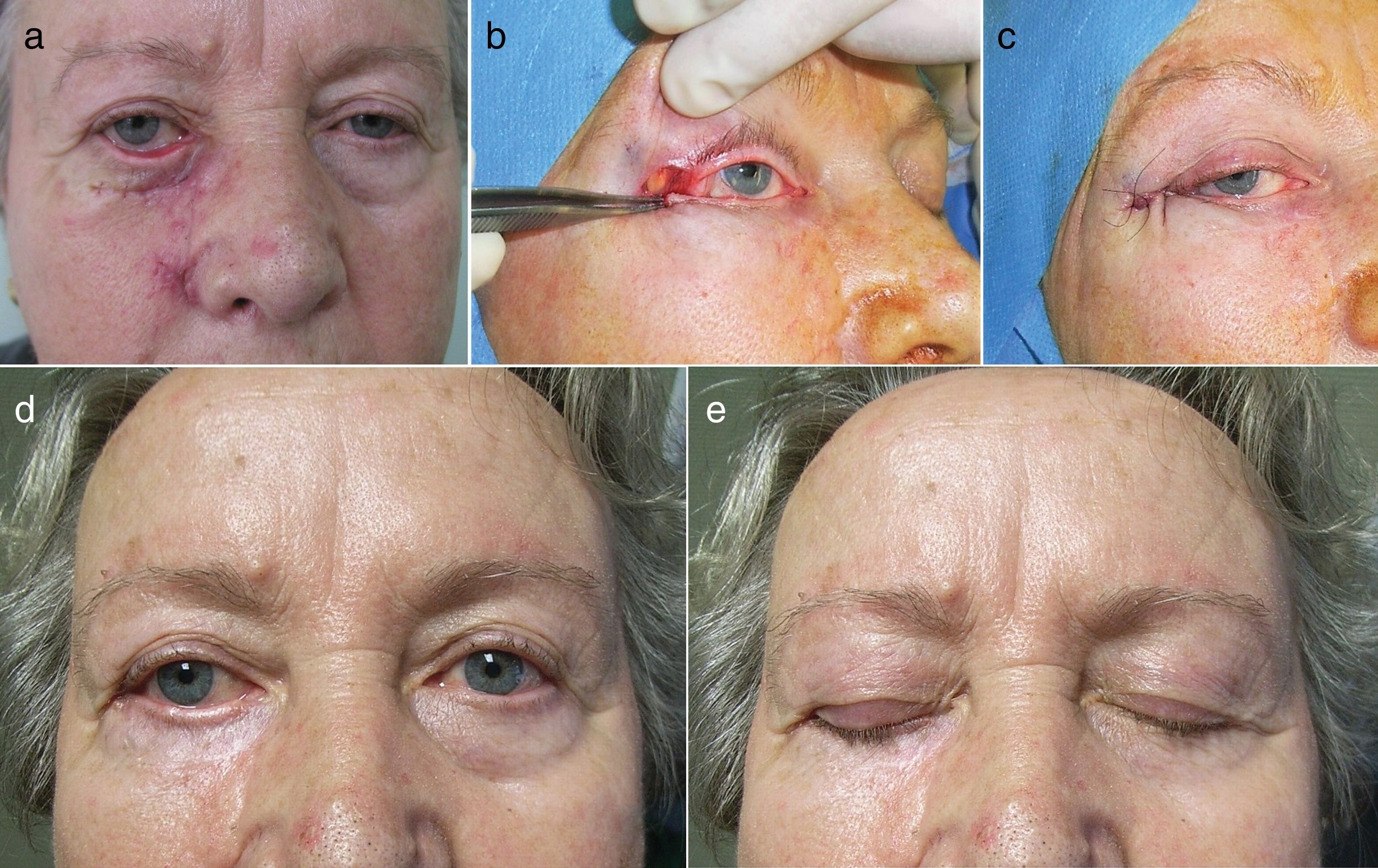
Treatment of postoperative ectropion in patients with eyelid laxity (involutional component) aims to achieve horizontal tightening. This is achieved by repositioning of the lateral canthus by canthopexy or cantoplasty.13 Canthopexy aims to tighten the lateral canthal tendon by attaching it to the lateral orbital rim without the need for canthotomy (incision and extension of the medial canthus) (Fig. 7). This is used in cases of mild hyperlaxity.13 In contrast, canthoplasty is used to correct more severe hyperlaxities and requires canthotomy before anchoring the outer canthus (Fig. 8).1,4,6,12 One of the most widely used canthoplasty procedures is the tarsal strip in which the free border of the inferior tarsus is released and deepithelialized to form a strip that is subsequently anchored to the orbital rim to form a neocanthus. The anchor point for the canthal repositioning is level with the periosteum, in the internal face of the lateral orbital rim, 2 mm above the medial canthus, so that the tears follow a superolateral or inferomedial pathway and can provide appropriate lubrication.9
Canthopexy. A, Mixed post-surgical ectropion (involutional and mechanical origin resulting from removal of a graft used for reconstruction after excision of basal cell carcinoma). B, Release of retractile tissue and an incision of 1 cm at 0.3 to 0.5 cm from the outer canthus and dissection until locating the external canthal ligament. C, Fixing the canthal ligament to the internal face of the periosteum of the orbital rim with a single-strand absorbable 5/0 suture.
Canthoplasty. A, Postsurgical eversion of the lower eyelid in a 65-year-old woman with moderate-severe horizontal laxity. B, Lateral canthoplasty for eyelid repositioning: horizontal incision of 1 cm in the anterior lamella through the external canthus, leaving the canthal ligament exposed. Location of the anchoring point that corrects the defect and attachment of the ligament to the periosteum of the internal face of the orbital rim with an absorbable 5/0 suture, at 2 mm above the internal canthus. C, Skin suture by direct closure with 5/0 silk (Fig. 7B and C). D and E, Good functional and esthetic outcome at 8 weeks.
Correction of severe ectropion, in which postoperative retraction is combined with excessive eyelid laxity, may require a combination of the 2 techniques, that is, elimination of the cicatricial component and canthal repositioning.
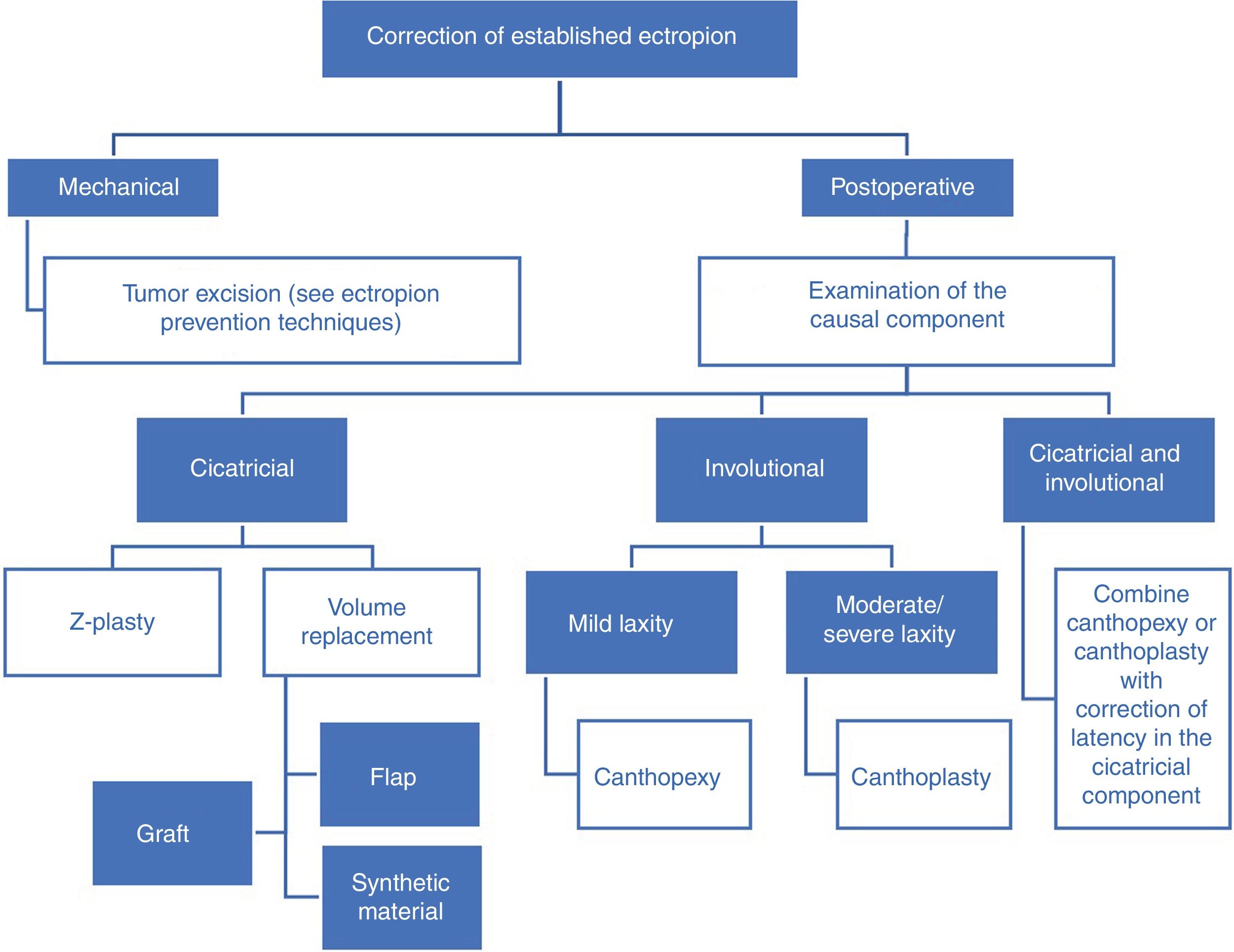
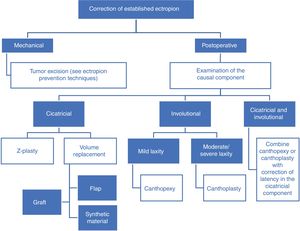
Fig. 9 shows the surgical techniques for repairing ectropion by cause.
ConclusionKnowledge of basic eyelid anatomy and adequate preoperative examination will enable the dermatologic surgeon to design the most effective surgical procedures to avoid ectropion, or, if applicable, choose the best type of repair surgery according to the predominant causal component.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Fernández Canga P, Varas Meis E, Castiñeiras González J, Prada García C, Rodríguez Prieto MÁ. Ectropión en cirugía dermatológica: exploración y técnicas reconstructivas. Actas Dermosifiliogr. 2020;111:229–235.