We herein describe a rare case of discoid lupus erythematosus (DLE) in a patient with alopecia totalis.
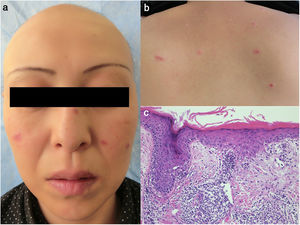
A 42-year-old female developed alopecia on the scalp, which worsened and involved all areas of the scalp 10 years previously. She received various treatments, such as topical corticosteroids, topical carpronium chloride, oral prednisolone, intra-lesional triamcinolone acetonide, and cryotherapy, for five years without success, and thus discontinued therapy a few years previously. She visited the dermatology clinic at Hanawa Kousei Hospital, complaining of asymptomatic facial erythemas which appeared one year previously. Physical examination revealed infiltrative scaly erythemas on the cheek, nose, lips, and upper back (Fig. 1a,b). Total alopecia of the scalp was also observed (Fig. 1a). Her eyebrows fell out, while the eyelashes remained intact. Laboratory examination showed positive anti-nuclear antibody (ANA) (1:1280, speckled), whereas other data such as complete blood count, liver and renal function, serum complement levels, anti-double strand DNA antibody, anti-Sm antibody, anti-SS-A antibody, anti-SS-B antibody, and antiphospholipid antibody were all within normal range. A biopsy specimen taken from the cheek revealed individual cell keratinization, liquefaction of epidermal basal membranes, and focal mononuclear cell infiltration in the dermis (Fig. 1c). Examination by direct immunofluorescence showed linear deposition of IgG, IgM, and C3. A diagnosis of DLE was made. Facial and back erythemas much improved by oral hydroxychloroquine (PlaquenilR, Sanofi, Swiss) (200 mg and 400 mg per alternate day) six months later; however, her alopecia remained unchanged.
(a) Alopecia totalis on the scalp and erythema scattered on the cheek, nose, and lips. (b) Infiltrative erythemas on the upper cheek. (c) A biopsy specimen showing epidermal atrophy, liquefaction of the basement membrane, dyskeratotic epidermal cells, and focal mononuclear cell infiltration in the dermis.
Our patient suffering alopecia totalis developed DLE with nearly nine years’ interval, and alopecia was already stable when the DLE lesions appeared. Her scalp alopecia was non-scarring without erythema, and was therefore not identified as lupus alopecia, although biopsy was not carried out. Alopecia areata is sometimes associated with other autoimmune or allergic diseases, and there has been increased incidence of alopecia areata and lupus erythematosus.1,2 To date, several cases of DLE in association with alopecia have been reported.3,4 Among patients with severe types of alopecia such as alopecia totalis and universalis, thyroid disease was most prevalent, followed by vitiligo, diabetes, atopic dermatitis, dyslipidemia, hypertension, psoriasis, and internal malignancy.5 However, to our knowledge, co-existence of DLE and alopecia totalis has not yet been reported. The present case showed a high titer of ANA (1:1280), suggesting that immunological abnormalities may have developed the DLE. She did not have any other specific autoantibodies, or other symptoms suggestive of systemic autoimmune diseases. Regarding the pathogenesis of alopecia areata, Th2 type cytokine predominance is seen in localized type while Th1 predominance in generalized type.2 Furthermore, recent findings suggest an important role of IL-17 in alopecia;6 however, the role of Th17 cells in DLE remains unclear. The cutaneous inflammatory infiltrates are dominated by Th1, but not Th17 cells, in the DLE lesion.7 A genome-wide study has suggested that several genomic regions are significantly associated with alopecia areata, lupus erythematosus, and other autoimmune diseases. Such immune-mediated imbalance may have contributed to the development of alopecia totalis and DLE in our case. The facial lesions of our patient were eventually improved with hydroxychloroquine, which did not show any effects on the alopecia lesions.
Conflict of interestsThe authors declare that they have no conflict of interest.
Please cite this article as: Yamamoto M, Yamamoto T. Lupus eritematoso discoide en una paciente con alopecia totalis. Actas Dermosifiliogr. 2021;112:77–79.