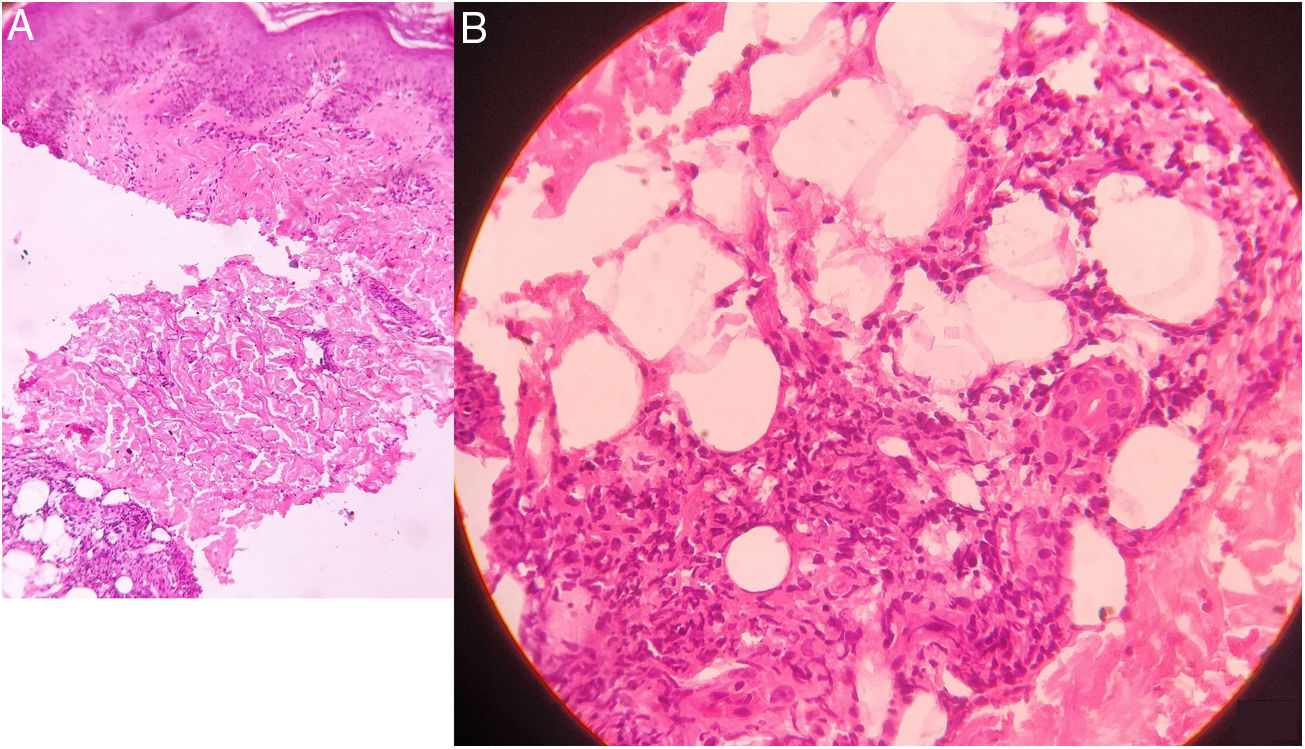
An 11-year-old Indian boy presented with sudden onset of tender, erythematous and edematous plaques with slight vesiculations over face, upper and lower extremities associated with high grade fever and arthralgia along with edema over the hands and feet for 10 days (Fig. 1A and B). His past and family history was non-contributory. On examination he was febrile (39 °C) and his both ulnar nerves were thickened and tender, however the sensations over the lesions were intact. Systemic review and general examination were normal. Laboratory investigations revealed leukocytosis with neutrophilia, and raised ESR; whereas rest all investigations were within normal limits. Biopsy of the lesion revealed infiltration of dermo-epidermal junction by neutrophils, lymphocytes, whereas deeper dermis and subcutaneous tissue showed epitheloid granulomas with fibrinoid necrosis and inflammatory infiltrates consisting neutrophils, lymphocytes and macrophages suggestive of borderline tuberculoid leprosy (BT) in type 2 lepra reaction (T2LR) (Fig. 2). Slit-skin smear taken from the lesion for the acid-fast bacilli was negative. Patient was given multidrug therapy-paucibacillary (MDT-PB) (rifampicin 450 mg one a month and dapsone 50 mg daily) as per WHO guidelines, along with oral steroid 1 mg/kg/per day and tapered according to the response. His skin lesions and constitutional symptoms improved significantly (Fig. 3A and B).
Histology showing infiltration of neutrophils, lymphocytes and plasma cells at the dermo-epidermal junction. Deeper dermis showing distorted epithelioid cell granulomas in fibrinoid necrosis and inflammatory infiltrate of neutrophils, lymphocytes, macrophages and plasma cells. (A- Original magnification X 100, B- Original magnification X 400, Haematoxylin and Eosin stain).
T2LR is an immune complex mediated complication of lepromatous leprosy (LL) and sometimes borderline lepromatous leprosy (BL) and most of it occurs during the first year of MDT.1 It’s characterized by sudden crops of red, tender nodules or plaques, which occasionally become vesicular, pustular, bullous, or necrotic.1 Systemic inflammation in T2LR may affect the nerves, eyes, joints, testes, and lymph nodes. Erythema nodosum leprosum (ENL) is the most common manifestation of T2LR. LL and a bacillary index greater than 4+ are the major risk factors, whereas infections, vaccination, stress pregnancy, lactation, and puberty have also been implicated in T2LR.1
In our patient, the lesions closely mimicked as that of Sweet’s syndrome and presence of fever along with neutrophilia, raised ESR (which are minor criteria to diagnose Sweet’s syndrome)2 added more dilemma. As lepra reactions are followed by surge of inflammatory cells, findings such as fever, leukocytosis, neutrophilia, raised ESR and CRP are common to occur. Moreover, on histology there were numerous neutrophils in the dermis, which is a histological feature of Sweet’s syndrome. Also steroid is quite effective in both the diseases; hence one might get deceived by the improvement of patient’s symptoms. Anesthesia over cutaneous lesions and enlarged and tender peripheral nerves point towards leprosy; and AFB positive bacilli on SSS and specific histopathologic findings aid in confirming the diagnosis. In our patient thickened and tender nerves and typical histology clinched the diagnosis of ENL. Interestingly, in our case, the reactional lesions were the presenting symptoms, as patient did not have a preceding diagnosis of leprosy, whereas most reported cases mimicking Sweet’s syndrome have prior diagnosis of BL or LL.1,3–5
Corticosteroid is the drug of choice in T2LR, whereas thalidomide is the drug of choice for severe ENL. MDT should be started immediately or should be continued if a patient is already taking it. Corticosteroids suppress the inflammatory immune response to M.leprae antigens and also reduce intraneural and cutaneous edema.1,3–5
Awareness of Sweet’s syndrome like T2LR and its prompt diagnosis and treatment is essential to prevent its dreaded sequelae in potentially treatable cases.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Pawar M, Zawar V, Kumavat S. Lepra tuberculoide borderline en paciente con reacción lepromatosa tipo eritema nudoso simulando un síndrome de Sweet. Actas Dermosifiliogr. 2021;112:75–77.