A 2-month-old infant with no personal or family history of interest was referred from a correctional facility for assessment of extensive skin lesions that first appeared in the second week of life. The patient exhibited loss of appetite, was very irritable, and his constant crying interfered with sleep. The patient had not previously been assessed for this condition and no specific treatment had been administered.
Physical ExaminationPhysical examination revealed thick, yellowish, crusted, hyperkeratotic, adherent plaques on the palms (Fig. 1A), soles, and scalp. Diffuse erythema, minute papules, superficial desquamation, and a few erosions were observed on the trunk and limbs (Fig. 1B). All 10 fingernails exhibited onychodystrophy and considerable distal thickening of the nail plate.
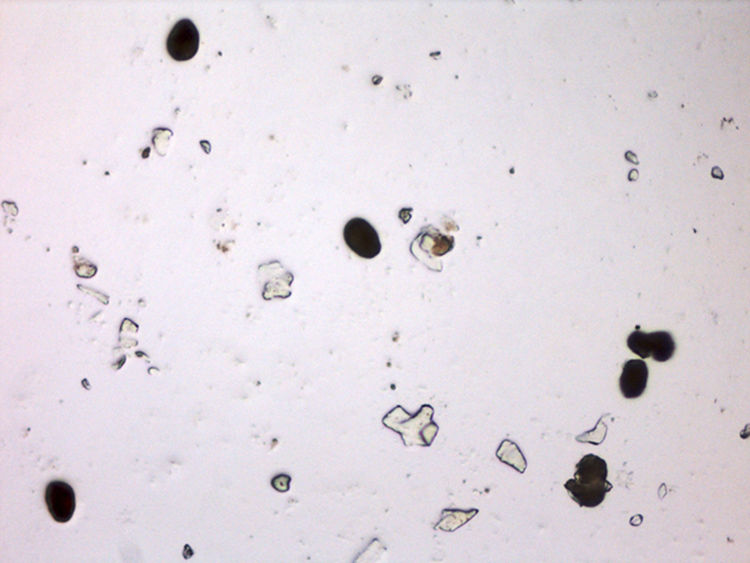
Additional TestsA lesion on the trunk was removed by manual scraping and observed under an optical microscope (Fig. 2).
Laboratory tests revealed marked leukocytosis (27 000 cells/mm3), with 36% eosinophils (absolute count 10 000 cells/mm3). A complete blood count and biochemistry profile showed no other abnormal findings. Levels of IgA, IgG, and IgM were within the normal range. The results of serologic tests for hepatitis B and C, syphilis, and human immunodeficiency virus were negative.
What Is Your Diagnosis?
DiagnosisCrusted or hyperkeratotic scabies in an infant.
Clinical Course and TreatmentThe patient was prescribed 5% permethrin cream, which was applied to the entire body, from the scalp to the feet, except for the perioral region. The first application was carried out in the hospital on the day of the consultation. Seven days later, the treatment was repeated at the correctional facility. After 1 month, the lesions had resolved.
CommentCrusted scabies—also known as hyperkeratotic or Norwegian scabies—is a variant of scabies first described in 1848 by Boeck and Danielssen in a group of Norwegian patients with leprosy. It is a rare, severe form of massive infestation of the ectoparasite Sarcoptes scabiei var. hominis, which also causes classic scabies. The main difference between the two forms is the number of mites per individual, which in the Norwegian variant can exceed 1 million.1
Four weeks after initial contact with the ectoparasite, the host develops a type IV hypersensitivity reaction that limits the spread of the mites. In individuals with crusted scabies, this mechanism is altered, generating an ineffective inflammation and an unbalanced immune response.2 Most cases of Norwegian scabies have been reported in immunocompromised patients; however, an immature immune system, the difficulty of scraping (the mechanism for elimination of mites and burrows), overcrowded living conditions, malnutrition, and institutionalization can lead to the appearance of the disease in newborns and infants.3
The clinical presentation is characterized by the presence of diffuse erythema and desquamation associated with adherent crusts with acral predominance. Onychodystrophy and distal thickening of the nail plate—which can be a reservoir for mites, eggs, and feces—are reported in most cases.4 The lesions associated with classic scabies, such as burrows and pearly vesicles, can be obscured by hyperkeratotic plaques or may not be present.
This atypical clinical presentation delays diagnosis, especially in young children.5 If laboratory tests are carried out, marked eosinophilia is a common finding, possibly with elevated levels of immunoglobulins (especially IgE and IgG). However, simply by scraping off flakes of skin and placing them under an optical microscope—where a large number of mites, eggs, and feces can be observed, as in our patient—a diagnosis of scabies can be confirmed and other entities such as psoriasis, palmoplantar keratoderma, chronic eczema, pityriasis rubra pilaris, Netherton syndrome, and Omenn syndrome can be ruled out.6
It is important that crusted scabies be treated properly to prevent persistence, recurrence, and superinfection of the lesions. The first-line treatment—even in newborns and infants—is 5% permethrin cream, which has a good safety profile due to its low percutaneous absorption. It can be necessary to combine this treatment with the use of topical keratolytics (10% urea cream) or oral ivermectin, which is approved for use in children older than 5 years who weigh more than 15kg (at a dosage of 0.2mg/kg on the first and seventh days of treatment).7 It is fundamental to insist that all members of the household undergo treatment and that fomites and clothing be handled properly.3
Although crusted scabies in infants is exceptionally rare in Spain, dermatologists should be familiar with the clinical presentation of this entity in order to establish the correct diagnosis and begin appropriate treatment, thereby preventing complications and transmission.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Gómez-Zubiaur A, Spanoudi-Kitrimi I, Torrelo A. Eritema difuso e hiperqueratosis acral en un lactante. Actas Dermosifiliogr. 2018;109:741–742.