Allergic contact dermatitis (ACD) is a common disease in daily clinical practice, and its prevalence has increased in recent years. It is characterized clinically by varying degrees of erythema, vesiculation, flaking, and lichenification, though these signs can also be present in other eczematous diseases. Patch testing is the main diagnostic tool to confirm ACD, but its accurate interpretation requires correct correlation with the medical history (details of exposure) and physical examination. We provide a practical and instructive description of the most common clinical patters of ACD depending on the area affected. Knowledge of these patterns will not only help the clinician reach the diagnosis but will suggest possible allergens and forms of contact.
La dermatitis de contacto alérgica (DCA) es una enfermedad frecuente en la práctica clínica diaria, con una prevalencia que ha aumentado en los últimos años. Clínicamente se caracteriza por grados variables de eritema, vesiculación, descamación y liquenificación, signos que también están presentes en otros procesos eccematosos. Las pruebas epicutáneas constituyen la principal herramienta diagnóstica para confirmar una DCA, sin embargo, su correcta interpretación requiere de una correcta correlación entre la anamnesis (historial de exposición) y el examen físico. En este artículo se describen de forma práctica y didáctica los patrones clínicos más frecuentes de DCA dependiendo de su localización. El conocimiento de estos patrones no solo ayudará al clínico en el diagnóstico diferencial, sino que también le permitirá sospechar el posible alérgeno y su forma de aplicación.
Allergic contact dermatitis (ACD) is a common disease in daily practice, and its prevalence has increased in recent years. Clinically, it is characterized by varying degrees of erythema, vesiculation, desquamation, and lichenification, which are also present in other eczematous processes such as atopic eczema, seborrheic eczema, contact eczema, and dyshidrotic eczema.
Given that the clinical and pathological characteristics of these processes are similar, our main tools for classification are the clinical history and physical examination, with emphasis on the location of the lesions. The present article provides a practical and instructive review of the most common clinical patterns of ACD depending on their location. It is important to stress that the description and names proposed to describe these patterns are the fruit of the literature review and the authors’ experience; therefore, they should be used for guidance only and are by no means specific to ACD.
Furthermore, in some cases, a brief comment is made on the most relevant allergens in each region.
ScalpDespite the fact that the scalp is constantly exposed to various everyday allergens, ACD is uncommon at this site. The greater thickness of the epidermis, the absence of folds and wrinkles, and the abundance of pilosebaceous glands all act as the perfect barrier to allergens. Even if a very potent allergen makes contact with the scalp, the most likely finding is that the patient will present symptoms and signs of dermatitis at another site, such as the face, eyelids, or neck.
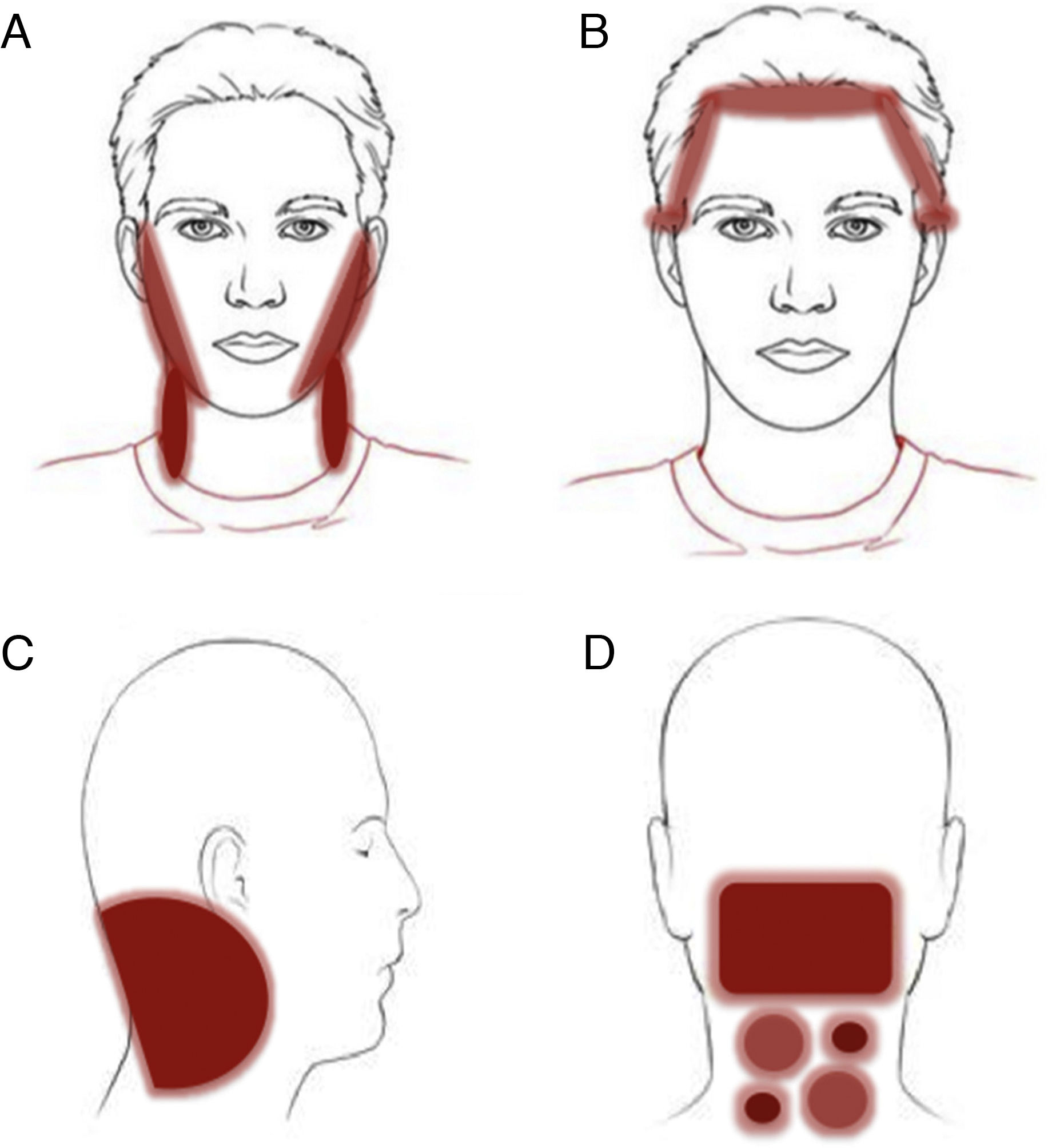
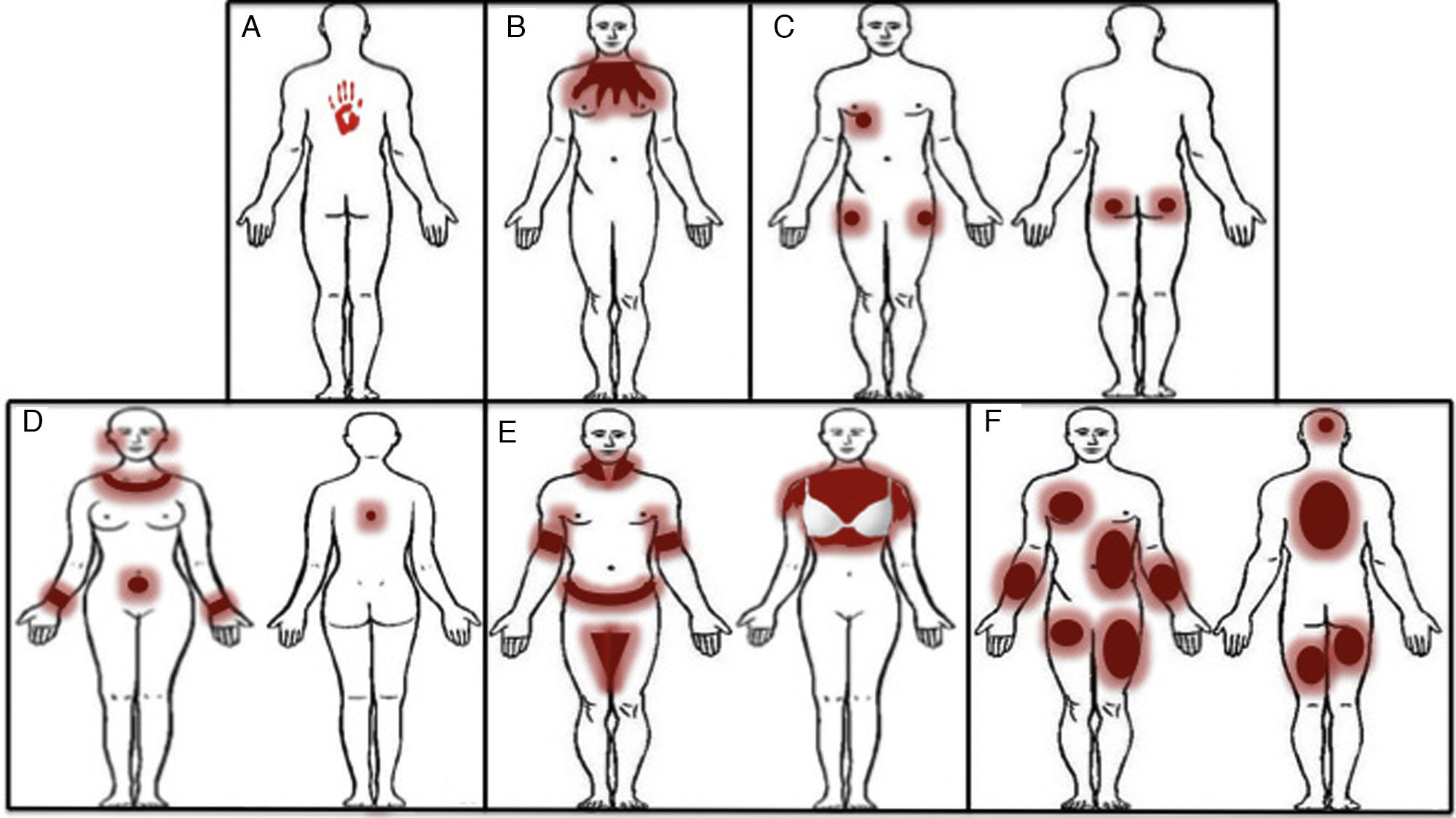
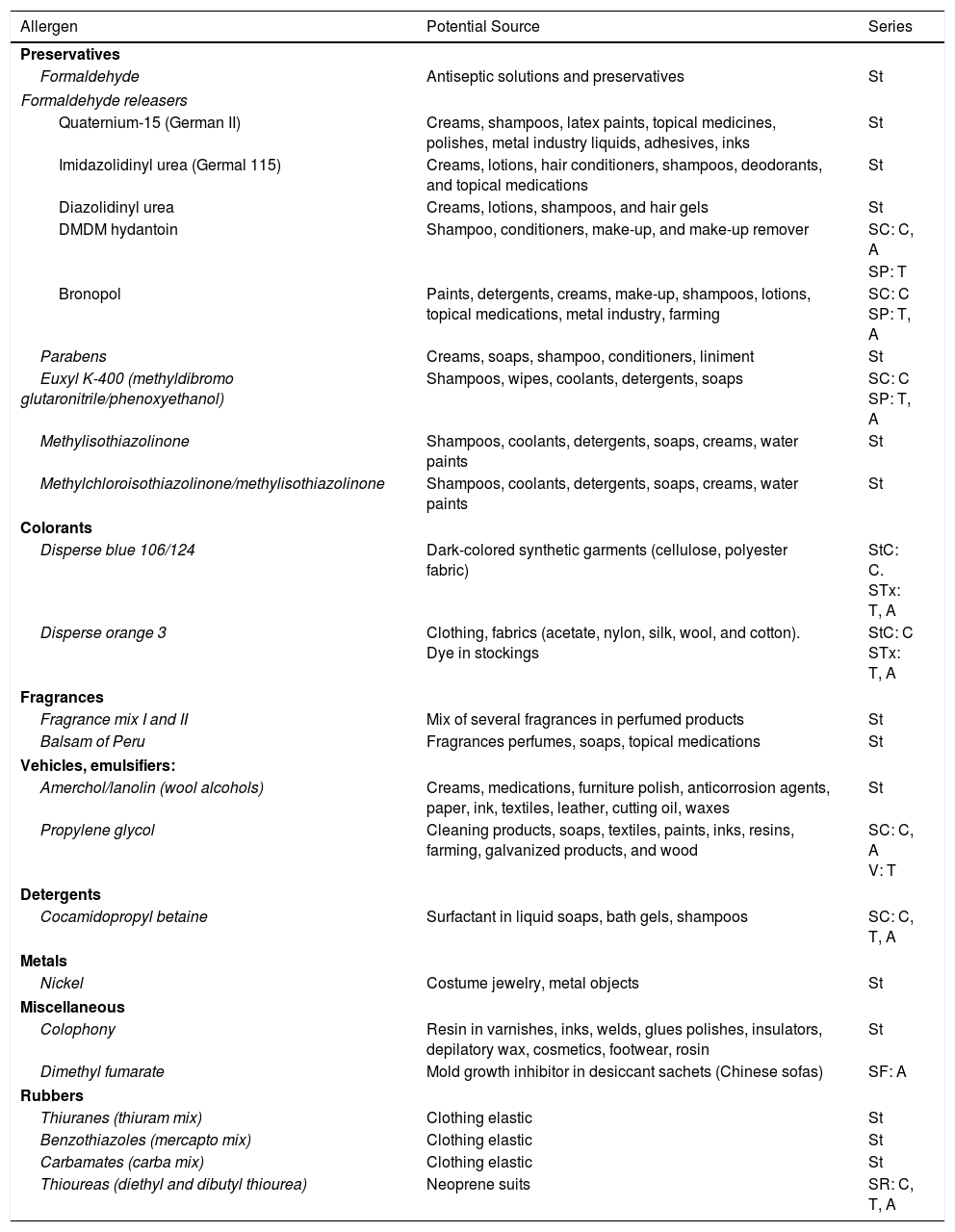
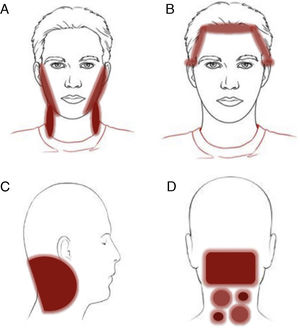
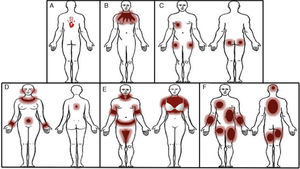
Patterns (Fig. 1)Two of the 3 eczema patterns discussed below actually apply to sites other than the scalp. These are discussed in this section for practical reasons, as they are the areas most affected by the allergen.
Clinical patterns of allergic contact dermatitis affecting the scalp.
A, Rinse-off pattern: eczematous plaques on the sides of the face (preauricular and mandibular) and neck; B, C, and D, pattern along the hairline. B, Forehead and area above the ears. C, Occipital and retroauricular area.
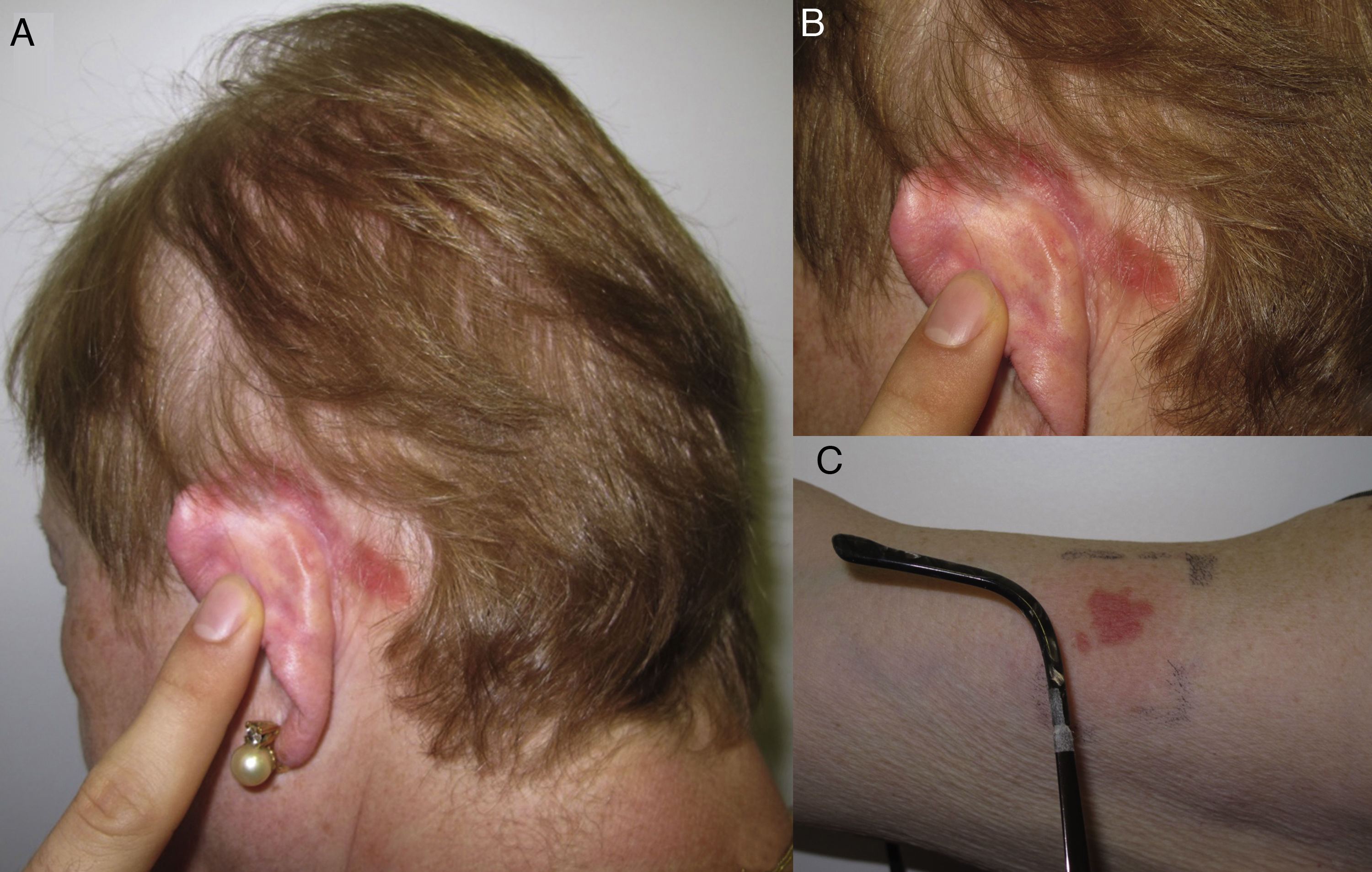
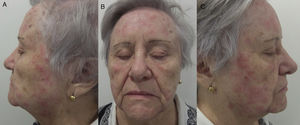
Eczematous plaques on the sides of the face (preauricular and mandibular) and neck. The lesions are produced by the allergen running along the side of the face. The pattern is typical of shampoos, conditioners, and other products that are applied temporarily to the scalp and make brief but recurrent contact with the skin of the face (Fig. 1A and Fig. 2).
Hairline patternEczematous plaques found at the limit between the scalp and the skin of the face, including the forehead, retroauricular region, nape of the neck, and the area above the eyebrows. The pattern is typical of dyes and perming solutions (Figs. 1B, C, and D and Fig. 3).
Geographic patternEczematous plaques confined to the area of contact with the allergen. Typical of objects (Fig. 4).
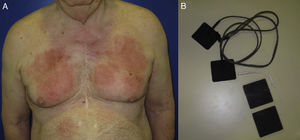
AllergensThe products most frequently described in ACD affecting the scalp are hair dyes, followed by shampoos and conditioners.1 In the case of hair dyes, the most common allergen is paraphenylenediamine, which is an oxidative coloring agent present in many dyes. Its concentration is higher in dark-colored dyes, although it is also found in light-colored dyes and has even been found in some dyes in which the manufacturer does not indicate its presence on the label.2 The symptoms of ACD caused by paraphenylenediamine are very typical and consist of acute edematous dermatitis with considerable involvement of the face, eyelids, and neck and minimal involvement of the scalp3 (Fig. 3). Shampoos and conditioners are uncommon causes of ACD, since rinsing means they have little contact with the skin. They are even well tolerated by sensitized patients.4,5 The most common allergens are fragrances, cocamidopropyl betaine, and preservatives such as quaternium-15.1
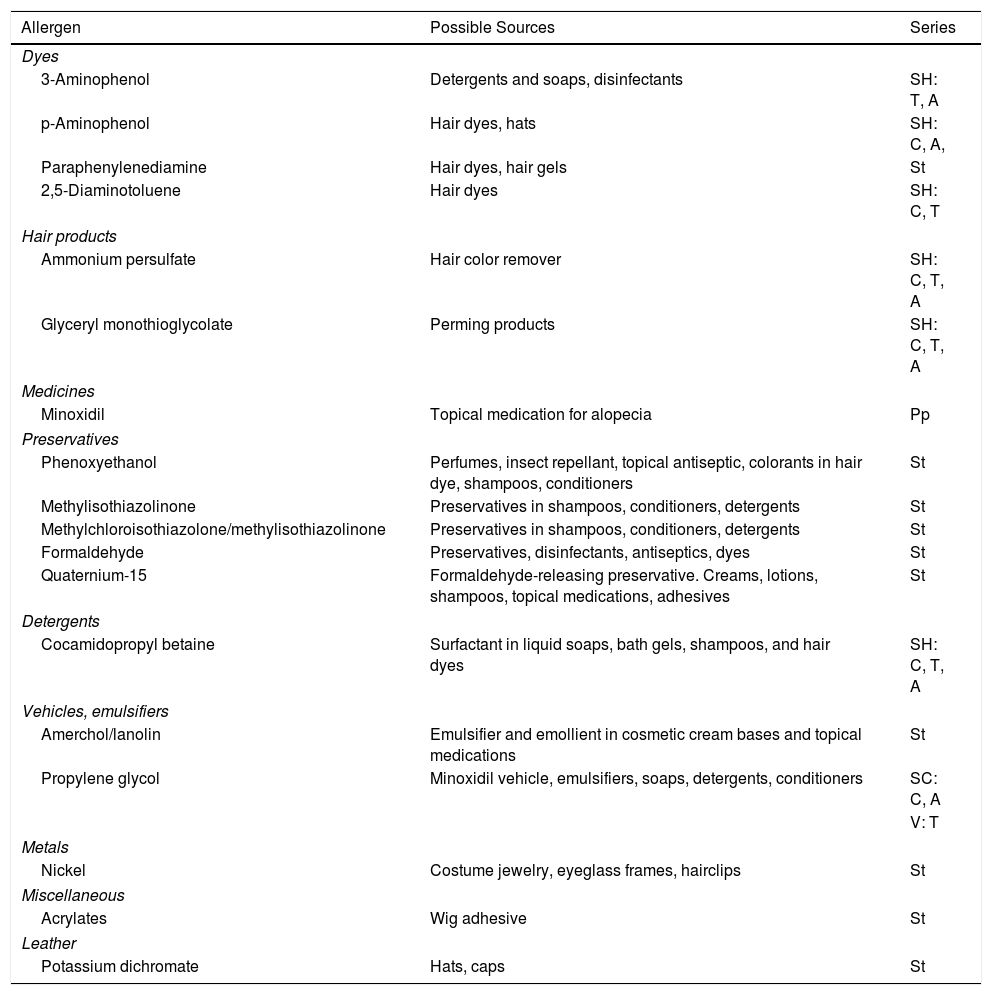
Special mention must be made of lotions containing minoxidil, where the most frequent allergens are propylene glycol, which is used as a vehicle, followed by minoxidil itself.6,7 Typical clinical findings include erythema, pruritus, desquamation, and dryness of the scalp, thus obliging us to make the differential diagnosis with seborrheic dermatitis or psoriasis. Table 1 summarizes the main allergens causing ACD of the scalp.
Most Common Allergens in Contact Dermatitis Affecting the Scalp.
| Allergen | Possible Sources | Series |
|---|---|---|
| Dyes | ||
| 3-Aminophenol | Detergents and soaps, disinfectants | SH: T, A |
| p-Aminophenol | Hair dyes, hats | SH: C, A, |
| Paraphenylenediamine | Hair dyes, hair gels | St |
| 2,5-Diaminotoluene | Hair dyes | SH: C, T |
| Hair products | ||
| Ammonium persulfate | Hair color remover | SH: C, T, A |
| Glyceryl monothioglycolate | Perming products | SH: C, T, A |
| Medicines | ||
| Minoxidil | Topical medication for alopecia | Pp |
| Preservatives | ||
| Phenoxyethanol | Perfumes, insect repellant, topical antiseptic, colorants in hair dye, shampoos, conditioners | St |
| Methylisothiazolinone | Preservatives in shampoos, conditioners, detergents | St |
| Methylchloroisothiazolone/methylisothiazolinone | Preservatives in shampoos, conditioners, detergents | St |
| Formaldehyde | Preservatives, disinfectants, antiseptics, dyes | St |
| Quaternium-15 | Formaldehyde-releasing preservative. Creams, lotions, shampoos, topical medications, adhesives | St |
| Detergents | ||
| Cocamidopropyl betaine | Surfactant in liquid soaps, bath gels, shampoos, and hair dyes | SH: C, T, A |
| Vehicles, emulsifiers | ||
| Amerchol/lanolin | Emulsifier and emollient in cosmetic cream bases and topical medications | St |
| Propylene glycol | Minoxidil vehicle, emulsifiers, soaps, detergents, conditioners | SC: C, A |
| V: T | ||
| Metals | ||
| Nickel | Costume jewelry, eyeglass frames, hairclips | St |
| Miscellaneous | ||
| Acrylates | Wig adhesive | St |
| Leather | ||
| Potassium dichromate | Hats, caps | St |
Abbreviations: A, allergEAZE; C, Chemotechnique; Pp, own product; SC, supplementary cosmetic series; SH, supplementary hairdressing series; St, standard series of the Spanish Contact Dermatitis and Skin Allergy Research Group (GEIDAC); T, Trolab; V, supplementary vehicle series.
The face is constantly exposed to environmental allergens, thus making it one of the sites most frequently affected by ACD, especially in women. Allergens can reach the face directly and indirectly (ie, via the hands, scalp, and air).
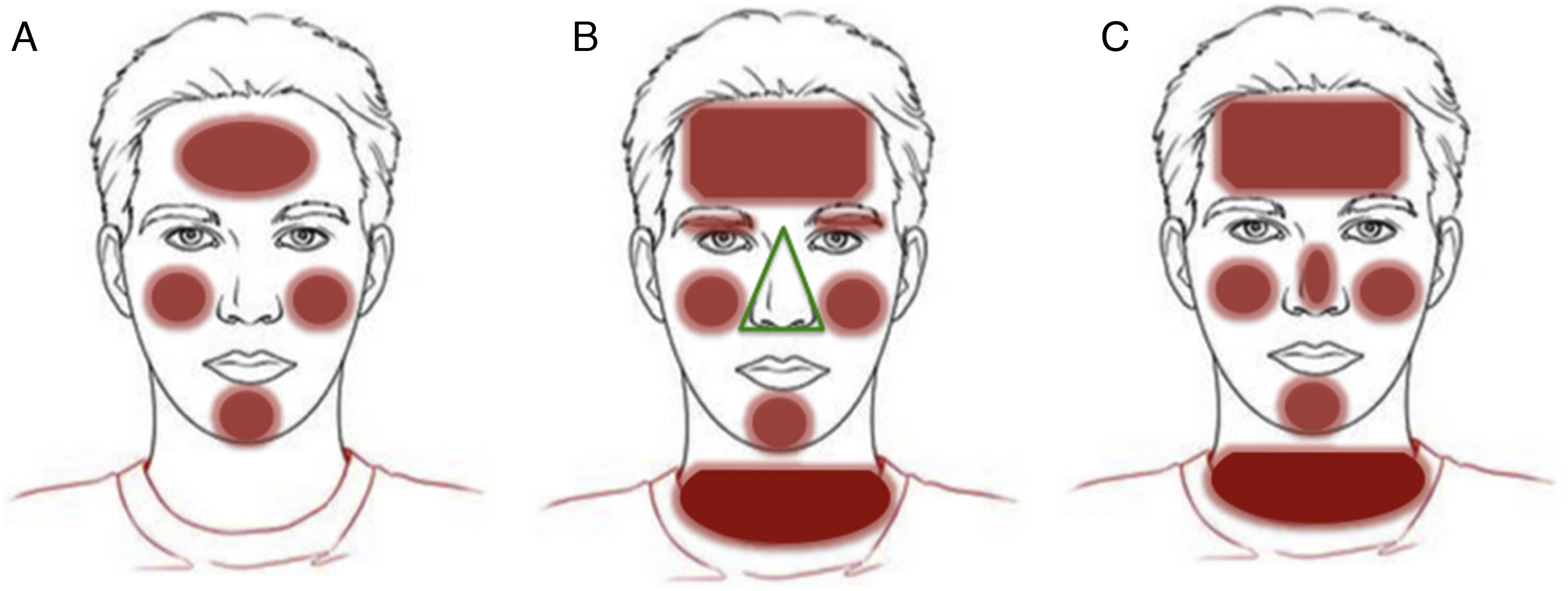
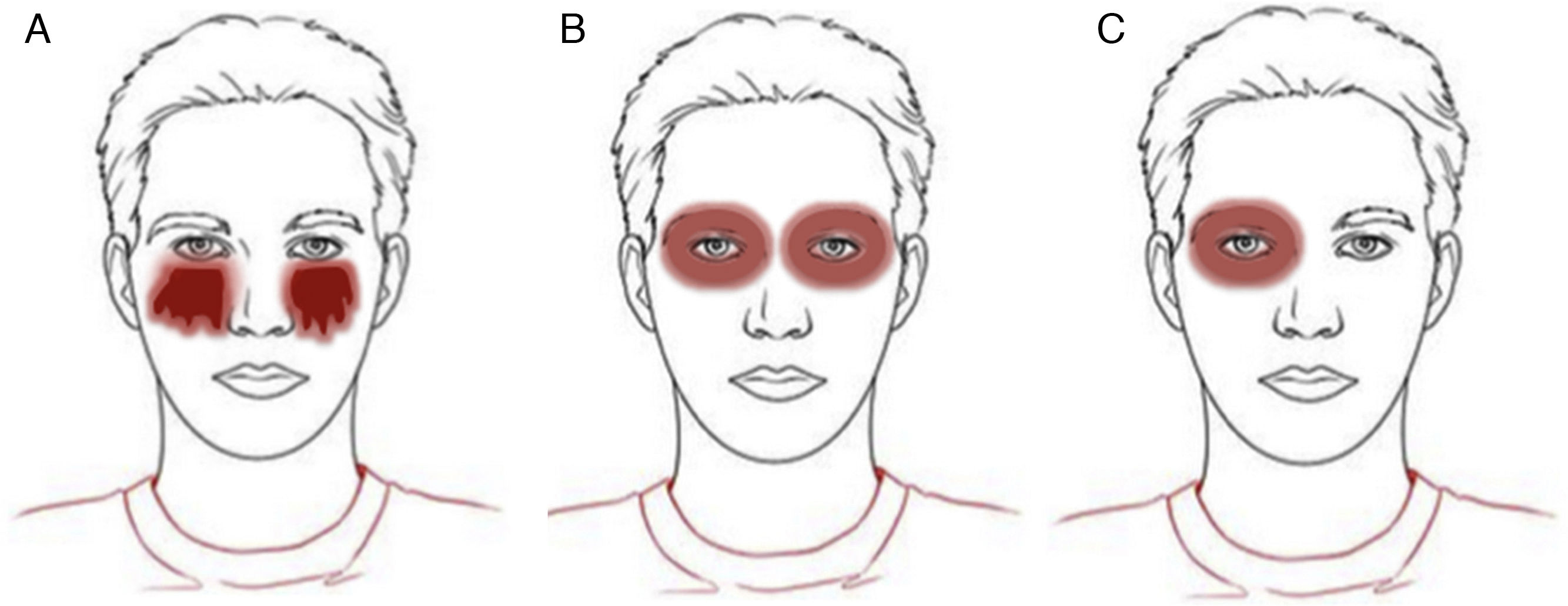
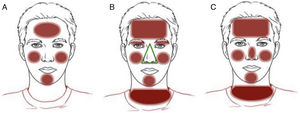
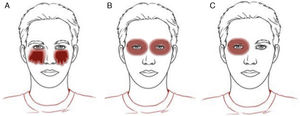
Patterns (Fig. 5)Bilateral patchy patternEczematous plaques arranged in patches on both sides of the face, that is, with some areas of skin unaffected. The pattern reflects the direct application of an allergen, generally a cosmetic product. Even if the product is applied homogeneously all over the face, it usually produces lesions on some parts and not on on others (Fig. 5A and Fig. 6).
See section on scalp.
Geometric patternEczematous plaques confined to the area of contact with the allergen. Typical of objects.
Airborne patternEczematous plaques that symmetrically affect areas exposed to the air. The most typically affected areas are the upper eyelids, the nasolabial fold, the retroauricular area, the submental area, and the intermammary area. In contrast with the photoallergic pattern, the bridge and tip of the nose are not usually affected (“beak sign”),8 probably because of the more pronounced activity of the sebaceous glands on the bridge of the nose, which hinder penetration of water-soluble allergens and subsequent development of lesions. This pattern is produced by allergens that can be transmitted in the form of powder, drops, or gas (Fig. 5B and Fig. 7).
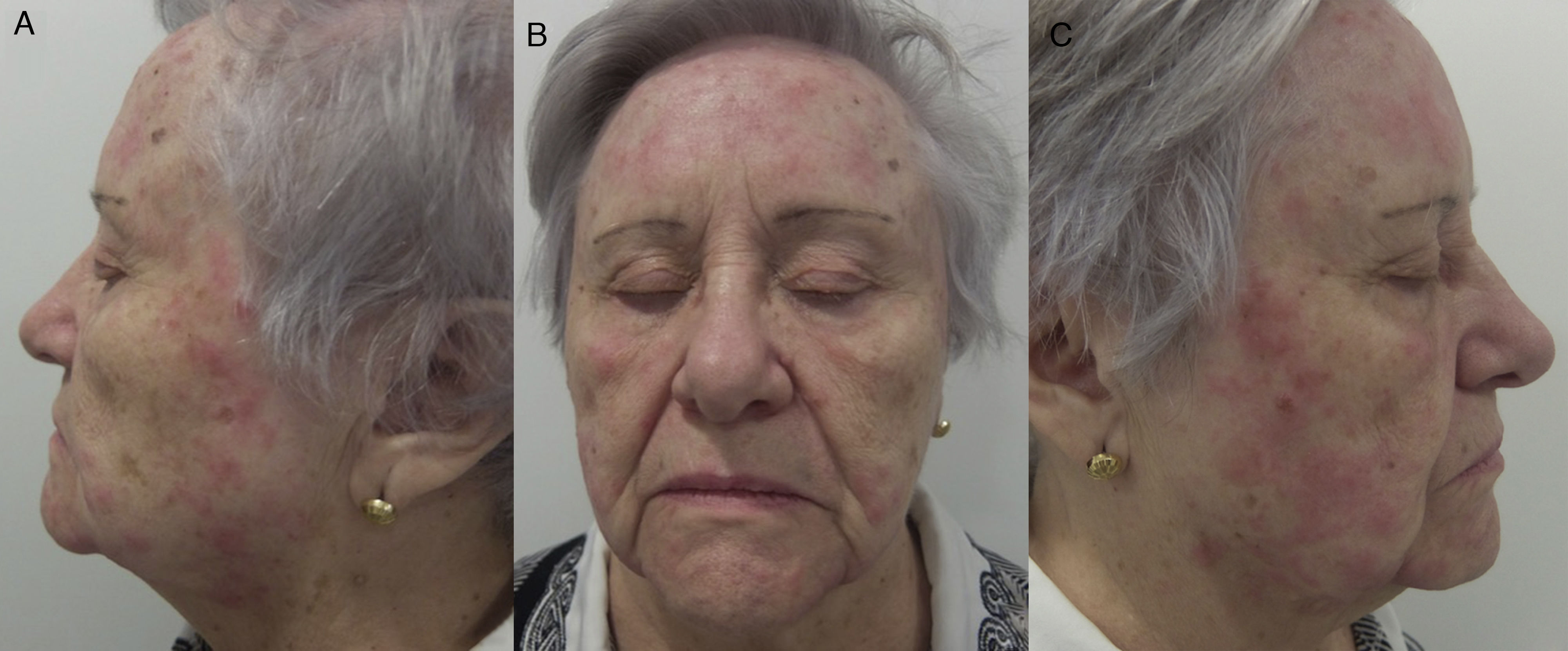
Photoallergic patternEczematous plaques symmetrically affecting areas of the body exposed to sunlight. The face is generally the main and only area affected. The bridge of the nose is involved, although the upper eyelids, retroauricular area, submental area, and areas covered by hair or clothing are spared (Fig. 5C and Fig. 8).
Photoallergic contact dermatitis. In contrast with the airborne pattern (Fig. 7), the eyelids are not affected, whereas the tip and bridge of the nose are.
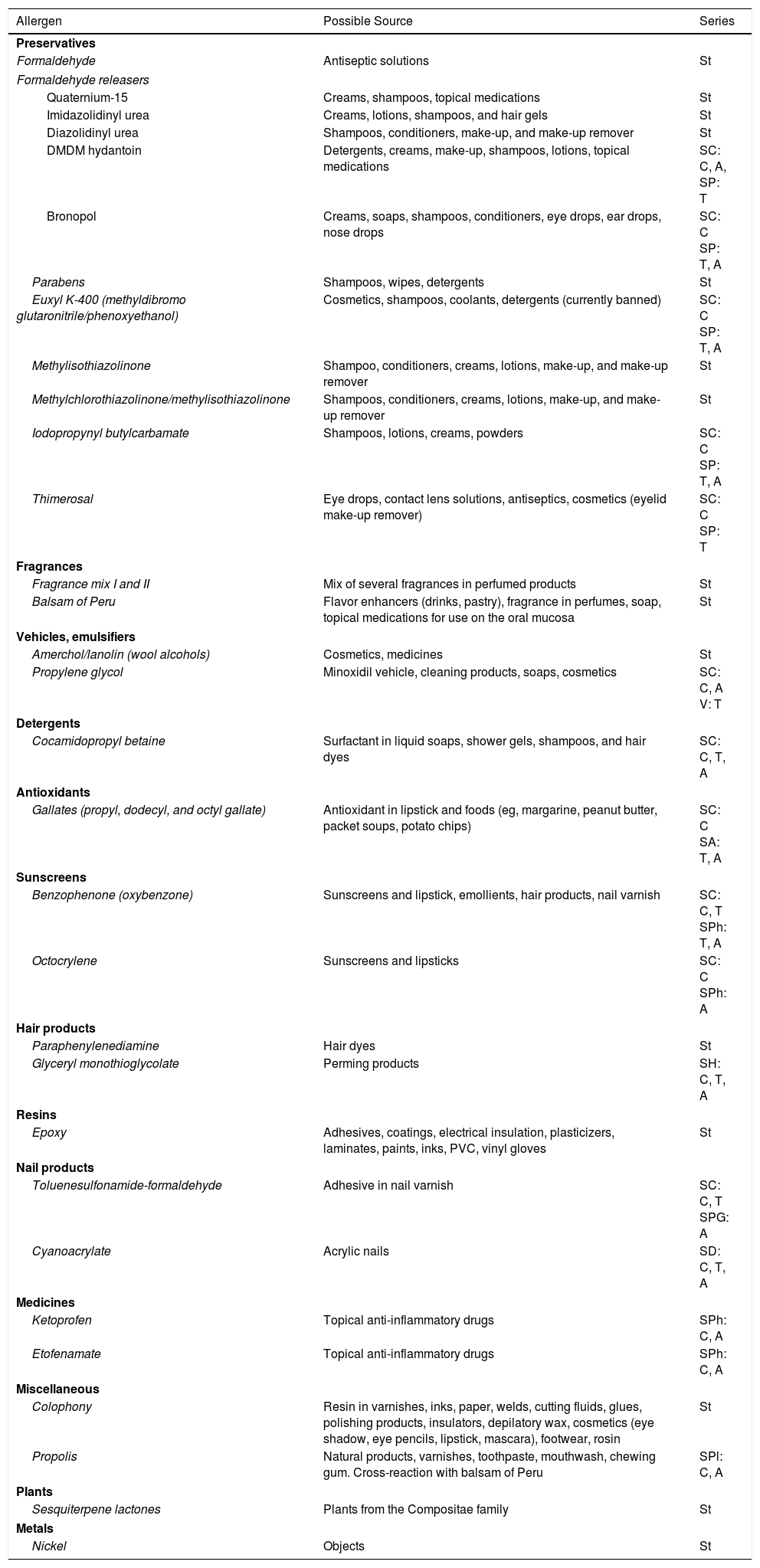
The allergens causing the bilateral patchy pattern are generally found in hygiene and moisturizing products.9,10 The list of potential allergens is very long and can be divided into 2 major groups: preservatives and fragrances. Within the preservatives, Kathon CG seems to be the most frequently involved in all series.9,10 Kathon CG is a 3:1 mixture of methylchloroisothiazolinone and methylisothiazolinone. This very efficient preservative is present in many products, such as moisturizing creams, gels, and shampoos.11 Sensitization to Kathon CG has become increasingly common in recent years. Therefore, in 2005, use of the preservative methylisothiazolinone alone was proposed to reduce sensitivity. However, this approach was unsuccessful, and methylisothiazolinone became Allergen of the Year in 2013 in Europe.12 With respect to fragrances, it is noteworthy that these substances are found not only in perfumes, but also in cosmetic products to make them more pleasant. The main allergens are summarized in Table 2.9–13 It is important to remember that the standard European series only detects some 50% of cases of ACD to cosmetics,9,10 thus making it necessary to perform patch tests with the patient's own products.
Most Common Allergens in Contact Dermatitis Affecting the Face.
| Allergen | Possible Source | Series |
|---|---|---|
| Preservatives | ||
| Formaldehyde | Antiseptic solutions | St |
| Formaldehyde releasers | ||
| Quaternium-15 | Creams, shampoos, topical medications | St |
| Imidazolidinyl urea | Creams, lotions, shampoos, and hair gels | St |
| Diazolidinyl urea | Shampoos, conditioners, make-up, and make-up remover | St |
| DMDM hydantoin | Detergents, creams, make-up, shampoos, lotions, topical medications | SC: C, A, SP: T |
| Bronopol | Creams, soaps, shampoos, conditioners, eye drops, ear drops, nose drops | SC: C SP: T, A |
| Parabens | Shampoos, wipes, detergents | St |
| Euxyl K-400 (methyldibromo glutaronitrile/phenoxyethanol) | Cosmetics, shampoos, coolants, detergents (currently banned) | SC: C SP: T, A |
| Methylisothiazolinone | Shampoo, conditioners, creams, lotions, make-up, and make-up remover | St |
| Methylchlorothiazolinone/methylisothiazolinone | Shampoos, conditioners, creams, lotions, make-up, and make-up remover | St |
| Iodopropynyl butylcarbamate | Shampoos, lotions, creams, powders | SC: C SP: T, A |
| Thimerosal | Eye drops, contact lens solutions, antiseptics, cosmetics (eyelid make-up remover) | SC: C SP: T |
| Fragrances | ||
| Fragrance mix I and II | Mix of several fragrances in perfumed products | St |
| Balsam of Peru | Flavor enhancers (drinks, pastry), fragrance in perfumes, soap, topical medications for use on the oral mucosa | St |
| Vehicles, emulsifiers | ||
| Amerchol/lanolin (wool alcohols) | Cosmetics, medicines | St |
| Propylene glycol | Minoxidil vehicle, cleaning products, soaps, cosmetics | SC: C, A V: T |
| Detergents | ||
| Cocamidopropyl betaine | Surfactant in liquid soaps, shower gels, shampoos, and hair dyes | SC: C, T, A |
| Antioxidants | ||
| Gallates (propyl, dodecyl, and octyl gallate) | Antioxidant in lipstick and foods (eg, margarine, peanut butter, packet soups, potato chips) | SC: C SA: T, A |
| Sunscreens | ||
| Benzophenone (oxybenzone) | Sunscreens and lipstick, emollients, hair products, nail varnish | SC: C, T SPh: T, A |
| Octocrylene | Sunscreens and lipsticks | SC: C SPh: A |
| Hair products | ||
| Paraphenylenediamine | Hair dyes | St |
| Glyceryl monothioglycolate | Perming products | SH: C, T, A |
| Resins | ||
| Epoxy | Adhesives, coatings, electrical insulation, plasticizers, laminates, paints, inks, PVC, vinyl gloves | St |
| Nail products | ||
| Toluenesulfonamide-formaldehyde | Adhesive in nail varnish | SC: C, T SPG: A |
| Cyanoacrylate | Acrylic nails | SD: C, T, A |
| Medicines | ||
| Ketoprofen | Topical anti-inflammatory drugs | SPh: C, A |
| Etofenamate | Topical anti-inflammatory drugs | SPh: C, A |
| Miscellaneous | ||
| Colophony | Resin in varnishes, inks, paper, welds, cutting fluids, glues, polishing products, insulators, depilatory wax, cosmetics (eye shadow, eye pencils, lipstick, mascara), footwear, rosin | St |
| Propolis | Natural products, varnishes, toothpaste, mouthwash, chewing gum. Cross-reaction with balsam of Peru | SPl: C, A |
| Plants | ||
| Sesquiterpene lactones | Plants from the Compositae family | St |
| Metals | ||
| Nickel | Objects | St |
Abbreviations: A, allergEAZE; C, Chemotechnique; SA, supplementary antioxidant series; SC, supplementary cosmetic series; SD, supplementary dental series; SH, supplementary hairdressing series; SP, supplementary preservative series; SPG, supplementary plastic and glue series; SPh, supplementary photoallergic series; SPl, supplementary plant series; St, standard series of the Spanish Contact Dermatitis and Skin Allergy Research Group (GEIDAC); T, Trolab; V, supplementary vehicle series.
The allergens causing the rinse-off pattern are addressed in the section on the scalp. The geographic pattern can be produced by several allergens, depending on the object that comes into contact with the skin.
Most cases involving the airborne pattern are occupational, with the main allergens being those present in medicines, plants, and resins.14 Airborne ACD to medicines generally affects health professionals and carers, who are responsible for crushing tablets for patients with difficulty swallowing.14 The main allergens in plants are sesquiterpene lactones from the Compositae family, which mainly affect people who work in the open air.15 In the case of resins, the main allergen is epoxy resin, which has high sensitizing potency. Resins have several uses and are found in paints and finishing products, immersion oils, adhesives, coating used in electrical equipment, and material used in sports articles, aeronautical applications, and even in medical products such as dental prostheses and pacemakers. ACD mainly affects workers in the industries where these products are manufactured.14
The allergens most frequently involved in the photoallergic pattern are topical anti-inflammatory drugs such as ketoprofen and etofenamate and sunscreens such as octocrylene and benzophenone-3.16–18
EyelidsThe eyelids are particular interesting area. They are at high risk of ACD owing to frequent exposure, a thinner epidermis, and trapping of allergens by the orbicularis muscles. Diagnosis is not easy, however, since eyelid ACD often presents with nonspecific symptoms (eg, pruritus, edema, and pain), which are also observed in processes such as seborrheic dermatitis, atopic dermatitis, rosacea, dermatomyositis, allergic conjunctivitis, and psoriasis. ACD is the main cause of eyelid dermatitis, affecting 50% of cases, especially if the face or another area of the body is involved.19–22
Patterns (Fig. 9)It is important to remember that eyelid ACD occurs more frequently after application of products on the scalp or face than after direct application on the eyelids.10,23 In addition, symptoms rarely appear at the sites of direct application, thus further hampering diagnosis. Therefore, when assessing a patient with eyelid eczema, in addition to considering patterns of direct application, we should include an evaluation of patterns on the scalp and face and the airborne pattern.
Eczematous plaques on the lower eyelids and cheeks. Typical of eye drops (the upper eyelids may be involved) (Fig. 9A and Fig. 10).
Contour patternEczematous plaques on the eyelids and periorbital region, more frequently affecting the upper eyelids and indicating direct application of cosmetic around the eyes. Typical of eye shadow, mascara, and moisturizing creams (Fig. 9B and Fig. 11).
Unilateral patternEczematous plaques affecting one eyelid and not the other. While not specific, this finding can point us towards ectopic ACD caused by transfer of allergens from the hands (Fig. 9C).
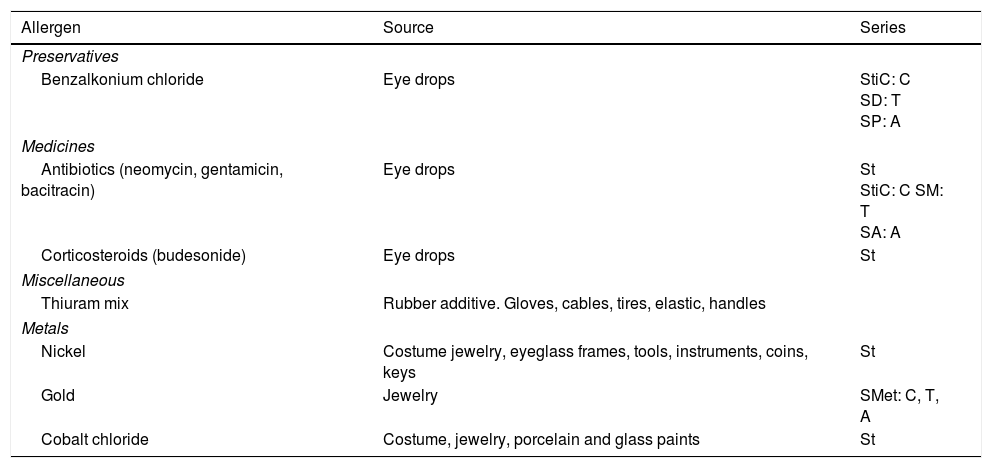
AllergensThe allergens responsible are many and varied and depend on the series studied.10,23,24 It is important to remember that the allergens can reach the eyelids via several routes (direct, indirect, airborne). Directly applied allergens are generally very similar to those found in ACD to cosmetics mentioned in the section on the face, that is, mainly preservatives and fragrances. However, in the case of eyelid ACD, we must remember that in some series, nickel is the most frequently involved allergen.23 Nickel can be found directly in cosmetic products containing colorants, for example, mascara, eye pencils, and eye shadow,25 or indirectly, for example, as a contaminant of a cosmetic or its container.26 Of note, many articles used to enhance the eyelashes (eg, eyelash curlers) contain nickel,27 which can also reach the eyelids ectopically, for example, through metallic nail files, contact with coins or keys,28,29 or after application of nail varnish or metallic nail polish containing nickel.30 As for the allergens in eye drops, the most relevant are preservatives and some medications.10,23,24,31 The main allergens in preservatives are benzalkonium chloride and thiomersal, and the main drugs involved are parasympathomimetic and sympathomimetic agents, carbonic anhydrase inhibitors, and adrenergic ß-blockers.10,23,32 The main indirectly applied allergens are those associated with nail enhancement products, such as the resin p-toluenesulfonamide formaldehyde (found in some polishes), acrylates (used as glue for artificial nails), and methacrylates (component of the paste of so-called porcelain nails).23,33 Lastly, it is worth mentioning gold, which is an uncommon allergen in ACD at other sites, although some series consider it the main allergen in isolated eyelid ACD.34 When gold in jewelry (eg, rings) comes into contact with certain particles, such as titanium dioxide (used in physical sunscreens or as an opacifier in some cosmetics), it releases ions that can cause ACD.35Table 3 summarizes the allergens that most commonly affect the eyelids, excluding those already mentioned in the section on the face.
Most Common Allergens in Contact Dermatitis Affecting the Eyelids.
| Allergen | Source | Series |
|---|---|---|
| Preservatives | ||
| Benzalkonium chloride | Eye drops | StiC: C SD: T SP: A |
| Medicines | ||
| Antibiotics (neomycin, gentamicin, bacitracin) | Eye drops | St StiC: C SM: T SA: A |
| Corticosteroids (budesonide) | Eye drops | St |
| Miscellaneous | ||
| Thiuram mix | Rubber additive. Gloves, cables, tires, elastic, handles | |
| Metals | ||
| Nickel | Costume jewelry, eyeglass frames, tools, instruments, coins, keys | St |
| Gold | Jewelry | SMet: C, T, A |
| Cobalt chloride | Costume, jewelry, porcelain and glass paints | St |
Abbreviations: A, allergEAZE; C, Chemotechnique; SA, supplementary antibiotic series; SD, supplementary disinfectant series; SM, supplementary medication series; SMet, supplementary metal series; SP, supplementary preservative series; St, standard series of the Spanish Contact Dermatitis and Skin Allergy Research Group (GEIDAC); StiC, Chemotechnique international standard supplementary series; T, Trolab.
Hand dermatitis or eczema is a common condition, with an annual estimated prevalence of 10% in the general population.36 This prevalence can be explained by the fact that our hands come into frequent contact with many products during our lifetime. The differential diagnosis between ACD, irritant contact dermatitis (ICD), and other inflammatory processes affecting the hands, such as psoriasis or dyshidrotic eczema, is difficult, since the morphology of the lesions, and even the histology findings, rarely enable us to differentiate between one process and another. The main risk factor that predisposes to contact dermatitis of the hand is repeated exposure of the skin to water and moisture. This exposure causes maceration of the stratum corneum and impairment of the skin barrier, thus rendering it more susceptible to irritants and potential allergens. We comment on clinical patterns, which, when combined with the clinical history, can indicate that the patient has contact eczema. Other findings that can point to a potential diagnosis of ACD include the following:
- •
Pruriginous vesicles on erythematous skin.
- •
Eczema at other sites (skin, eyelids).
- •
Change in a stable hand eczema pattern.
It is important to remember that these findings are not always present; therefore, as recommended in European guidelines on hand eczema, we should perform patch tests on all patients with chronic hand eczema as a method of diagnosing hand ACD.37,38
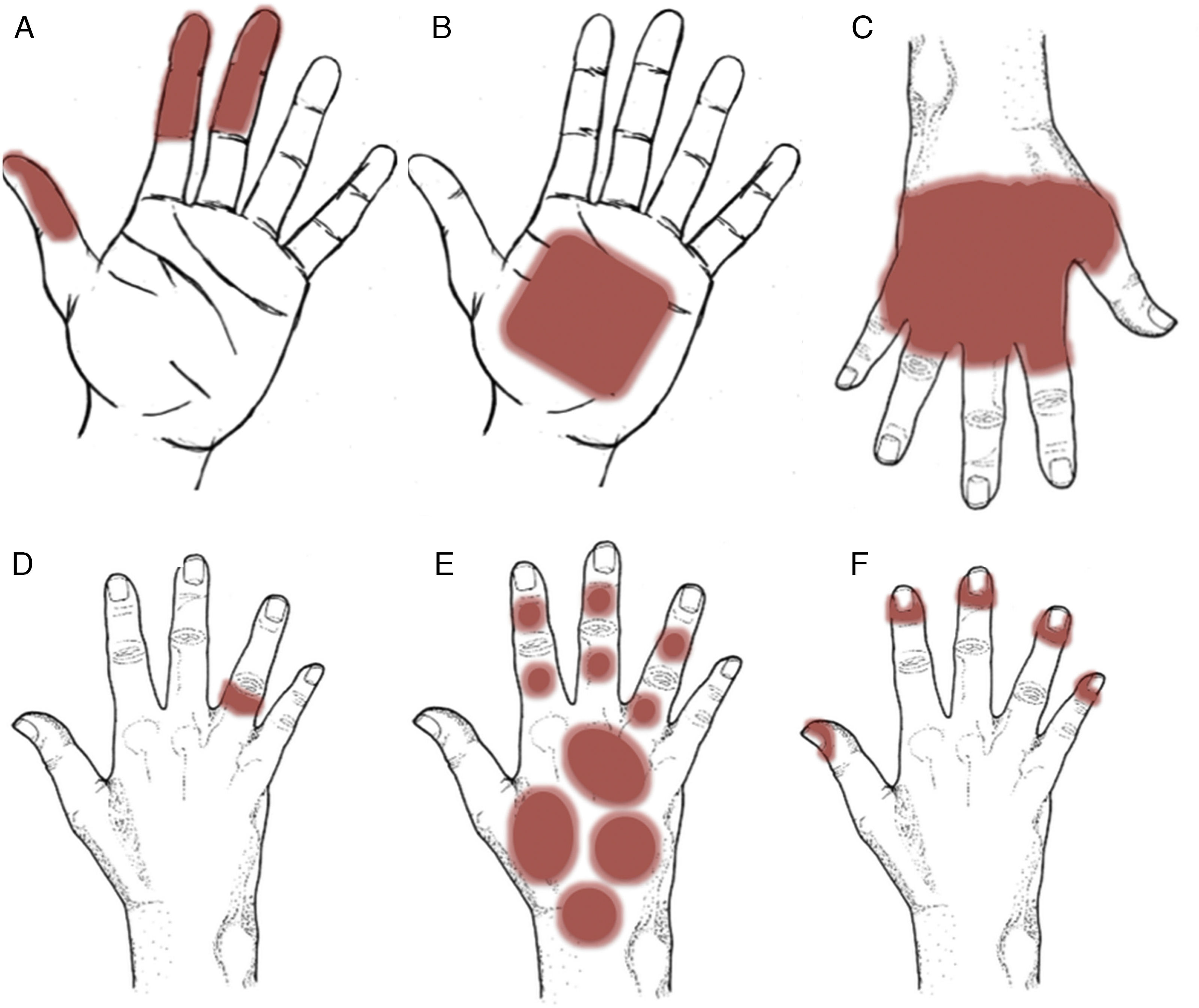
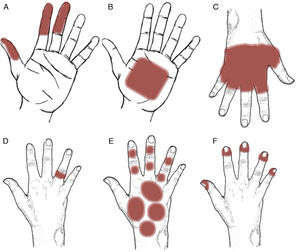
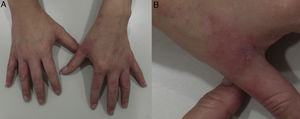
Patterns (Fig. 12)Pincer grasp patternEczematous plaques affecting the finger that make the pincer movement (thumb, ring finger, and, sometimes, middle finger). Typical of frictional ICD (repeated contact with money, paper, etc.), although this can also be observed in occupational ACD, as observed with dentists (acrylates),39,40 florists (plants),15,41 and cooks (foods)15,42 (Fig. 12A).
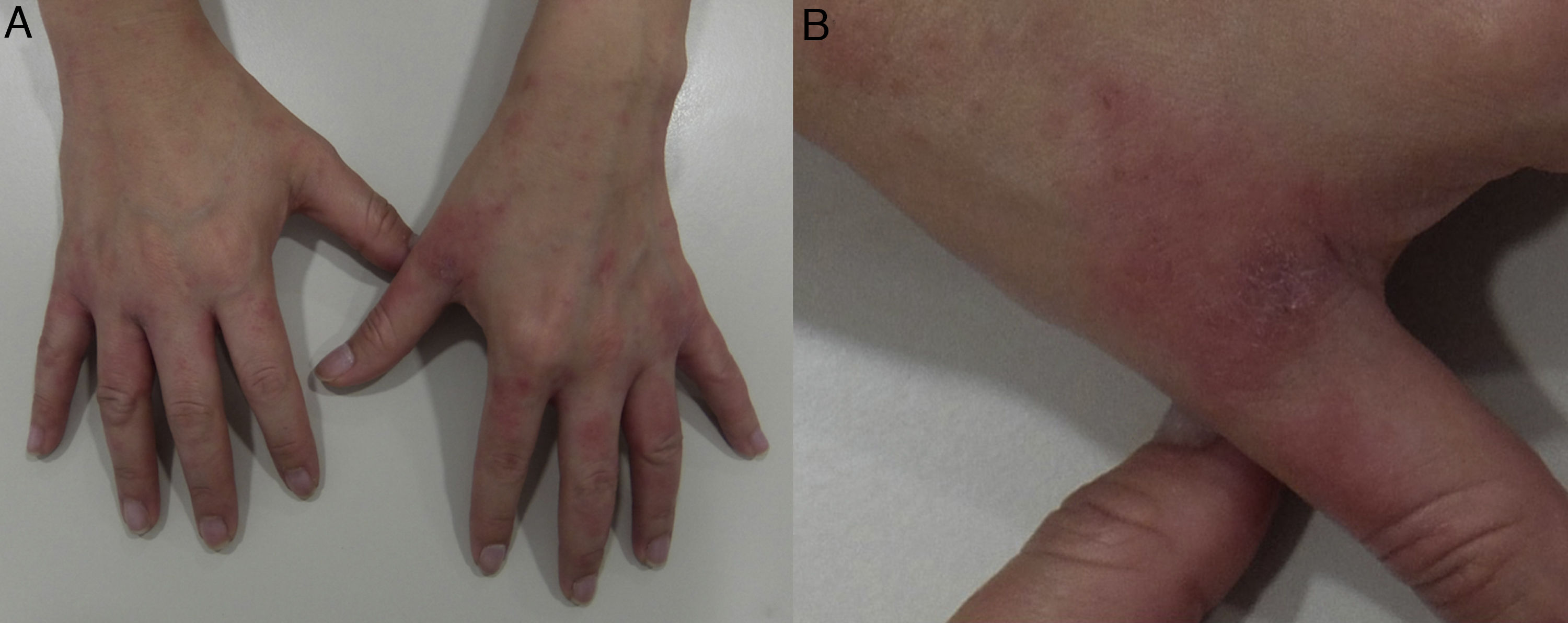
Palmar grasp patternEczematous plaques on the palm. The pattern occurs with objects that come into contact with the palm, such as cellphones, computer mouses, stair-rails, and gear shifts.43,44 The differential diagnosis should be with psoriasis and dyshidrotic eczema. Involvement of the skin on the dorsum of the hands and wrists points to ACD (Fig. 12B and Fig. 13).
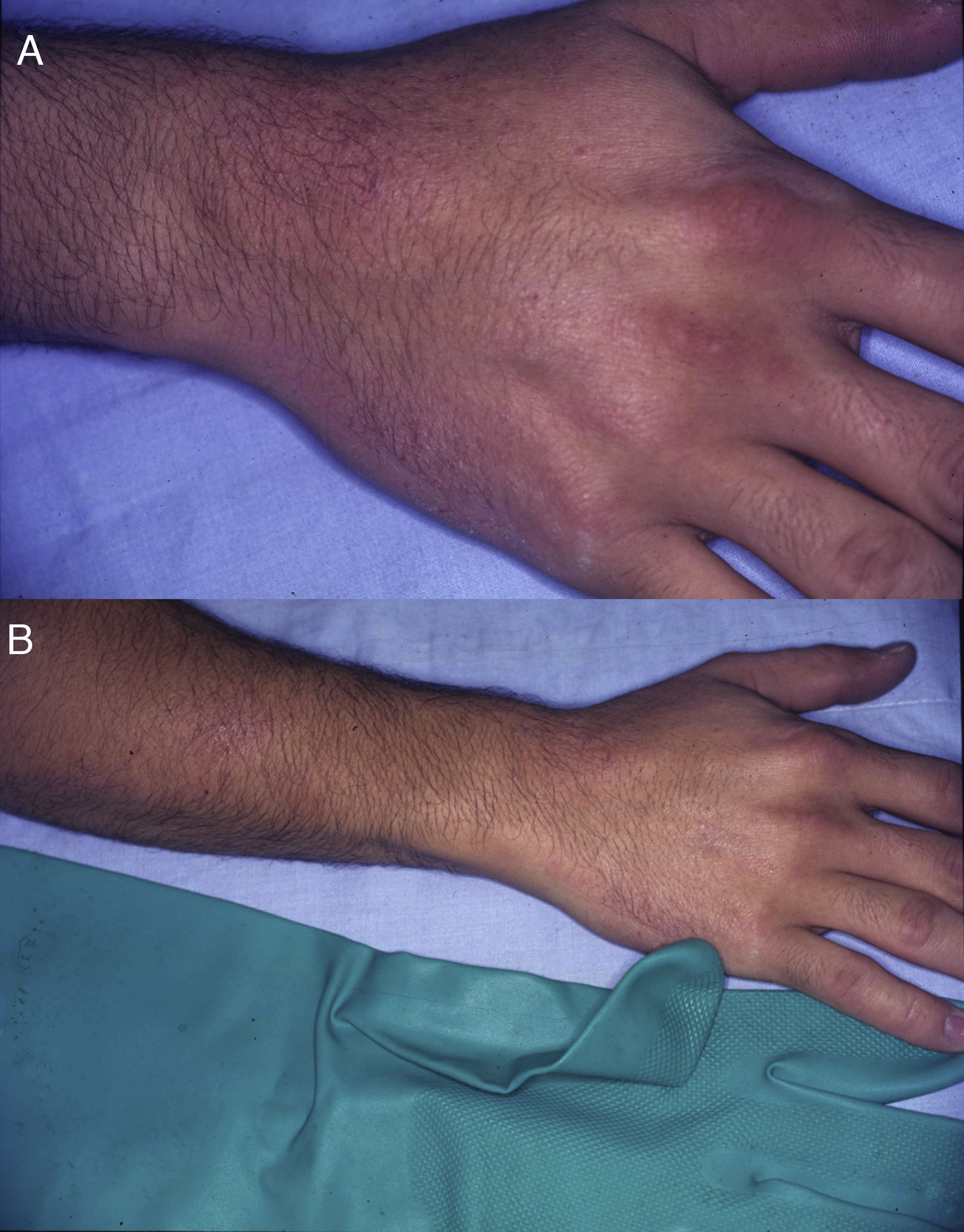
Apron patternEczematous plaques that generally first manifest in the interdigital spaces of the dorsum of the hand before extending over the palmar and dorsal surfaces. This pattern is typical of ICD in cleaners who regularly come into contact with water45 (Fig. 12C and Fig. 14).
Ring patternEczematous plaques that affect the skin under a ring. This pattern is generally secondary to ICD. Metals or fragrances should be taken into consideration when ACD is suspected (Fig. 12D and Fig. 15).
Glove patternEczematous plaques arranged in a patched pattern affecting the dorsum of the hands and wrists. The dorsum of the forearm may also be affected. Unlike the apron pattern, the glove pattern usually spares the interdigital spaces43,46 (Fig. 12E and Fig. 16).
Periungual patternEczema that affects the periungual area. Typical of products used to enhance the nails10,47 (Fig. 12F and Fig. 17).
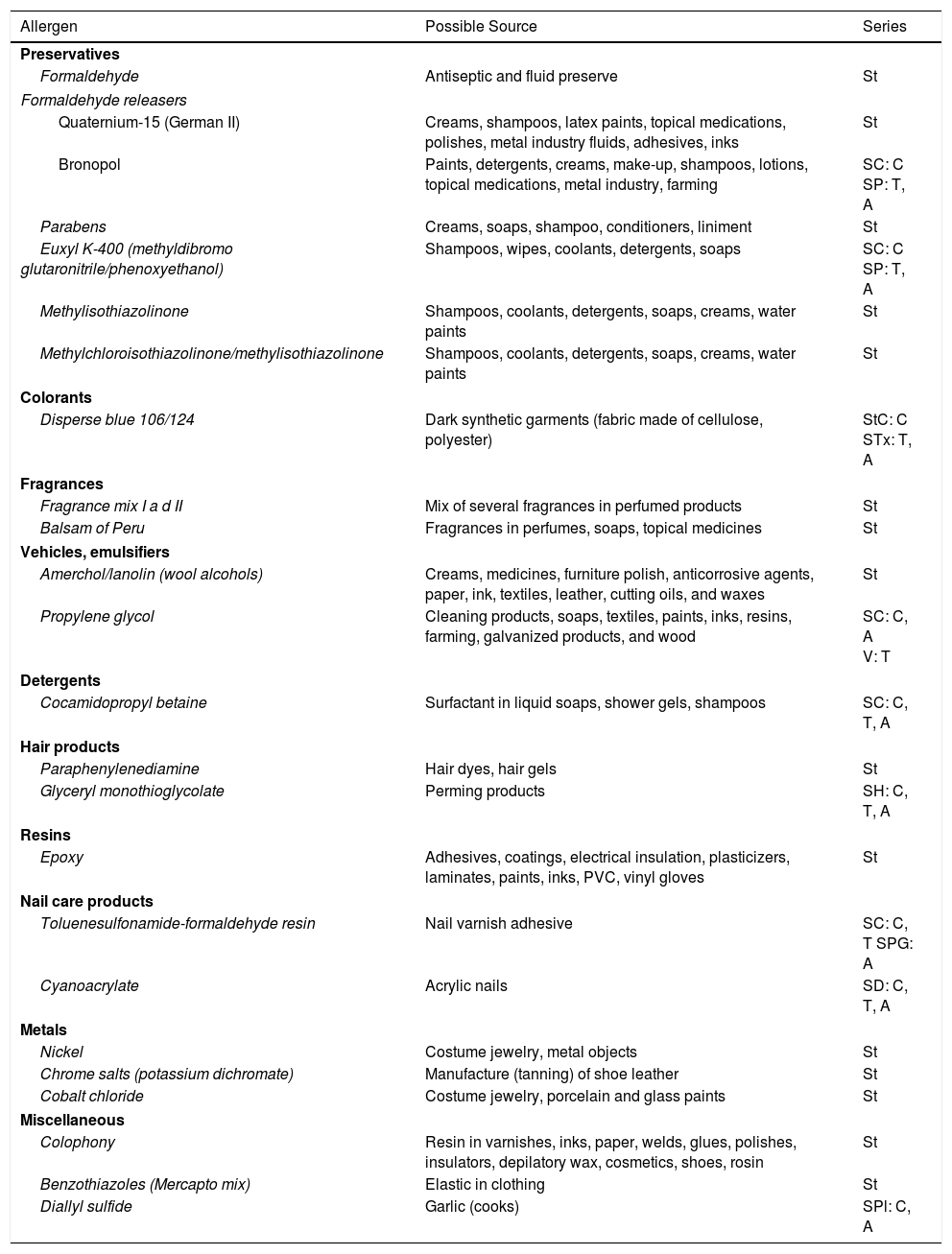
AllergensThe allergens involved vary widely depending on the series studied.43,46–49Table 4 summarizes the main ones. ACD, as is the case with ICD, is mainly associated with occupational and recreational activities in which the patient uses his/her hands. In addition, ICD is often complicated by ACD and vice versa. The professions that entail the greatest risk of ACD include food handlers, hairdressers, construction workers, and cleaning staff.46 The most commonly reported allergens are diallyl disulfide in patients who handle garlic,15,42 paraphenylenediamine in hairdressers,50,51 nickel in the case of people who handle coins,50,51 chrome in construction workers,51 cobalt in electronics workers, and specific preservatives (eg, quaternium-15 and formaldehyde) in the case of health care professionals and persons who work with textiles and wood.51,52 In some cases, the protective measures used to avoid contact with the substances involved (eg, gloves or protective creams) or treatment with corticosteroids may be the cause of ACD.48,53–56
Most Common Allergens in Contact Dermatitis Affecting the Hands.
| Allergen | Possible Source | Series |
|---|---|---|
| Preservatives | ||
| Formaldehyde | Antiseptic and fluid preserve | St |
| Formaldehyde releasers | ||
| Quaternium-15 (German II) | Creams, shampoos, latex paints, topical medications, polishes, metal industry fluids, adhesives, inks | St |
| Bronopol | Paints, detergents, creams, make-up, shampoos, lotions, topical medications, metal industry, farming | SC: C SP: T, A |
| Parabens | Creams, soaps, shampoo, conditioners, liniment | St |
| Euxyl K-400 (methyldibromo glutaronitrile/phenoxyethanol) | Shampoos, wipes, coolants, detergents, soaps | SC: C SP: T, A |
| Methylisothiazolinone | Shampoos, coolants, detergents, soaps, creams, water paints | St |
| Methylchloroisothiazolinone/methylisothiazolinone | Shampoos, coolants, detergents, soaps, creams, water paints | St |
| Colorants | ||
| Disperse blue 106/124 | Dark synthetic garments (fabric made of cellulose, polyester) | StC: C STx: T, A |
| Fragrances | ||
| Fragrance mix I a d II | Mix of several fragrances in perfumed products | St |
| Balsam of Peru | Fragrances in perfumes, soaps, topical medicines | St |
| Vehicles, emulsifiers | ||
| Amerchol/lanolin (wool alcohols) | Creams, medicines, furniture polish, anticorrosive agents, paper, ink, textiles, leather, cutting oils, and waxes | St |
| Propylene glycol | Cleaning products, soaps, textiles, paints, inks, resins, farming, galvanized products, and wood | SC: C, A V: T |
| Detergents | ||
| Cocamidopropyl betaine | Surfactant in liquid soaps, shower gels, shampoos | SC: C, T, A |
| Hair products | ||
| Paraphenylenediamine | Hair dyes, hair gels | St |
| Glyceryl monothioglycolate | Perming products | SH: C, T, A |
| Resins | ||
| Epoxy | Adhesives, coatings, electrical insulation, plasticizers, laminates, paints, inks, PVC, vinyl gloves | St |
| Nail care products | ||
| Toluenesulfonamide-formaldehyde resin | Nail varnish adhesive | SC: C, T SPG: A |
| Cyanoacrylate | Acrylic nails | SD: C, T, A |
| Metals | ||
| Nickel | Costume jewelry, metal objects | St |
| Chrome salts (potassium dichromate) | Manufacture (tanning) of shoe leather | St |
| Cobalt chloride | Costume jewelry, porcelain and glass paints | St |
| Miscellaneous | ||
| Colophony | Resin in varnishes, inks, paper, welds, glues, polishes, insulators, depilatory wax, cosmetics, shoes, rosin | St |
| Benzothiazoles (Mercapto mix) | Elastic in clothing | St |
| Diallyl sulfide | Garlic (cooks) | SPl: C, A |
Abbreviations: A, allergEAZE; C, Chemotechnique; SC, supplementary cosmetic series; SD, supplementary dental series; SH, supplementary hairdressing series; SP, supplementary preservative series; SPG, supplementary plastic and glue series; SPl, supplementary plants series; St, standard series of the Spanish Contact Dermatitis and Skin Allergy Research Group (GEIDAC); StC, Chemotechnique standard series; STx, supplementary textile series; T, Trolab; V, supplementary vehicle series.
Although the trunk is relatively protected from contact with many allergens, ACD at this site remains a diagnosis worthy of consideration. The wide clinical variability and considerable number of differential diagnoses, including multiple eczematous and noneczematous processes, such as toxicoderma, atopic dermatitis, seborrheic dermatitis, pityriasis versicolor, and viral diseases, oblige us to maintain a high degree of suspicion in order to confirm the diagnosis. We review the main patterns that should guide the clinician toward ACD at this site.
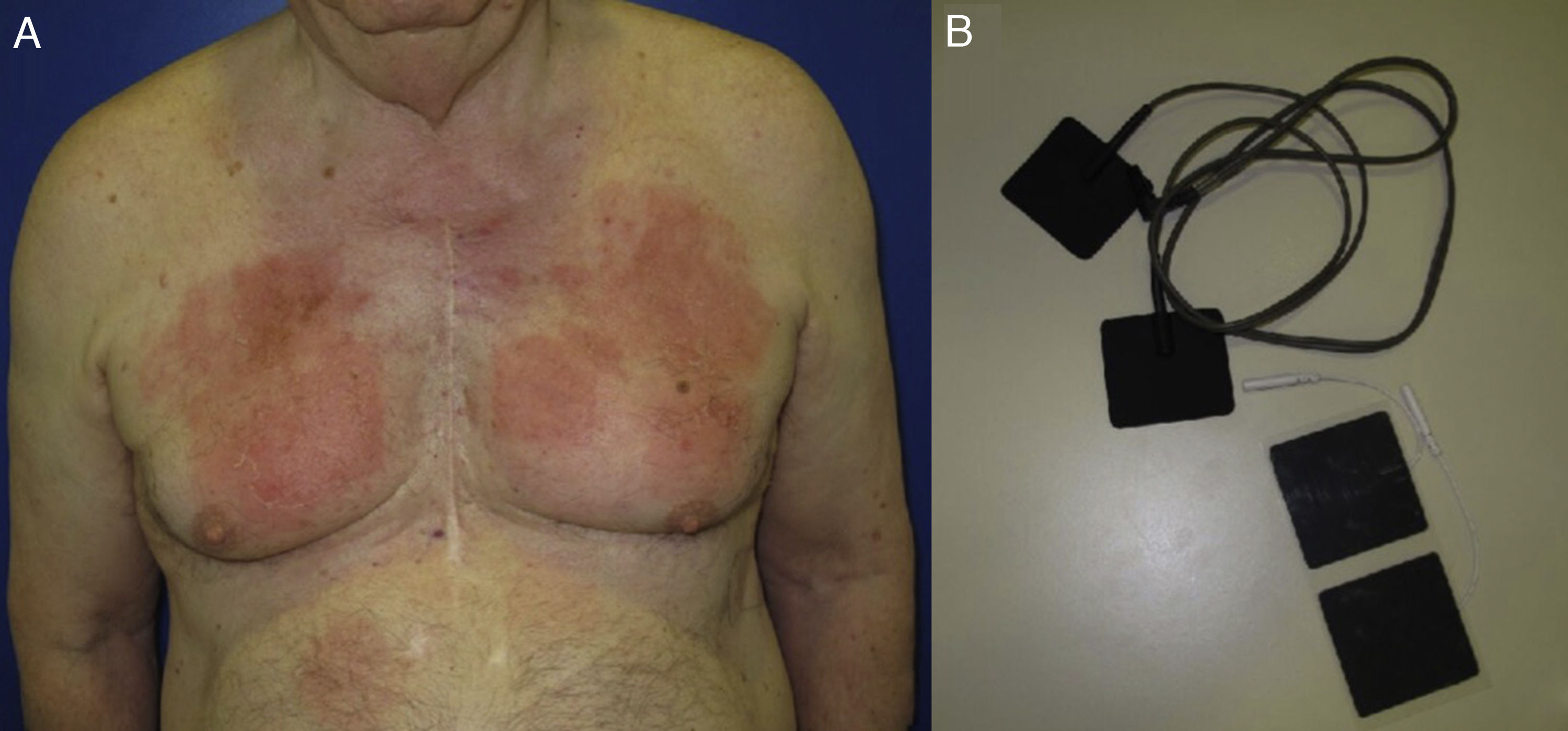
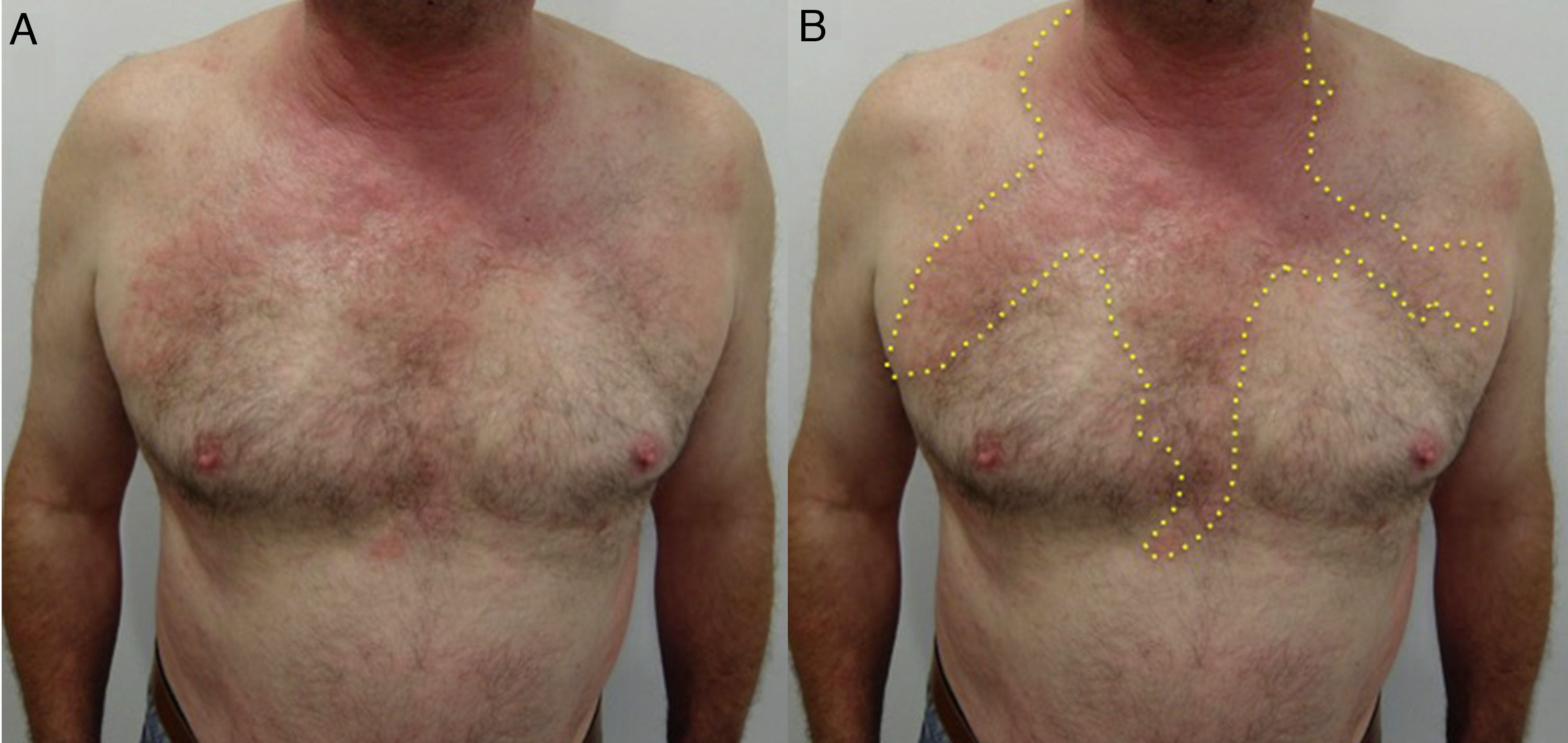
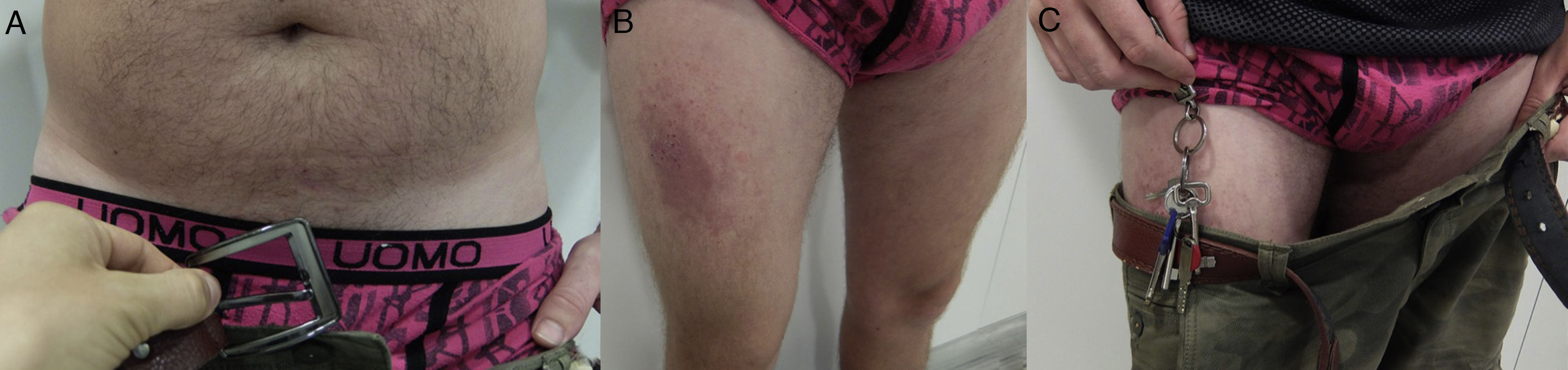
Patterns (Fig. 18)Geographic patternEczematous plaques confined to the area of contact with the allergen. Typical of objects57 (Fig. 18A and Fig. 19).
Eczematous plaques that follow a linear morphology, indicating that a liquid has run down the affected area. Typical of antiseptics and soaps (Fig. 18B and Fig. 20).
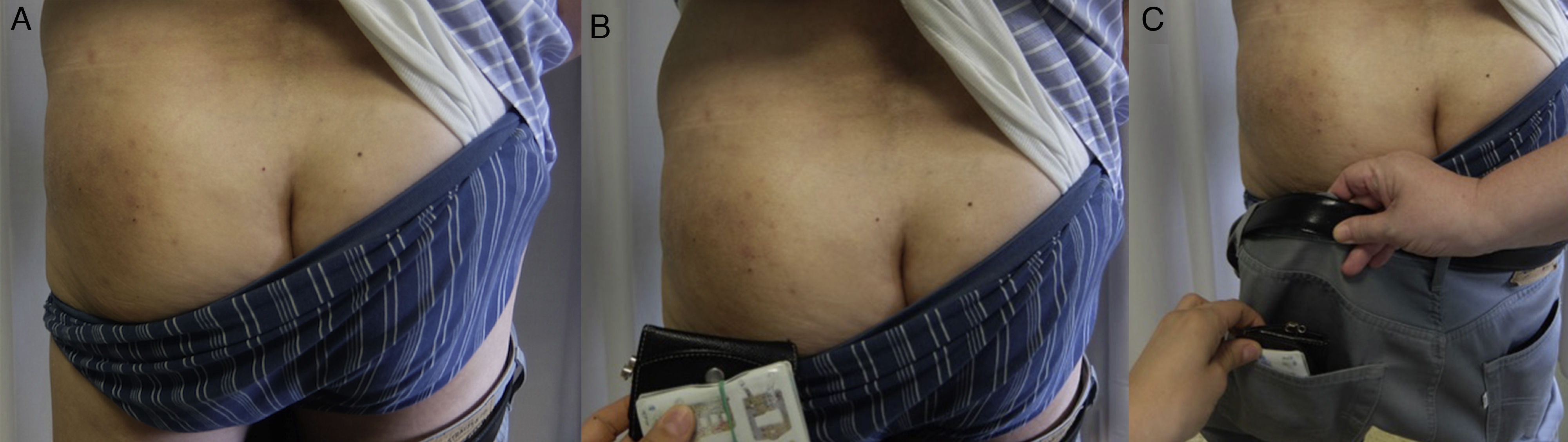
Pocket patternEczematous plaques at sites where there is contact with the pockets, such as the anterior surface of the thighs and the buttocks (Fig. 18C and Fig. 21).
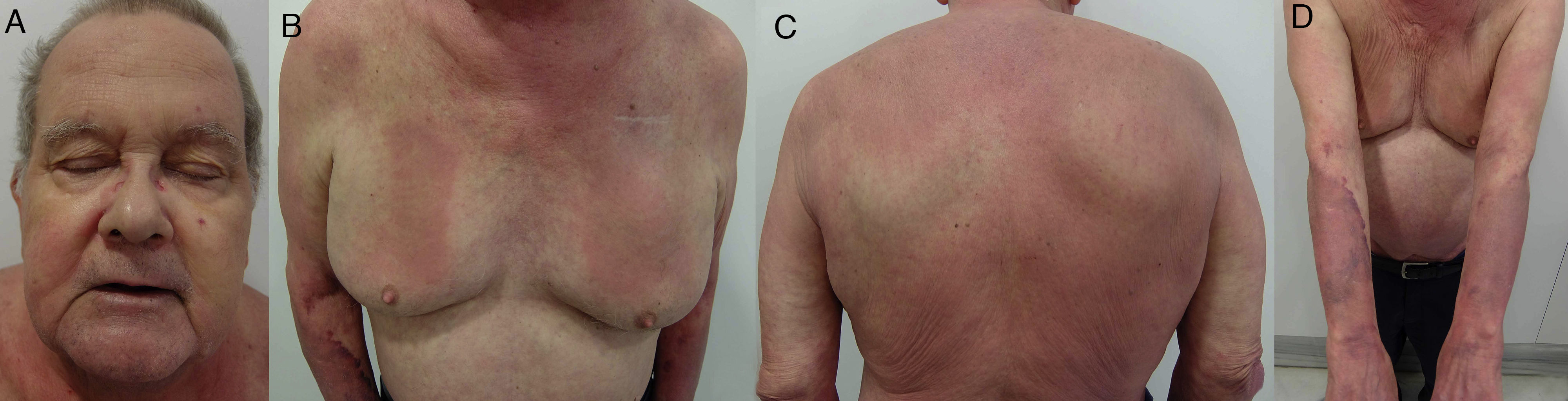
Nickel patternEczematous plaques on parts of the body that are in contact with metals. The most frequent areas are the earlobes, neck, wrists, and the area below the umbilicus. Less commonly involved sites include the intermammary area (midline), owing to contact with the metal underwire of the bra, and the back (midline), owing to contact with the clasp of the bra (Fig. 18D and Fig. 22).
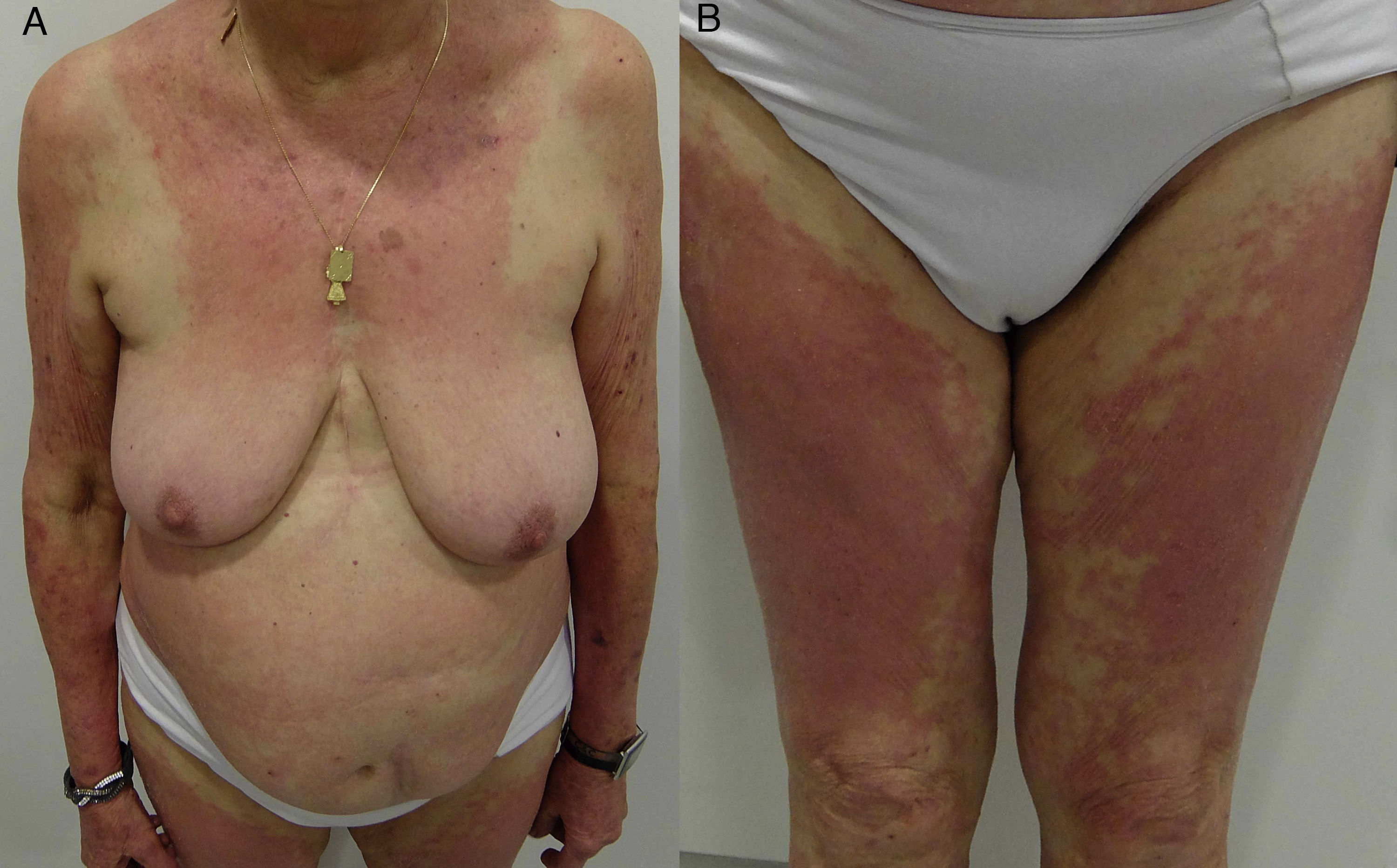
Textile patternEczematous plaque affecting areas of the body where clothing rubs against the skin or where sweat is more abundant. The most frequently involved areas are the neck, axillae, and the internal surface of the arms and thighs. The antecubital and popliteal fossae are typical but infrequent sites. The palms, soles, elbows, and eyelids are rarely affected.
In women, involvement of the trunk can point to a diagnosis, although the area of contact between the skin and bra is spared58 (Fig. 18E and Fig. 23).
Generalized patchy patternEczematous plaques affecting ≥3 areas of the body in a patchy and diffuse distribution, for example, the arms, trunk, and extremities59 (Fig. 18F and Fig. 24).
AllergensThe list of allergens that can affect the trunk is extensive and varied, and an exhaustive clinical history is required before a potential culprit can be identified. The geometric, pocket, and nickel patterns are the easiest to identify and do not usually hamper diagnosis. The drip pattern is mainly associated with preservatives and fragrances in soaps and disinfectants, the main allergen being Kathon CG. The main allergens in the textile pattern are dyes, which have overtaken formaldehyde-releasing finishing products, the predominant allergen in the 1960s.60–62 Dyes are classified into 2 main groups: disperse dyes used in synthetic fabrics, and reactive dyes used in natural or mixed fibers. Disperse dyes bind more weakly to fabric than reactive dyes, with the result that they are released more easily and produce sensitization more often under specific conditions such as sweating, moisture, or repeated rubbing. Despite differences between the populations studied, the most commonly reported allergens are Disperse Blue 106, Disperse Blue 124, and Disperse Orange 3.60–62
In the generalized patchy pattern, the most common allergens are preservatives present in topical products, mainly imidazolidinyl urea, DMDM hydantoin, propylene glycol, and diazolidinyl urea.59Table 5 summarizes the most common allergens.
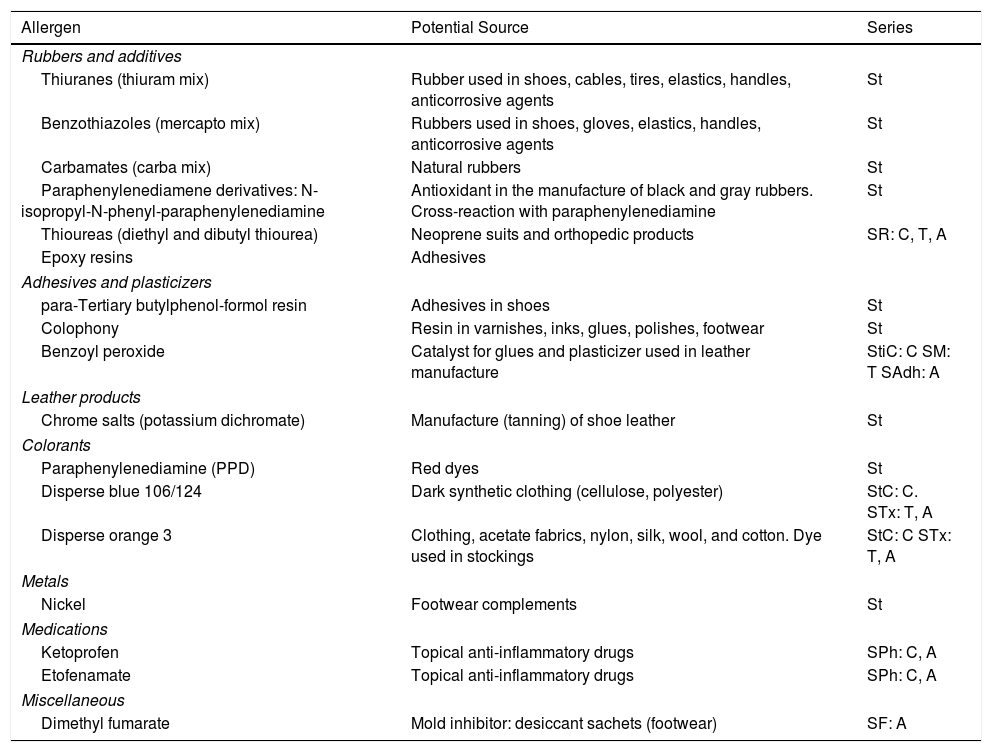
Most Common Allergens in Contact Dermatitis Affecting the Trunk.
| Allergen | Potential Source | Series |
|---|---|---|
| Preservatives | ||
| Formaldehyde | Antiseptic solutions and preservatives | St |
| Formaldehyde releasers | ||
| Quaternium-15 (German II) | Creams, shampoos, latex paints, topical medicines, polishes, metal industry liquids, adhesives, inks | St |
| Imidazolidinyl urea (Germal 115) | Creams, lotions, hair conditioners, shampoos, deodorants, and topical medications | St |
| Diazolidinyl urea | Creams, lotions, shampoos, and hair gels | St |
| DMDM hydantoin | Shampoo, conditioners, make-up, and make-up remover | SC: C, A |
| SP: T | ||
| Bronopol | Paints, detergents, creams, make-up, shampoos, lotions, topical medications, metal industry, farming | SC: C SP: T, A |
| Parabens | Creams, soaps, shampoo, conditioners, liniment | St |
| Euxyl K-400 (methyldibromo glutaronitrile/phenoxyethanol) | Shampoos, wipes, coolants, detergents, soaps | SC: C SP: T, A |
| Methylisothiazolinone | Shampoos, coolants, detergents, soaps, creams, water paints | St |
| Methylchloroisothiazolinone/methylisothiazolinone | Shampoos, coolants, detergents, soaps, creams, water paints | St |
| Colorants | ||
| Disperse blue 106/124 | Dark-colored synthetic garments (cellulose, polyester fabric) | StC: C. STx: T, A |
| Disperse orange 3 | Clothing, fabrics (acetate, nylon, silk, wool, and cotton). Dye in stockings | StC: C STx: T, A |
| Fragrances | ||
| Fragrance mix I and II | Mix of several fragrances in perfumed products | St |
| Balsam of Peru | Fragrances perfumes, soaps, topical medications | St |
| Vehicles, emulsifiers: | ||
| Amerchol/lanolin (wool alcohols) | Creams, medications, furniture polish, anticorrosion agents, paper, ink, textiles, leather, cutting oil, waxes | St |
| Propylene glycol | Cleaning products, soaps, textiles, paints, inks, resins, farming, galvanized products, and wood | SC: C, A V: T |
| Detergents | ||
| Cocamidopropyl betaine | Surfactant in liquid soaps, bath gels, shampoos | SC: C, T, A |
| Metals | ||
| Nickel | Costume jewelry, metal objects | St |
| Miscellaneous | ||
| Colophony | Resin in varnishes, inks, welds, glues polishes, insulators, depilatory wax, cosmetics, footwear, rosin | St |
| Dimethyl fumarate | Mold growth inhibitor in desiccant sachets (Chinese sofas) | SF: A |
| Rubbers | ||
| Thiuranes (thiuram mix) | Clothing elastic | St |
| Benzothiazoles (mercapto mix) | Clothing elastic | St |
| Carbamates (carba mix) | Clothing elastic | St |
| Thioureas (diethyl and dibutyl thiourea) | Neoprene suits | SR: C, T, A |
Abbreviations: A, allergEAZE; C, Chemotechnique; SC, supplementary cosmetic series; SF, supplementary footwear series; SP, supplementary preservative series; SR, supplementary rubber series; St, standard series of the Spanish Contact Dermatitis and Skin Allergy Research Group (GEIDAC); StC, standard Chemotechnique series; STx, supplementary textile series; T, Trolab; V, supplementary vehicle series.
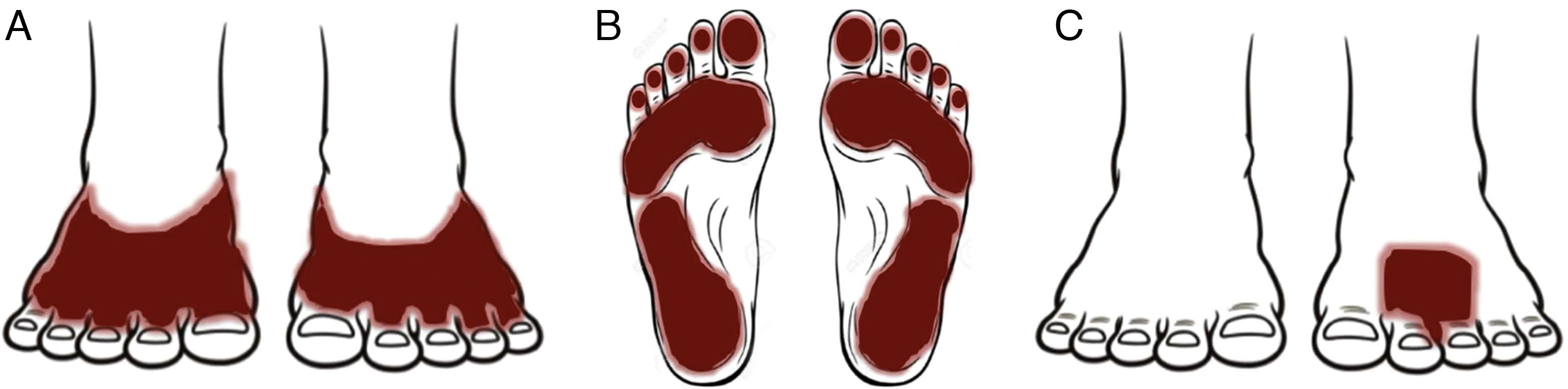
The prevalence of ACD affecting the feet is very variable and has been estimated at 1.5% to 24.2% of all patients undergoing patch tests.63,64 However, these percentages may be even higher, since there is no appropriate legislation that requires potential allergens and their concentrations to be specified. The prolonged exposure to allergens and the frequent occlusion and moisture to which the feet are subject favor development of ACD. It is also important to remember that, as with ACD of the hands, the differential diagnosis should be made with processes characterized by similar symptoms and histopathology (eg, dyshidrotic eczema, psoriasis, ICD, tinea).
Patterns (Fig. 25)Shoe patternEczematous plaques mainly affecting the dorsum of the feet that take the form of the footwear involved. The shoe pattern does not usually affect the interdigital spaces. The pattern points to the allergens present in the shoe (Fig. 25A and Fig. 26).
Eczematous plaques affecting the soles but sparing the arches and interdigital skin. The skin on the dorsum of the food under the tongue of the shoe may also be affected. The pattern is typical of allergens present in black rubber or adhesives (Fig. 25B and Fig. 27).
Localized patternEczematous plaques that are confined to the area of application of the product. Typical of topical medications (Fig. 25C and Fig. 28).
AllergensThe major allergens are found mainly in footwear, followed by topical medications that are applied on the feet, such as antibiotics, antifungals, and corticosteroids.63–69
In the case of ACD caused by footwear, the most common allergens are the products used in the manufacture of rubber (especially black rubber), leather, and adhesives.63–70
Derivatives of paraphenylenediamine, mercaptobenzothiazole, and thiurams are the allergens most frequently associated with the use of rubber.70 Mercaptobenzothiazole may affect the hands and feet. The hands are affected by occupational ACD caused by the mercaptobenzothiazole present in anticorrosion liquids and, to a lesser extent, by rubber gloves. ACD on the feet is caused by work boots or sports shoes.70
Potassium dichromate is the allergen most frequently associated with leather shoes. Para-tertiary-butylphenol-formaldehyde resin71 and colophony are the allergens most frequently associated with adhesives.67,69,70
As for medications, the allergen is usually the active ingredient in antibiotics (more frequently neomycin); ACD to antifungals and corticosteroids is more frequently caused by the vehicle.60–67 There have also been occasional reports of photoallergy to topical anti-inflammatory drugs, with ketoprofen and etofenamate being the most common allergens.72,73 In these cases, symptoms are usually very acute, and tense blisters are a frequent finding (Fig. 29).
Lastly, special attention should be given to a recently reported allergen, dimethyl fumarate. Dimethyl fumarate is used as a mold inhibitor during the storage and transport of various products, including shoes. Dimethyl fumarate–induced ACD was first associated with contact with furniture from China; however, in Spain, most cases were associated with shoes packaged with desiccant sachets containing dimethyl fumarate. The symptoms almost only affect women, and the most common pattern is the shoe pattern, although the clinical picture is usually very acute with marked edema, vesicles, and blisters.66Table 6 summarizes the main allergens.
Most Common Allergens in Contact Dermatitis Affecting the Feet.
| Allergen | Potential Source | Series |
|---|---|---|
| Rubbers and additives | ||
| Thiuranes (thiuram mix) | Rubber used in shoes, cables, tires, elastics, handles, anticorrosive agents | St |
| Benzothiazoles (mercapto mix) | Rubbers used in shoes, gloves, elastics, handles, anticorrosive agents | St |
| Carbamates (carba mix) | Natural rubbers | St |
| Paraphenylenediamene derivatives: N-isopropyl-N-phenyl-paraphenylenediamine | Antioxidant in the manufacture of black and gray rubbers. Cross-reaction with paraphenylenediamine | St |
| Thioureas (diethyl and dibutyl thiourea) | Neoprene suits and orthopedic products | SR: C, T, A |
| Epoxy resins | Adhesives | |
| Adhesives and plasticizers | ||
| para-Tertiary butylphenol-formol resin | Adhesives in shoes | St |
| Colophony | Resin in varnishes, inks, glues, polishes, footwear | St |
| Benzoyl peroxide | Catalyst for glues and plasticizer used in leather manufacture | StiC: C SM: T SAdh: A |
| Leather products | ||
| Chrome salts (potassium dichromate) | Manufacture (tanning) of shoe leather | St |
| Colorants | ||
| Paraphenylenediamine (PPD) | Red dyes | St |
| Disperse blue 106/124 | Dark synthetic clothing (cellulose, polyester) | StC: C. STx: T, A |
| Disperse orange 3 | Clothing, acetate fabrics, nylon, silk, wool, and cotton. Dye used in stockings | StC: C STx: T, A |
| Metals | ||
| Nickel | Footwear complements | St |
| Medications | ||
| Ketoprofen | Topical anti-inflammatory drugs | SPh: C, A |
| Etofenamate | Topical anti-inflammatory drugs | SPh: C, A |
| Miscellaneous | ||
| Dimethyl fumarate | Mold inhibitor: desiccant sachets (footwear) | SF: A |
Abbreviations: A, allergEAZE; C, Chemotechnique; SAdh, supplementary adhesive series; SF, supplementary footwear series; SM, supplementary medication series; SPh, supplementary photoallergen series; SR, supplementary rubber series; St, standard series of the Spanish Contact Dermatitis and Skin Allergy Research Group (GEIDAC); StC, standard Chemotechnique series; StiC, standard Chemotechnique international series; STx, supplementary textile series; T, Trolab.
The authors declare that they have no conflicts of interest.
Please cite this article as: Rozas-Muñoz E, Gamé D, Serra-Baldrich E. Dermatitis de contacto alérgica por regiones anatómicas. Claves diagnósticas. Actas Dermosifiliogr. 2018;109:485–507.