In recent years the concept of psoriasis as a systemic disease has gained acceptance due to its association with numerous comorbid conditions, particularly atherosclerosis and cardiovascular disease. Several studies have shown that patients with psoriasis, especially younger patients and those with more severe forms of psoriasis or with psoriatic arthritis, have a higher prevalence of risk factors and metabolic syndrome, as well as an increased risk of major cardiovascular events such as myocardial infarction, cerebrovascular disease, and peripheral arterial disease. Furthermore, it remains unclear which of the current treatments might be more effective in reducing cardiovascular risk in these patients. It is therefore important for dermatologists to be aware of this increased risk, to be able to detect modifiable risk factors early and, when appropriate, refer patients to other specialists for the prevention of major cardiovascular events.
En los últimos años el concepto de psoriasis como enfermedad sistémica se ha ido extendiendo debido a su asociación con múltiples comorbilidades, entre las que destaca la arterioesclerosis y la enfermedad cardiovascular. En diferentes estudios a lo largo de los años se ha demostrado que en los pacientes con psoriasis, sobre todo en aquellos más jóvenes, con formas más graves y/o artritis psoriásica, existe una mayor prevalencia de factores de riesgo y síndrome metabólico, así como un mayor riesgo de presentar eventos cardiovasculares mayores, como el infarto de miocardio, la enfermedad cerebrovascular y la arteriopatía periférica. Además, aún no queda claro cuáles de los tratamientos actuales podrían ser más beneficiosos en cuanto a reducción del riesgo cardiovascular en estos pacientes. Por eso, es importante la difusión entre dermatólogos de este riesgo aumentado, con el fin de diagnosticar precozmente aquellos factores de riesgo modificables, y derivar al paciente a otros especialistas en el momento oportuno para prevenir el desarrollo de eventos cardiovasculares mayores.
Psoriasis is a chronic systemic inflammatory disease that can be associated with multiple comorbidities, of which cardiovascular (CV) disease due to atherosclerosis is one of the most significant.1 Advances in our understanding of the association between psoriasis and CV disease could facilitate early diagnosis and treatment. Assessment of the risk factors for potential comorbid conditions and of the signs and symptoms of such diseases is an important aspect of the care of patients with psoriasis. This article reviews the current evidence on the association between moderate to severe psoriasis and CV disease, the impact of systemic treatments for psoriasis on this association, and recommendations for the clinical monitoring and referral of these patients.
Association Between Psoriasis and Cardiovascular DiseaseModerate to severe psoriasis is associated with a increased risk of developing CV disease, including coronary heart disease, cerebrovascular disease, and peripheral artery disease. Observational studies have detected an elevated risk of myocardial infarction in patients with psoriasis.2–6In a prospective cohort of over 130 000 adults with psoriasis, the incidence of myocardial infarction (adjusted for CV risk factors) per 1000 person-years was 3.58 (95% CI, 3.52-3.65) for the control group, 4.04 (95% CI, 3.88-4.21) for patients with moderate psoriasis, and 5.13 (95% CI, 4.22-6.17) for patients with severe psoriasis (defined as those requiring systemic therapy). The impact on risk was greater in younger patients (relative risk [RR], 3.10 with a 95% CI, 1.98-4.86 in patients under 60 years versus RR, 1.36 with a 95% CI, 1.13-1.64 in patients older than 60 years).3
Other forms of CV disease besides coronary heart disease also occur with greater frequency in patients with psoriasis.5–7 Prodanovich et al. found a significant increase in the prevalence of cerebrovascular disease in patients with psoriasis (OR, 1.70; 95% CI, 1.33-2.17) and peripheral vascular disease (OR 1.98, 95% CI, 1.32-2.82).8 Once again, it is in patients with severe psoriasis that a significant increase in the risk of stroke has been observed (hazard ratio [HR], 1.43; 95% CI, 1.1-1.9) compared to a modest increase in patients with mild forms of the disease (HR, 1.06; 95% CI, 1.01-1.1).9
However, this epidemiological association between psoriasis and CV disease has not been confirmed in all studies.10–12 The inconsistency appears to be due largely to variations in impact relating to the severity of psoriasis.
Current evidence indicates that the association between psoriasis and CV disease is due to the underlying chronic inflammation present in both conditions. Common pathophysiological pathways have been identified, including the involvement of T-helper 1 cells, cytokines (interferon-γ, tumor necrosis factor [TNF] α, and interleukin-2) and vascular endothelial growth factor-mediated angiogenesis.13–18
Association Between Psoriasis and Cardiovascular Risk FactorsObservational studies have found an independent relationship between moderate to severe psoriasis and certain risk factors for CV disease, including diabetes mellitus,19,20 hypertension,21–23 obesity, and dyslipidemia.24 A higher prevalence of smoking has also been observed among patients with psoriasis.25
The available evidence indicates that psoriasis also has an influence on the severity of hypertension and diabetes mellitus. Epidemiological studies show that patients with psoriasis and diabetes mellitus more often receive pharmacological treatment and have a higher risk of microvascular and macrovascular complications.26,27 In population-based studies, a relationship has also been observed between the severity of psoriasis and uncontrolled hypertension.20
Furthermore, multiple epidemiological studies support the association between psoriasis and metabolic syndrome or some of its components, such as abdominal obesity, hypertriglyceridemia, and low levels of high-density lipoprotein.28–30
However, the origin of the association between psoriasis and CV risk factors and atherosclerotic disease is, as yet, poorly understood. Since, our knowledge of the association is based on epidemiological studies, it is unclear whether psoriasis is the pathogenic factor that favors the onset of the other conditions (because of the inflammation it causes in the body) or whether what we are seeing is a set of comorbid conditions with no shared pathogenic basis.
Clinical Implications of Cardiovascular Disease in PsoriasisThe association between psoriasis and CV disease has important prognostic implications. Patients with psoriasis appear to have a worse prognosis following a first-time myocardial infarction3,31 as well as an increased risk of CV mortality.32 In a meta-analysis, CV mortality was significantly higher in patients with severe psoriasis than in the general population (RR, 1.37; 95% CI, 1.17-1.60).6 Similarly, a cohort of 3603 patients with severe psoriasis was observed to have a higher risk of dying from a cardiac or cerebrovascular disease (HR, 1.57; 95% CI, 1.26-1.96) compared to a control group.33
Impact on Cardiovascular Disease of Drugs Used to Treat PsoriasisSince psoriasis is associated with a risk of CV disease, probably as a result of systemic inflammation, the therapies used to treat psoriasis, which are designed to reduce inflammation, could theoretically reduce CV risk. However, the evidence for this hypothesis, derived mainly from observational studies, is scant and inconsistent.34 Abuabara et al. studied a cohort of 25 554 patients that included a group receiving systemic immunomodulatory therapy (methotrexate, ciclosporin, alefacept, efalizumab, adalimumab, etanercept, or infliximab) and a control group treated with phototherapy.35They found no differences in risk of myocardial infarction between the 2 groups.
Other authors have also failed to confirm the beneficial effect of systemic treatment in general; however, there is evidence indicating that certain therapies may have a potentially beneficial effect.36
MethotrexateA hypothesis has been advanced that the anti-inflammatory properties of methotrexate (MTX) could reduce CV risk in patients with chronic inflammatory diseases through the modulation of nucleotide metabolism and the inhibition of cytokine signaling.37,38 This hypothesis has led to the design of clinical trials (currently under way) to assess the use of low-dose treatment with MTX in myocardial infarction with ST-segment elevation (the TETHYS trial) and in patients with chronic coronary artery disease and persistent elevations in C-reactive protein (the CIRT trial).39,40 The results of these and other studies will improve our understanding of the association between inflammation and CV disease and the role of MTX.
Several epidemiological studies have observed a possible beneficial effect of treatment with MTX on CV risk in patients with underlying autoimmune diseases. The authors of a retrospective cohort study of patients with psoriasis found treatment with MTX to be associated with a lower risk of CV and cerebrovascular disease and arteriosclerosis.41 Similarly, the authors of a retrospective study of 2400 patients with severe psoriasis reported a lower risk for CV disease events in patients treated with biologic agents or MTX compared to patients on other treatments.42However, in another retrospective study, no differences were found in the hospitalization rate for ischemic heart disease between patients with psoriasis receiving MTX and those being treated with other nonbiologic antipsoriatic drugs.43A meta-analysis investigating the relationship between MTX use and risk of CV disease in patients with rheumatoid arthritis or psoriasis (mainly the former) found a reduction in the risk of CV events and myocardial infarction of 21% and 18%, respectively in patients on methotrexate.38
CiclosporinTreatment with ciclosporin is associated with a dose-dependent increase in blood pressure, serum triglycerides, and total cholesterol levels.44,45 Ciclosporin has been shown to generate reactive oxygen species, to cause cellular death in the myocardium, and to inhibit the migration of endothelial cells and angiogenesis induced by vascular endothelia growth factor (VEGF).46 In spite of these effects, there is evidence that ciclosporin use may help to protect the heart against reperfusion injury after myocardial infarction.47 It has also been associated with a possible reduction in infarct size in animal models.48 However, in a placebo-controlled randomized clinical trial in which ciclosporin was administered before primary angioplasty in patients with myocardial infarction, no differences were found with respect to the primary outcome (mortality, readmission due to heart failure or adverse remodeling at 1 year).49
With respect to the possible influence of ciclosporin treatment on CV risk in patients with psoriasis, a prospective analysis of CV events in an observational cohort of 6902 patients with severe psoriasis and a maximum follow-up of 5 years, ciclosporin use was not found to be associated with any protective effect (HR, 1.06; 95% CI, 0.26-4.27), in contrast with the reduced risk of such events seen in patients treated with MTX.42
RetinoidsRetinoids increase triglyceride and total cholesterol levels (particularly low-density lipoproteins) but they have not been shown to increase CV risk.50 The triglyceride and cholesterol elevations appears to be dose-dependent, but they can be controlled with diet and changes in dose. As in the case of ciclosporin, treatment with retinoids was not associated with any reduction in the number of CV events in the follow-up of the Danish cohort of 6902 patients with severe psoriasis.42
Tumor Necrosis Factor InhibitorsThe association between TNF antagonist therapy and CV disease has been studied in a number of different settings:
Cardiovascular risk factorsTNF antagonist therapy appears to have metabolic effects that could improve the patient's CV risk profile. Etanercept, infliximab, and adalimumab have been associated with an improvement in insulin resistance in patients with inflammatory diseases, including psoriasis, and with a decrease in fasting blood sugar and a lower risk of developing diabetes mellitus.51–54The effect on the lipid profile is more nebulous and these drugs do not appear to significantly modify serum levels, although there may be an antiatherogenic effect (which in the long term is clearer with etanercept than with infliximab).55–58
Biomarkers, such as C-reactive protein, adiponectin and resistin are considered to be markers of both inflammation and CV risk.59,60While initial findings suggest a possible beneficial effect on levels of adiponectin and other markers, the evidence is controversial and does not support firm conclusions.61 Treatment with TNF inhibitors in patients with psoriatic joint disease has been shown to reduce carotid artery intima-media thickness and arterial rigidity, both predictors of CV disease.62–64
Ischemic heart diseaseThe authors of a retrospective study of 8845 patients with psoriasis or psoriatic arthritis report a reduction in the risk of myocardial infarction in the patients on TNF antagonist therapy compared to those receiving topical therapies (HR, 0.50, 0.32-0.79).65Further evidence of the potential beneficial effect of TNF blockers on CV risk can be extrapolated from studies in patients with rheumatoid arthritis, which have shown reduced rates of CV events in patients on TNF antagonist therapy.66,67
Heart failureTNF-α levels are elevated in patients with heart failure. These elevations may contribute to cardiac dysfunction, deterioration of peripheral perfusion, and cachexia and have a negative impact on prognosis.68–70 This finding led to the suggestion that treatment with TNF inhibitors could be a possible therapeutic strategy in patients with heart failure.71,72 Initial clinical trials showed a good safety profile and suggested a clinical benefit in terms of quality of life, ventricular remodeling, and endothelial function.73–75 However, subsequent randomized clinical trials with etanercept (RENAISSANCE, RECOVER, and RENEWAL) and infliximab (ATTACH) in the treatment of heart failure were stopped early because of lack of efficacy.76–78 In the case of infliximab, all-cause mortality was increased in the high-dose arm of the trial (10 mg/kg).78
In view of the results of these trials, TNF inhibitors went from being a possible therapeutic strategy to being a cause for concern in heart failure. In 2002, the Food and Drug Administration (FDA) published a series of 47 cases of heart failure (38 of which were new-onset) associated with treatment with infliximab or etanercept. These cases had been reported on the FDA MedWatch program. After TNF antagonist therapy was discontinued and heart failure therapy was started, most of these patients presented considerable improvement or complete resolution.79 In a study of etanercept in patients with psoriasis, heart failure was rare and no increased risk was demonstrated.80
In a recent meta-analysis, no significant differences were found between patients treated with biologic drugs and controls in the prevalence of heart failure.81 In safety analyses of adalimumab in patients with rheumatoid arthritis both in clinical trials and postmarketing surveillance, the rate for heart failure was very low.82,83
In summary, the data on the risk of heart failure associated with TNF antagonist therapy administered at the doses approved by the FDA are inconclusive.84 However, infliximab is contraindicated at doses higher than 5 mg/kg in patients with moderate to severe heart failure (New York Heart Association [NYHA] III-IV), and it is recommended that etanercept and adalimumab be used with caution in patients who have symptomatic heart failure or a low ejection fraction [EF] (EF < 50%). In patients who develop new-onset heart failure while on treatment with a TNF blocker, cessation of the treatment is recommended.34
UstekinumabA meta-analysis of controlled clinical trials found no significant increase in the risk of major CV events in patients treated with ustekinumab.85 These results are confirmed by the data from the 12 093 patients on the PSOLAR registry, collected to evaluate the risk of adverse events of particular interest in patients with psoriasis treated with ustekinumab and other psoriasis treatments.86 Ustekinumab is not, therefore, contraindicated in patients with heart failure. However, by contrast to what was observed in other studies, a modest increase in CV events in patients treated with MTX or ciclosporin was observed on that registry.86
SecukinumabSecukinumab has been shown to be highly effective in clearing psoriatic lesions, with higher rates of response than 2 of the currently available alternative treatment options in patients with moderate to severe psoriasis following failure to respond to conventional immunosuppressants. The available data does not suggest that secukinumab increases the risk of CV events. However, since there is little long-term data available, additional studies are needed to investigate the CV safety of this drug.87
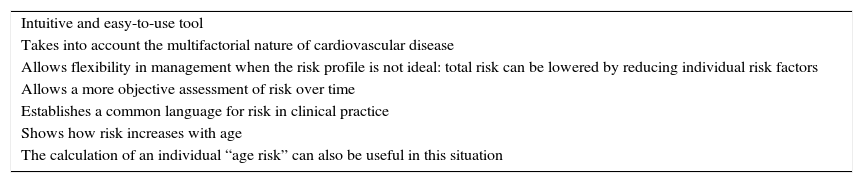
Risk Stratification Concepts and StrategiesCV risk refers to the probability of a person having a CV event within a defined period. It is calculated by assessing the most important risk factors: age, sex, smoking status, blood pressure, and lipid levels. It is essential for clinicians to be able to assess a patient's risk profile quickly and accurately when making decisions about how to manage their condition. In general, screening for risk factors is recommended for men over 40 years of age and in women who are over 50 or postmenopausal.88 The use of risk scales to assess overall risk is recommended. These scales must be validated for the population to which they are applied. Table 1 lists some of the advantages of risk stratification.
Advantages of Using Risk Tables.
| Intuitive and easy-to-use tool |
| Takes into account the multifactorial nature of cardiovascular disease |
| Allows flexibility in management when the risk profile is not ideal: total risk can be lowered by reducing individual risk factors |
| Allows a more objective assessment of risk over time |
| Establishes a common language for risk in clinical practice |
| Shows how risk increases with age |
| The calculation of an individual “age risk” can also be useful in this situation |
In the USA, the Framingham Risk Score is the most widely used risk calculator and the one recommended in the American Heart Association's clinical guidelines.89 This scoring system is based on data from the Framingham epidemiological study, which has been collecting information on succeeding generations since it started in 1948. The recommended model estimates the 10-year risk of heart disease.90 There is an easy-to-use calculator available online (https://www.framinghamheartstudy.org/risk-functions/index.php).
The Framingham model has been adapted for use in the Spanish population using a carefully checked calibration process. The adapted score was subsequently validated and the result is the REGICOR scale and risk calculator.91–93
The SCORE system is the risk scale recommended by the European guidelines on CV disease prevention based on data from the cohorts included in 12 European studies (205 178 patients examined for the first time between 1970 and 1988 with 2.7 million years of follow-up and 7934 deaths from CV disease) and amply validated.88 SCORE estimates the 10-year risk of a first CV event leading to death. Although there is no universal risk threshold, the intensity of advice should increase with increased risk. In general, people with a risk of CV death of 5% or more require intensive counseling and may benefit from pharmacological treatment. At risk levels of 10% or more, patients require pharmacological treatment.
In addition, there are complementary techniques that can be useful in assessing CV risk in individuals with a moderate risk level. At any level of exposure to risk factors, there is a substantial variation in the severity of atherosclerosis, which can probably be attributed to variations in genetic susceptibility, the combination of different risk factors, and the interaction between genetic and environmental factors. Thus, it can be useful to assess subclinical atherosclerosis to obtain a better CV risk prediction. Various non-invasive techniques (such as carotid ultrasound to measure intima-media thickness and the presence and characteristics of plaques, electron beam computed tomography, multislice computed tomography coronary imaging, the ankle-wrist vascular index, and magnetic resonance imaging) have potential for measuring and directly or indirectly monitoring atherosclerosis in asymptomatic individuals. However, the cost-benefit ratio for such techniques has not been determined.
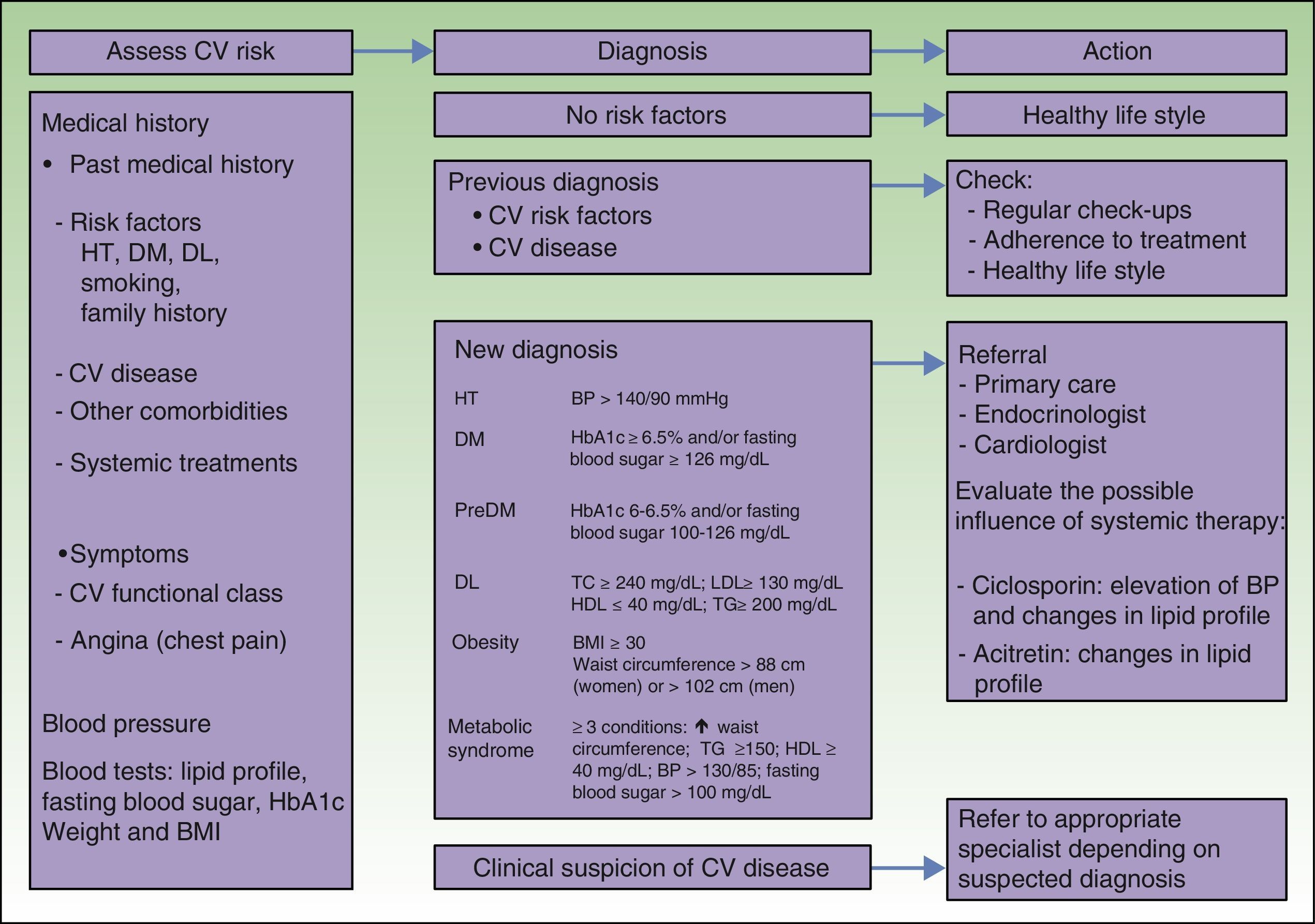
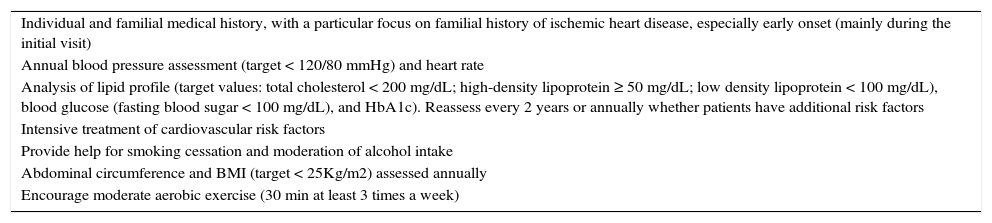
Recommendations on Cardiovascular Follow-Up and Monitoring of Patients With Psoriasis by DermatologistsThe current recommendations for CV follow-up of patients with psoriasis by dermatologists stress the importance of informing patients with moderate to severe psoriasis about their increased risk of CV disease.94–96 CV risk should be assessed during the initial evaluation and subsequent follow-up of patients with psoriasis (Table 2). Patients should also be informed about the need for future multidisciplinary care (cardiologist, internist, endocrinologist, general practitioner) and referral criteria (Fig. 1) to ensure the best overall care in these patients with high CV risk.
General Recommendations for Initial and Follow-up Cardiovascular Risk Assessment in Patients with Psoriasis.
| Individual and familial medical history, with a particular focus on familial history of ischemic heart disease, especially early onset (mainly during the initial visit) |
| Annual blood pressure assessment (target < 120/80 mmHg) and heart rate |
| Analysis of lipid profile (target values: total cholesterol < 200 mg/dL; high-density lipoprotein ≥ 50 mg/dL; low density lipoprotein < 100 mg/dL), blood glucose (fasting blood sugar < 100 mg/dL), and HbA1c). Reassess every 2 years or annually whether patients have additional risk factors |
| Intensive treatment of cardiovascular risk factors |
| Provide help for smoking cessation and moderation of alcohol intake |
| Abdominal circumference and BMI (target < 25Kg/m2) assessed annually |
| Encourage moderate aerobic exercise (30 min at least 3 times a week) |
Screening of patients with psoriasis for cardiovascular risk factors and criteria for specialist referral.
BP: blood pressure; BMI: body mass index; CV: cardiovascular; DL: dyslipidemia; DM: diabetes mellitus; HDL-C: high density lipoprotein cholesterol; HT: hypertension; LDL-C: low density lipoprotein cholesterol; TC: total cholesterol; TG: triglycerides.
The association between psoriasis and CV disease is supported by ample observational evidence, which shows a greater prevalence of CV risk factors, higher incidence of CV disease, and worse prognosis in patients with psoriasis, particularly in the case of young patients with severe forms of the skin disease. This association is probably the result of a chronic underlying inflammatory state; certain proinflammatory cytokines are common to the pathophysiology of both diseases. However, the underlying mechanisms are still poorly understood.
When the available data is analyzed globally, systemic immunomodulatory therapy for psoriasis does not appear to influence the onset or severity of CV disease. However, when the drug therapies are analyzed separately, differences are found. There is currently insufficient evidence to recommend certain psoriasis treatments solely on the basis of their impact on CV risk. However, when considering a systemic treatment clinicians must assess the risk involved and take into account the fact that TNF inhibitors and MTX have been shown to be the treatments that offer the greatest potential benefit in the context of ischemic heart disease and that there is evidence of a possible prejudicial effect in the case of certain TNF inhibitors in patients with ischemic heart disease, systolic dysfunction and a poor functional classification.
The management of psoriasis must include a thorough assessment of CV risk and of possible signs and symptoms of CV disease, both on diagnosis and periodically thereafter, depending on the severity of the disease. This follow-up is essential to ensure the early diagnosis and treatment of CV disease as well as early referral and multidisciplinary treatment when this becomes necessary.94–96Finally, studies are needed to clarify the mechanisms underlying the association between these 2 diseases, the impact of systemic therapies, and the best clinical approach.
- 1.
An association exists between psoriasis and certain CV risk factors: hypertension, diabetes mellitus, and metabolic syndrome.
- 2.
Psoriasis, and particularly severe psoriasis, is itself a CV risk factor, since these patients have an increased risk for CV disease and mortality. Although the differences vary between studies, the increase in risk is around 50%.
- 3.
The mechanism by which psoriasis increases CV risk is unknown. The hypothesis has been considered that it is due to systemic inflammation or to the fact that patients with psoriasis often present several CV risk factors, with psoriasis acting as an attracting factor.
- 4.
There is evidence that—of all the systemic treatments of psoriasis—MTX and TNF inhibitors may have a beneficial effect on CV disease. However, caution should be exercised when prescribing TNF blockers to patients who have heart failure in very advanced functional classes (NYHA III-IV) or severe ventricular dysfunction (EF ≤ 35%).
- 5.
CV risk must be assessed in all patients with psoriasis. Risk assessment will help prevent CV morbidity and mortality and inform the choice of the best treatment for each patient.
The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors state that they have followed the protocols of their hospitals on the publication of patient data.
Right to privacy and informed consentThe authors declare that no private patient data are disclosed in this article.
Conflict Of InterestsAbbvie facilitated the meetings of the workgroup, but none of the company's employees participated in the collection of scientific evidence, group discussions, or writing the article.
Rafael Botella has served as a paid consultant for Pfizer, Abbvie and Galderma and as a speaker for Abbvie, Pfizer, Novartis, Leo Pharma and MSD. He has been an investigator for Novartis, Abbvie, Janssen, Leo Pharma, Cantabria, Biofrontera and Viñas and has been sponsored to attend conferences by Novartis, Pfizer, Abbvie, Janssen, Lilly, Cantabria and MSD.
José Manuel Carrascosa has served as a paid consultant and a speaker for Abbvie, Novartis, Janssen, Amgen, Biogen, Leo, Celgene, Lilly, and Pfizer.
Raquel Rivera has served as a paid consultant for Abbvie, Janssen, Lilly, and Pfizer, and as a speaker for MSD, Abbvie, Janssen, Leo Pharma, Novartis, and Pfizer. She has been an investigator for Abbvie, Pfizer, Janssen, Celgene, Lilly, Novartis, and Leo Pharma and has been sponsored to attend conferences by Abbvie, Janssen, Novartis, Pfizer, Leo Pharma, Celgene, and MSD.
Esteban Daudén has served as a member of the Advisory Board, has been a consultant, has received grants, undertaken research support, participated in clinical trials and been remunerated to as a speaker by the following pharmaceutical companies: Abbvie/Abbott, Amgen, Biogen, Janssen-Cilag, Leo Pharma, MSD, Pfizer, Novartis, Celgene, and Lilly.
Please cite this article as: Bonanad C, González-Parra E, Rivera R, Carrascosa JM, Daudén E, Olveira A, et al. Implicaciones Clínicas, Diagnósticas Y Terapéuticas De La Psoriasis Y Enfermedad Cardiovascular. Actas Dermosifiliogr. 2017;108:800–808.