Paracoccidioidomycosis (PCM) is a deep systemic mycosis caused by Paracoccidioides brasiliensis, a thermally dimorphic fungus that grows as a yeast at 37°C and in mycelial form at 25°C. It is endemic in rural areas of Central and South America. In natural conditions, humans are the only known host. The source of the infection is soil contaminated with the fungus and the most common route of entry is the airway, giving rise to a primary infection in the lungs, which is often asymptomatic, particularly in young patients. From the lungs, infection spreads via the blood and lymph to the skin, mucous membranes, lymph nodes, and other organs.1–4
We report the case of a 50-year-old male agricultural worker from Paraguay (South America) who presented with a 4-month history of lesions in the mouth, on the palmar surface of the third finger of his left hand, and on the plantar surface of his right great toe. These were accompanied by swelling of the lip, pain, weight loss of 10 kg since the onset of the condition, and a feeling of fever, particularly at night. The patient reported no underlying disease or any history of trauma. He had been a smoker for many years.
Physical examination revealed a swollen lower lip with marked infiltration and induration as well as multiple eroded, mulberry-like, erythematous papules giving the lesion a cobblestone appearance (Fig. 1). The lesions on the fingers and toes were small ulcers with well-defined borders and clean bases (Fig. 2).
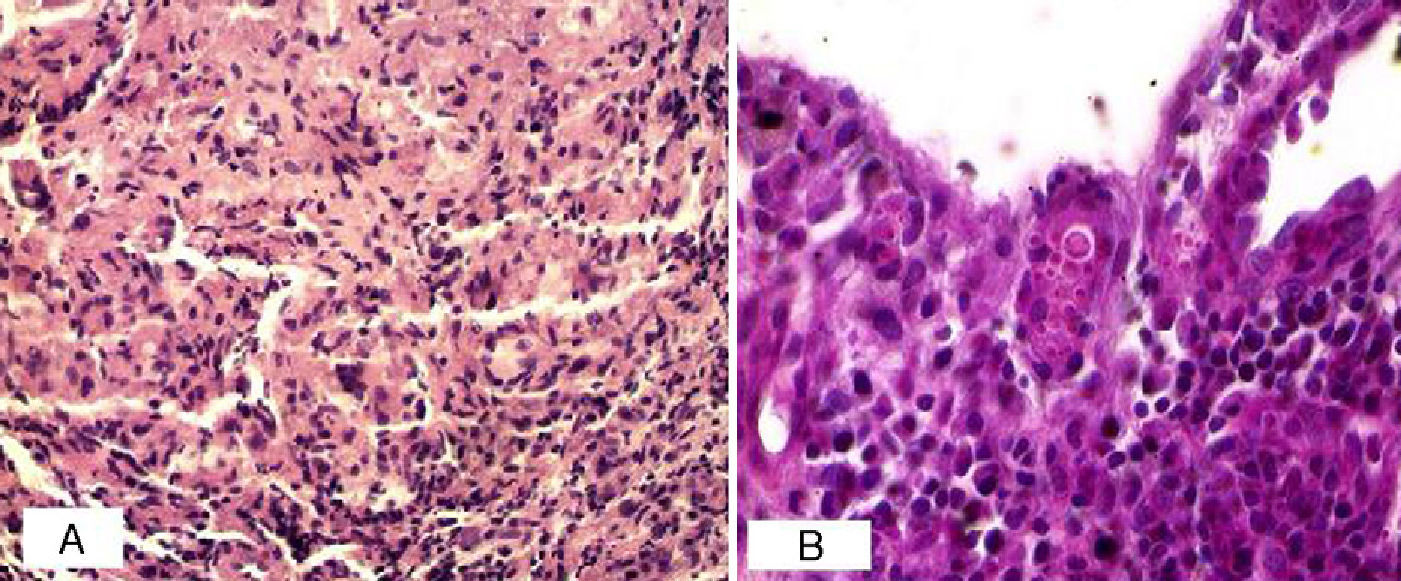
The most relevant laboratory findings were eosinophilia (7%) and an erythrocyte sedimentation rate of 78mm in the first hour. The patient tested negative for human immunodeficiency virus (HIV) and had a Venereal Disease Research Laboratory test result of 1:2. Chest radiography showed a mild interstitial infiltrate at the base of both lungs and histopathology revealed an intense granulomatous reaction in the dermis, with numerous multinucleated giant cells containing small, round, thick-walled structures with double contour membrane, some with surface buds and others showing multiple budding. These cells stained positively with periodic acid-Schiff stain (Fig. 3).
Treatment with itraconazole 200 mg/d achieved a good therapeutic response at initial monthly assessments. The patient is now in his eighth month of treatment and the therapy will be continued for at least another 4 months.
PCM is a deep mycosis that primarily affects male agricultural workers. The male to female ratio is approximately 9 to 1. In women, the infection occurs before menarche or after menopause. P brasiliensis has cytoplasmic receptors for 17-β-estradiol, a female hormone that inhibits the mycelial-to-yeast transformation, an essential step in the establishment of infection. The age of affected patients ranges between 15-24 years and 65-74 years, with incidence peaking in the older patients.1–4
Clinically, the condition can presents as PCM infection (which can be asymptomatic or subclinical or else a symptomatic primary infection) or PCM disease, which can be acute or chronic. There are several forms of PCM disease, including juvenile (affecting children and adolescents), adult (unifocal or multifocal), and residual disease. The most frequent clinical form is chronic multifocal disease with pulmonary and mucocutaneous involvement. In HIV-positive patients with acquired immunodeficiency syndrome the clinical features are those of the acute juvenile form but with the addition of granulomatous mucosal lesions and diffuse pulmonary involvement.5–7
There are numerous clinical manifestations, which include general symptoms, enlarged lymph nodes and lesions in the lungs, bones, and other organs, including (in order of frequency) the gastrointestinal tract, liver, spleen, and adrenal glands. The lymph nodes may suppurate and become necrotic, giving rise to fistulas similar to those observed in tuberculosis.5,6
The most common manifestations are mucocutaneous lesions; when these affect the mucosas of the nose, mouth, pharynx, and larynx, they can take 3 forms: a) de Aguiar Pupo stomatitis (mulberry stomatitis); b) inflamed and deformed lips (tapir lip); and c) infiltrative, vegetative, and ulcerative lesions. Cutaneous lesions take various forms as follows: papular, vegetating papular-pustular, ulcerative-vegetative, and papular-tuberous with pinpoint hemorrhages and a mulberry-like appearance. In the nasal region crusted ulcerated lesions that destroy the septum mimic American cutaneous leishmaniasis, one of the diseases that should be included in the differential diagnosis.5,6
PCM is diagnosed on the basis of 2 types of findings: a) Epidemiological information obtained from the medical history; and b) Demonstration and isolation of the fungus using any of the following methods: direct microscopic examination of exudate from lesions using potassium hydroxide smear or Giemsa or Groccot staining; culture on Saboureaud or blood agar; or histopathologic procedures demonstrating ‘pilot's wheel’ structures either within multinucleated giant cells or floating free in areas of suppuration. In the present case, the patient was a male agricultural worker and a smoker, and fungal structures were identified in a biopsy specimen.
The first-line treatment is oral itraconazole 200-400 mg/d for 6 to 12 months in mild cases and 12 to 18 months in moderate cases. Severe disease is treated with intravenous amphotericin B.6,7
Please cite this article as: Di Martino Ortiz B, Rodríguez-Oviedo ML, Rodríguez-Masi M. Paracoccidioidomicosis crónica multifocal de tipo adulto en paciente inmunocompetente. Actas Dermosifiliogr.2012;103:645-646.