An 83-year-old woman with a history of hypothyroidism and depression, which was being treated, was referred to our department by the rheumatology department, where she was in follow-up for osteoporosis. She reported the gradual appearance of asymptomatic nodules on the forearms; the nodules had appeared a year earlier and were not associated with prior trauma or any other trigger.
Physical ExaminationThe patient presented between 8 and 10 subcutaneous nodules in the cubital region of both forearms; the nodules measured between 0.5 and 1.5cm in diameter, were of a rubbery consistency, skin-colored, with a smooth surface, rounded, and arrayed in a line (Fig. 1). The patient presented joint deformities of the metacarpophalangeal joints with no signs of arthritis, and no other skin lesions were observed.
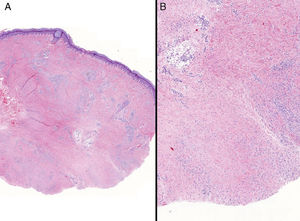
HistopathologyInvolvement of the entire thickness of the dermis was observed, with foci of partial collagen degeneration, surrounded by a discrete lymphohistiocytic infiltrate (Fig. 2).
Additional TestsTests revealed elevated PCR (30.7mg/L); ANA (+) at a 1/320 titer, and anti-ENA (+); SS-A, 68U/mL. Other parameters (hemogram, biochemistry, erythrocyte sedimentation rate, rheumatoid factor, anti-CCP2, urinary sediment, proteinogram, immunoglobulins, C3, C4, anticardiolipin antibodies) were normal or negative. X-ray of the hands, forearms, and spine showed signs of degeneration and reduced bone density.
What Is Your Diagnosis?DiagnosisSubcutaneous granuloma annulare.
Clinical Course and TreatmentBecause of the pain reported by the patient, after a 1-year follow-up period, treatment with 2 intralesional injections of triamcinolone in suspension at a concentration of 1:2 was instated, followed by oral vitamin E (200mg/d) for 6 months. The condition resolved completely and no relapse was observed in the last 10 months of follow-up (Fig. 3).
CommentGranuloma annulare (GA) is a benign form of dermatosis of uncertain origin and is generally self-limiting; it may present different clinical forms, the most common of which are localized, generalized, subcutaneous, and perforating GA.1 Several rare or atypical patterns of GA exist, including follicular GA, macular GA, patch GA, and linear GA.1,2 Subcutaneous granuloma annulare (SGA) is a rare variant of GA and is more frequent in children. It is characterized by the appearance of asymptomatic unadhered nodules of variable size and a firm elastic consistency, with normal overlying skin.3,4 The most frequent locations are the head, lower extremities, forearms, and backs of the hands and feet.3,4 Diagnosis is clinical and histologic, and the disease presents a broad differential diagnosis that includes abscesses, calcified hematomas, soft-tissue tumors, fat necrosis, reaction to foreign bodies, and interstitial granulomatous dermatitis. Histopathologic differentiation, however, should principally include rheumatoid nodules (RN).4,5 Differentiation may be difficult, as both diseases present a granulomatous dermal infiltrate consisting of an area of collagen necrobiosis surrounded by palisading histiocytes.4,5 RN present better circumscribed abnormal connective tissue located more deeply and fibrin deposition in the collagen is highly characteristic.4,5 RN tend to have giant cells in the palisade of histiocytes, but the key histiologic finding for differentiating the diseases is the presence of mucin in the area of necrobiosis in SGA.4,5 In our patient, we identified mucin deposits using colloidal iron and Alcian blue, which together with negative results for RF and anti-CCP2 and the absence of clinical findings of rheumatologic disease, aided us to perform the differential diagnosis between the 2 processes. With respect to treatment, many drugs have been proposed with variable results; the most accepted approach is not to treat.3,4 In our case, we decided to treat, with an excellent response; nevertheless, the possibility that remission was spontaneous cannot be ruled out. Few cases of SGA or linear GA have been reported and we have found no cases similar to ours. We would like to highlight the exceptional nature of the clinical presentation, in the form of linear beaded nodules, which has not been described to date. While this is an atypical presentation, the potential diagnosis of SGA should be taken into account to avoid unnecessary treatment.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: García Río I, Heras Gonzalez S, Martínez Gonzalez MI. Beaded Nodules on the Forearms. Actas Dermosifiliogr. 2019;110:597–598.