Hypersensitivity reactions to drugs have a very varied clinical spectrum and can present different types of skin lesion, including erythema nodosum.
A 44-year-old woman with no known drug allergies, diagnosed with Crohn disease 2 years earlier, had started treatment with azathioprine (AZT) 3 weeks prior to consultation because of laboratory and radiological signs of progression of her Crohn disease. She came to the emergency department with a 7-day history of painful erythematous lesions on both lower limbs, associated with general malaise, loss of appetite, and knee and ankle pain. She did not report fever.
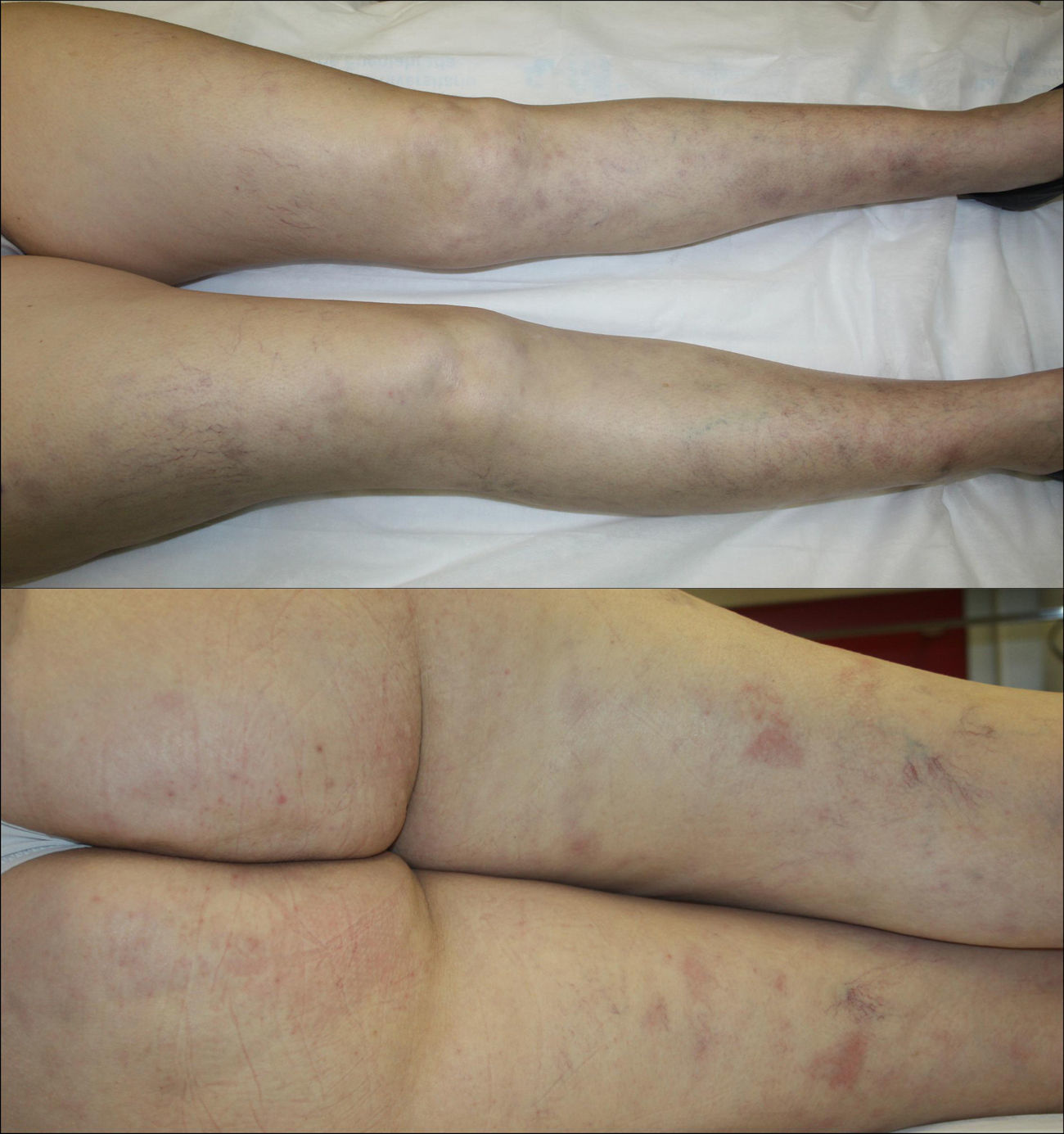
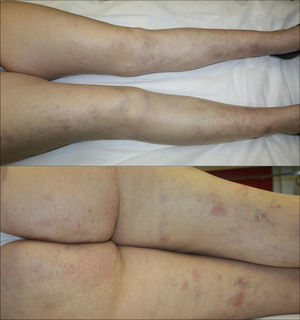
Examination revealed multiple disperse, occasionally tender, erythematous subcutaneous nodules measuring between 10 and 20mm on both lower limbs. There were also a number of violaceous macules of residual appearance measuring 15 to 20mm in diameter (Fig. 1).
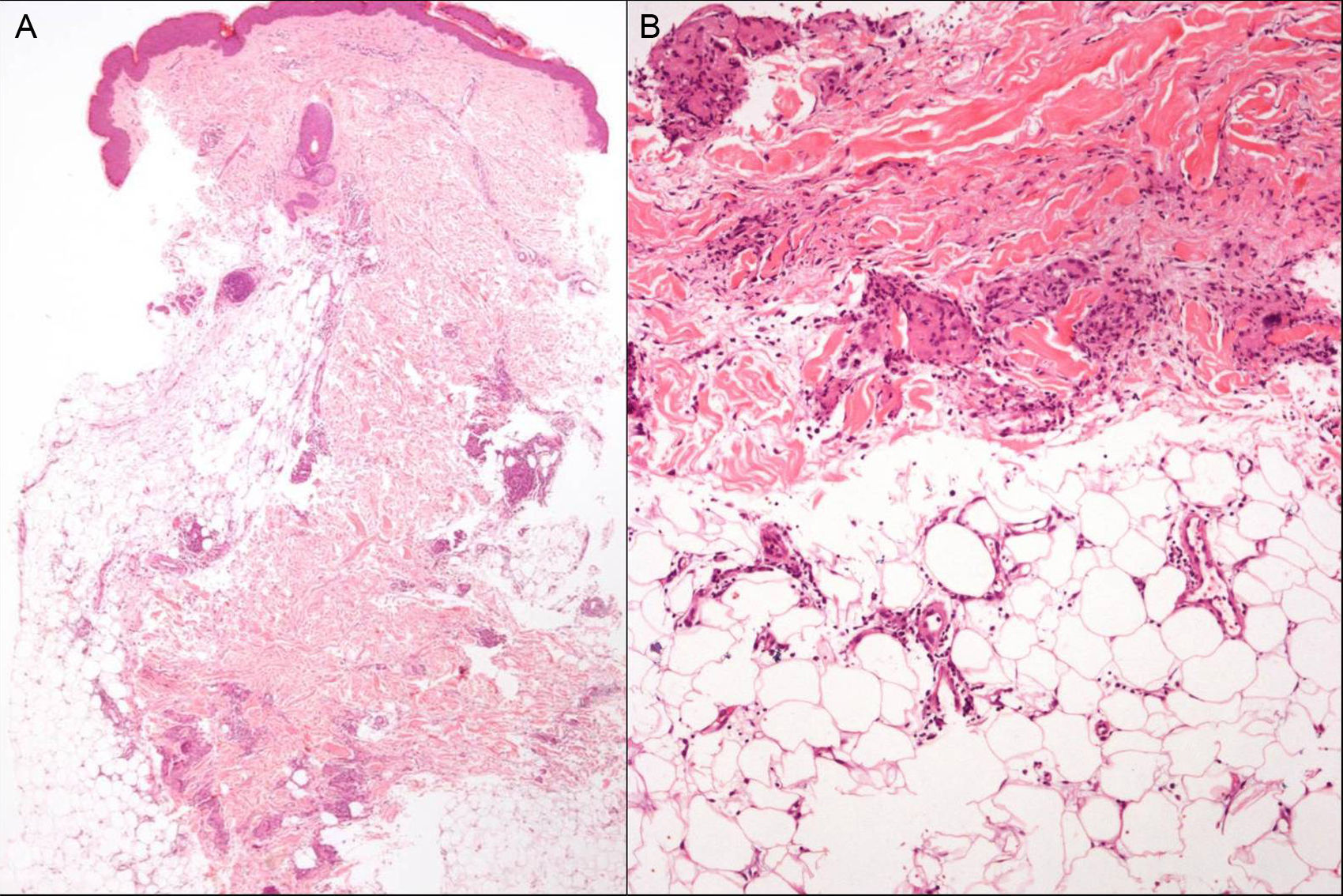
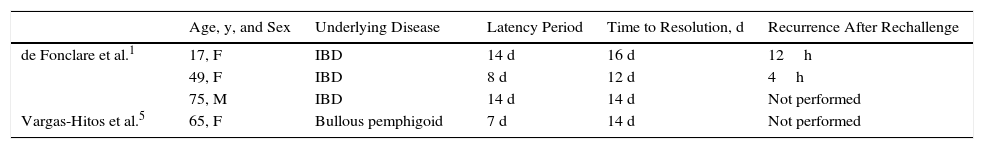
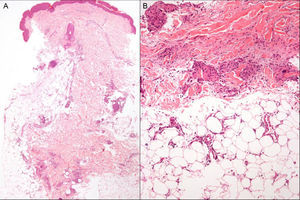
Histopathology of a lesion showed thickening and fibrosis of septa in the subcutaneous cellular tissue, with a chronic inflammatory infiltrate formed of histiocytes and lymphocytes, and granulomas with multinucleated giant cells were also present (Fig. 2,A andB). No microorganisms were observed on staining with periodic acid-Schiff, Gram, and Ziehl-Neelsen stains. Laboratory findings were as follows: hemoglobin, 10.4g/dL; mean corpuscular volume, 78.4fL; mean corpuscular hemoglobin, 25.3pg; elevation of the transaminases (alanine aminotransferase, 82U/L); γ-glutamyl transferase, 126U/L; C-reactive protein, 12.59mg/dL (normal range, 0.1-0.5mg/dL); and no abnormalities in the autoimmunity study. There was no induration on the tuberculin skin test and chest x-ray showed no changes (Table 1).
Review of Published Cases of Erythema Nodosum as a Hypersensitivity Reaction to Azathioprine.
| Age, y, and Sex | Underlying Disease | Latency Period | Time to Resolution, d | Recurrence After Rechallenge | |
|---|---|---|---|---|---|
| de Fonclare et al.1 | 17, F | IBD | 14 d | 16 d | 12h |
| 49, F | IBD | 8 d | 12 d | 4h | |
| 75, M | IBD | 14 d | 14 d | Not performed | |
| Vargas-Hitos et al.5 | 65, F | Bullous pemphigoid | 7 d | 14 d | Not performed |
Abbreviations: F, female; IBD, inflammatory bowel disease; M, male.
Given the possibility that the lesions could have been due to the AZT, it was decided to interrupt the treatment. This led to the resolution of systemic symptoms within 24h and of the skin lesions within 3 days, with no other treatment. Based on these findings, we made a diagnosis of hypersensitivity reaction to AZT with cutaneous manifestations in the form of erythema nodosum.
AZT is a precursor of 6-mercaptopurine and is used as an immunosuppressant drug for the treatment of chronic inflammatory diseases such as inflammatory bowel disease (IBD).
Adverse effects associated with this drug are subdivided into early and late reactions.
Early reactions, including hypersensitivity reactions, are common.1 These are idiosyncratic reactions that occur in approximately 2% of patients in the first 4 weeks of treatment, though they are probably underdiagnosed.1,2 Clinically they can present with fever, hypotension, general malaise, joint pain, gastrointestinal symptoms, hepatitis, pancreatitis, nephritis, pneumonia, pericarditis, and skin lesions.1,3 After the interruption of treatment, the lesions resolve rapidly, within 2 to 3 days.2 Many cases are initially diagnosed as infectious diseases or exacerbations of the underlying disease, and the hypersensitivity reaction may not be detected until re-exposure to the drug.2,3 Symptom recurrence after rechallenge to the drug will confirm the cause-effect relationship, but as the reaction is more intense and develops more rapidly, occasionally within a few hours,3 rechallenge is contraindicated.2 Patients with IBD have been considered to be at greater risk of hypersensitivity reactions to AZT; this may be due to a polymorphism in the gene that codes for inosine triphosphate pyrophosphatase.4
In 2011, Bidinger et al.2 reviewed all published cases of hypersensitivity to AZT, finding that approximately 50% presented cutaneous manifestations. The most common cutaneous presentation was Sweet syndrome, followed in order of frequency by nonspecific maculopapular, vesicular, pustular, or urticarial rashes, small-vessel vasculitis, erythema nodosum,1,5 and acute generalized exanthematous pustulosis. A dozen more cases with skin involvement have been published since that time, the majority presenting as Sweet syndrome, though also including 2 cases of neutrophilic eccrine hidradenitis,6,7 an association not previously described. The most common histopathology finding is a neutrophilic dermatosis.2
Erythema nodosum associated with IBD is observed in up to 10% of patients with ulcerative colitis and 15% of those with Crohn disease. The course of the skin lesions usually parallels activity of the bowel disease and resolve with appropriate treatment of that disease.8
Late reactions, such as myelosuppression, are dose dependent and can be avoided to a great extent by measuring activity of the enzyme thiopurine methyltransferase.1
In our patient, the lesions resolved within 3 days without treatment. After resolution of the alterations, treatment was started with infliximab, which had to be interrupted due to an infusion reaction and possible drug-induced dermatitis. A year after consultation, the patient has presented occasional outbreaks of her bowel disease, presenting as episodes of subacute intestinal occlusion, but no further episodes of erythema nodosum.
The presence of erythema nodosum lesions in patients on treatment with AZT who do not present signs of an exacerbation of IBD or intercurrent infection must alert us to a possible hypersensitivity reaction to the drug.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: González-Olivares M. Eritema nudoso como reacción de hipersensibilidad a la azatioprina. Actas Dermosifiliogr. 2017;108:591–593.