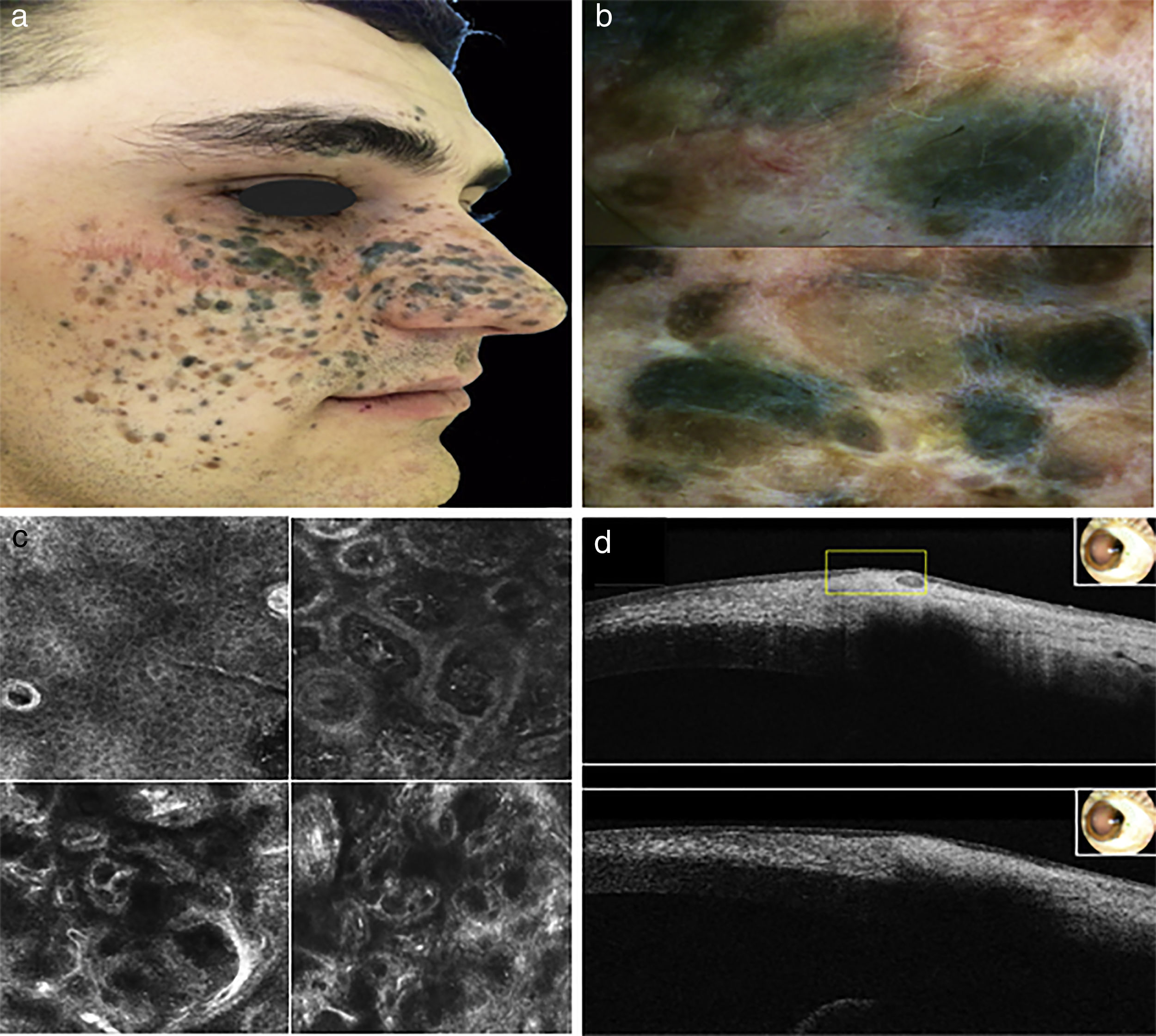
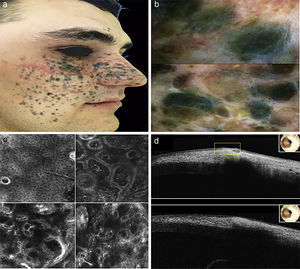
Together with Mongolian spot, Ota's naevus, Ito's naevus, blue nevi are believed to represent a dermal arrest in embryonal migration of neural crest melanocytes that fail to reach epidermis. They usually appear in childhood but sometimes later in life.1 After a trauma, damaged keratinocytes and inflammatory cells can release alpha-Melanocyte-stimulating hormone, that could influence nevus cells to form larger nests and macroscopically visible nevi.2 Blue nevi usually are solitary bluish-pigmented neoplasms, rarely are multiple and clustered in a well-circumscribed area, as agminated subtype. The Latin term “agmen” means “army” and indicates this rare flat or raised arranged group of nevi.3,4 These lesions are distributed on trunk, extremities and head/neck.5 A twenty-year-old Bulgarian, phototype IV boy presented with multiple asymptomatic pigmented lesions on right hemiface involving the three major branches of trigeminal nerve, developed since 18 months of age after a trauma. He underwent surgical treatments to reduce the involved area. Family history for skin cancer was negative. We observed approximately 100 maculo-papular, blue and brown lesions of different sizes, forming a cluster of nevi (Fig. 1a). The skin around papules was not discolored nor indurated. The surgical scar was not free of pigmentary process. Dermoscopy revealed homogeneous pattern with diffuse brownish areas, regular network at the periphery and numerous regularly distributed small dots or homogeneous blue-gray pattern (Fig. 1b). No background pigmentation was noted between lesions. Moreover we performed Reflectance Confocal Microscopy (RCM) and a single lesion was excised for histological evaluation, disclosing typical findings of blue nevus. RCM displayed a regular epidermal architecture with a typical honeycomb pattern. At the spinous- granular layer we observed bright and polygonal keratinocytes with dark central nuclei. At basal layer we observed a single layer of refractive cells with cobblestone pattern. The dermo-epidermal junction was preserved with dermal papillae surrounded by luminous cells, with round nucleous and elongated cells, correlating to inflammmatory cells and melanophages. Within upper dermis, we noticed irregular bright area corresponding to collagen bundles. Irregular refractive structures with unvisible nucleous were observed within dermal papillae of reticular dermis corresponding melanophages, inflammatory cells and dendritic melanocytes (Fig. 1c). Histologic examination revealed deep and concentrated dermal fusiform or dentritic- like melanocytes, not arranged in clusters. Thickening of the connective tissue with melanophages was also observed. No bluish stain of the ipsilateral eye was observed and ophthalmic evaluation demonstrated a stromal corneal melanosis in the caruncle and corneal-limbal complex. Optical Coherence Tomography (OCT) visualized hyperreflective regular structure with definite margins in both regions (Fig. 1d). No pigmented areas were found under otolaryngological examination. Nuclear Magnetic Resonance displayed normal morphological and dimensional features and did not reveal signal intensity alterations of brain parenchyma. We report a case of a boy with congenital large agminated blue pigmented lesion within area of Ota's nevus. The nevus enclosed distribution of the first, second divisions of the trigeminal nerve, but also extended into the third branch, which is rarely seen in Ota's nevus. Physical exam revealed several maculo-papular blue and brown lesions, but the skin between papules appeared not discolored nor indurated. No bluish discoloration of the eye was observed, but a stromal corneal melanosis in the caruncle and corneal-limbal complex is also present. Furthermore no oral mucosal or neurological lesions were noted. Moreover, histologic examination showed dermal melanocytes are deeply located and densely packed. These features were consistent with diagnosis of blue nevus. However, it would appear that the blue nevus, Mongolian spot and the nevus of Ota are closely related and possibly represent different entities within the spectrum of blue lesions.6 Considering these results and treatment limitations due lesion size, a 3-months-follow-up of patient was followed, carrying out multidisciplinary management to rule out malignant changes. Dermoscopy is important for early detection of malignant transformation: agminated blue nevi are commonly characterized by homogeneous pattern with diffuse brownish areas, in combination with peripheral typical network and small dots. Furthermore, Pizzichetta reported darker sulci, brown veil and pseudopods.7 RCM is limited by penetration depth, but can identify malignant features, as pagetoid melanocytosis, cellular atypia, epidermal disarrangement.8 The extracutaneous assessment to exclude ocular, neurologic and otolaryngoiatric involvement should be performed routinely. OCT imaging provides optical signs of ocular surface lesions, demonstrating benign findings as hyper-reflective appearance, well circumscribed lesion, regular margins, no invasion of surrounding tissue. Moreover, patients affected by multiple blue nevi, agminated blue nevus or giant blue nevus, particularly caucasians, should be monitored for ocular/orbital involvement and followed closely for signs of rapid growth. Indeed, in blue nevi and uveal melanoma occur somatic mutations in Guanine Nucleotide-binding Protein G(q) (GNAQ), protein encoded by GNAQ gene. These mutations turn GNAQ into a dominant acting oncogene, causing melanocytic neoplasia.9,10 We described a case of agminated dermal melanocytosis in the territory of Ota's nevus, enriching the spectrum of bluish pigmented lesions. Moreover, an integrated team is needed to optimally manage patients with rare neoplasm.
a) Clinical aspect of pigmented lesion b) Dermoscopic features c) RCM in the top left corner: spinous-granular layer of epidermis. In the top right corner: dermo-epidermal junction and upper dermis. In the bottom left corner: upper dermis. In the bottom right corner. Reticular dermis d) OTC images.
The authors declare that they have no conflicts of interest.
The authors would like to thank Lucia Pietroleonardo for RCM analysis.
Please cite this article as: Diluvio L, Mazzeo M, Bianchi L, Campione E. Melanocitosis dérmica agminada en el territorio del nevus de Ota. Actas Dermosifiliogr. 2018;109:653–655.