A 32-year-old woman consulted for an asymptomatic lesion that had been present on the mid sternum for 12 years, unchanged in size or shape. She was concerned about the cosmetic effect of the lesion, as it looked like a surgical sternotomy scar. The only relevant background was a scoliosis that had required treatment using a corset during childhood.
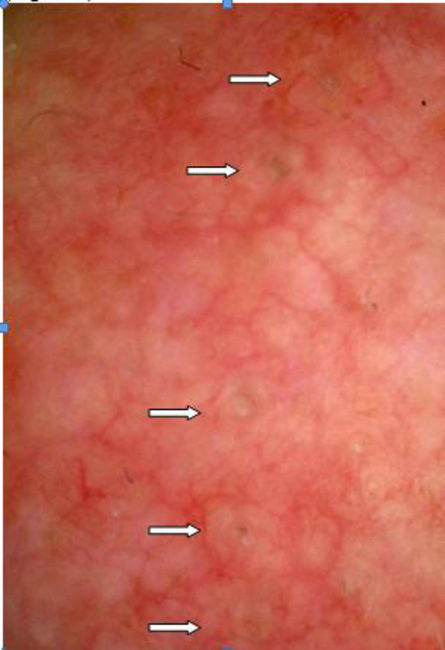
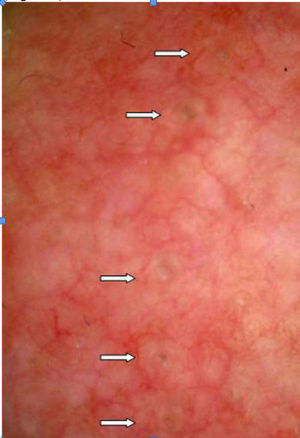
Physical ExaminationA linear midline lesion of approximately 5cm in length was observed. It was formed of papular lesions with central follicular openings that simulated open comedos arranged in line, one after the other (Fig. 1).
Additional TestsEpiluminiscence examination made the follicular openings clearly visible; they were found to be full of a homogeneous brownish material (Fig. 2).
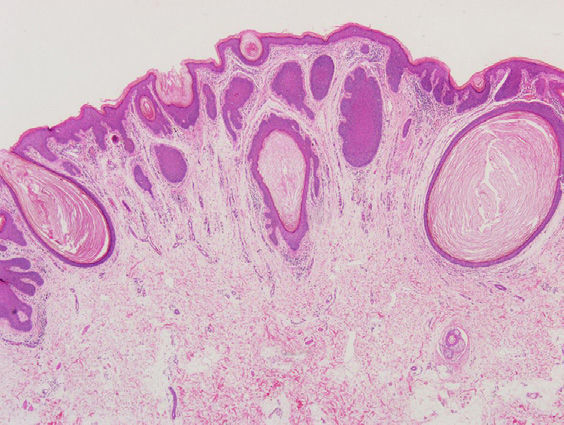
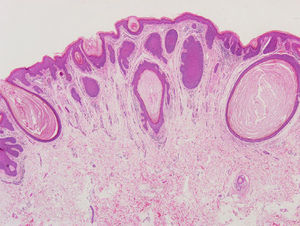
Histology revealed infundibular dilatations, with no hairs, in the form of contiguous epidermal invaginations into the dermis, filled by laminar keratin (Fig. 3).
Chest x-ray revealed a moderate dorsolumbar scoliosis that had been partially corrected years earlier.
Ophthalmologic examination of the right eye revealed an asymptomatic subcapsular cataract, which could have been of recent onset.
Neurologic examination was rigorously normal.
What Is Your Diagnosis?
Nevus comedonicus.
Clinical Course and TreatmentTreatment was started with 0.1% retinoic acid, leading to a notable improvement within a few days, leaving a barely perceptible residual lesion.
CommentNevus comedonicus is considered to be a variant of epidermal nevus. It is formed of infundibular dilatations filled by keratin, similar to typical comedos, and it usually arises on the face and neck. The prevalence of this condition is estimated at between 1 in 45 000 and 1 in 100 000 patients, with no gender or racial differences.1 Most commonly it is present at birth or appears during infancy. The typical presentation of these dilated follicles is grouped in a plaque or honeycomb distribution, although we may observe other patterns: unilateral or bilateral, linear, segmental, or Blaschkoid.1 The clinical appearance is usually sufficient to make the diagnosis, although epiluminescence can be useful, as it can make follicles visible as papules with openings filled by brown-colored plugs; the dermoscopic image of acne vulgaris would show numerous superficial comedos of light or dark brown or black color, depending on the type of acne (open or closed comedos).2 In case of doubt, histology will confirm the diagnosis.1
Nevus comedonicus can occur as an isolated finding3 or, more rarely, be associated with ocular, skeletal, or central nervous system changes, forming part of a neurocutaneous syndrome called nevus comedonicus syndrome. The most common changes described in this syndrome are cataracts (typically ipsilateral), scoliosis, vertebral fusions, spina bifida, and mental retardation, although many and varied alterations have been reported in the literature.1,3,4 The appearance of epithelial tumors within the lesion have also been reported, in particular trichoepitheliomas, syringocystadenoma papilliferum, keratoacanthoma, and, more rarely, basal cell and squamous cell carcinomas.1
In the absence of complications or marked cosmetic alterations, management is conservative. First-line treatment is with keratolytics and topical retinoids. Laser therapy or surgical excision can be considered in some cases.1 The possible associated diseases must be taken into account, and periodic follow-up of the lesion should be performed to detect skin tumors.
In conclusion, we have described the clinical and dermoscopic characteristics of a new case of linear nevus comedonicus of uncertain time since onset, associated with moderate scoliosis and a mild subcapsular cataract. Treatment with topical retinoids was effective. The prevalence of moderate scoliosis and subcapsular cataract is high in the general population, and this association may therefore be mere coincidence, in which case this would not be nevus comedonicus syndrome.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We would like to thank Dr. María J. Beato Merino of the Pathology Department of Hospital Universitario La Paz
Please cite this article as: Sánchez-Orta A. Lesión adquirida de distribución lineal en región preesternal. Actas Dermosifiliogr. 2016;107:597–598.