A man aged 80 years, with no past medical history of interest, consulted for an exophytic tumor that had arisen a year earlier in the frontal region and had grown progressively to its current size. There were no associated symptoms and the patient did not recall any history of trauma.
Physical ExaminationOn physical examination, a single, well-defined exophytic tumor with a cylindric polypoid morphology and a fibrinous and friable surface was observed in the left lateral frontal region (Fig. 1). The tumor measured approximately 4cm in its largest diameter and 3cm in height. There were no palpable locoregional lymph nodes.
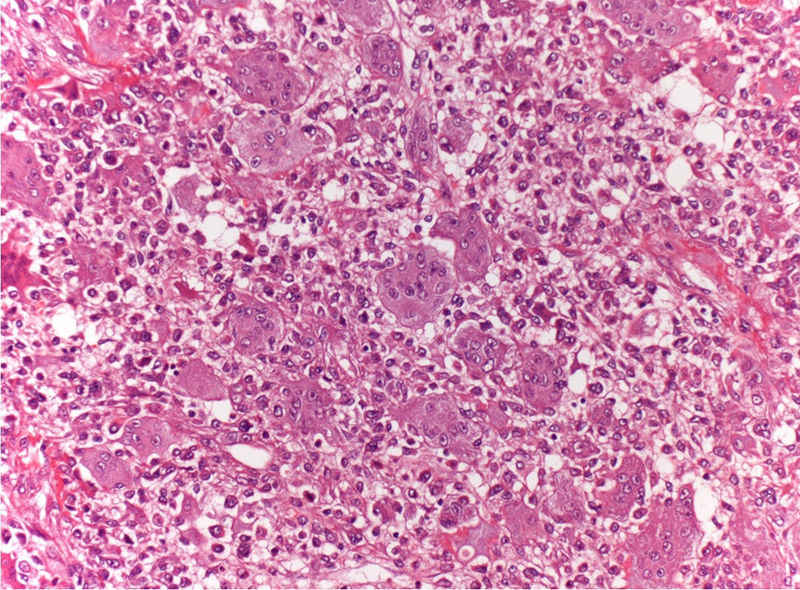
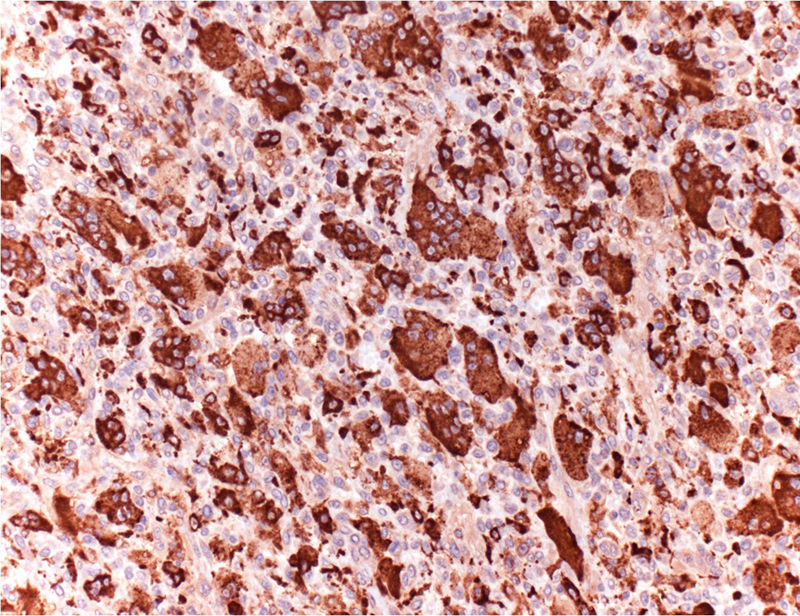
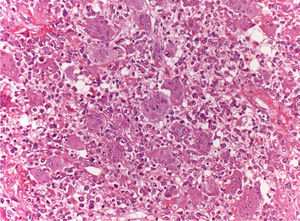
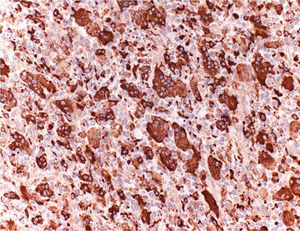
Additional TestsThe lesion was completely excised and the defect was closed using a full-thickness skin graft. Histopathology revealed the presence of tumor nodules in the dermis. The nodules were composed of monomorphic mononuclear cells, spindle-shaped cells, and multinucleated osteoclast-like giant cells, with no cellular atypia (Fig. 2). The number of mitoses was 3 per 10 high-power fields and the Ki-67 index was 21%. Immunohistochemistry was positive for CD68 (Fig. 3) and negative for S100 and pancytokeratins. No vascular invasion was detected.
¿What Is Your Diagnosis?
DiagnosisSoft tissue giant cell tumor of low malignant potential (STGCTLMP).
Clinical Course and TreatmentThe patient has attended follow-up in the dermatology unit for 2 years and has presented no local recurrence or lymph-node or distant metastases.
CommentSTGCTLMP is a rare neoplasm that presents in middle-aged men and women as an asymptomatic, well-defined tumor. Around 80 cases with similar characteristics have been reported, the majority located on the upper and lower limbs, in contrast to our patient, in whom the tumor was in the frontal region.1–5
Although STGCTLMP was initially included as a malignant soft tissue giant cell tumor, Folpe et al.2 subsequently proposed the term soft tissue giant cell tumor of low malignant potential as, in contrast to the former tumors, this neoplasm only presents mild or moderate atypia and an indolent clinical course.
They are considered to be the soft tissue analogy to giant cell tumors of bone, due to their histological and immunohistochemical similarity.2 Microscopically, STGCTLMP presents a monomorphic proliferation of mononuclear cells and osteoclast-like multinucleated giant cells distributed uniformly through the tumor, as was observed in our case. These tumors can present metaplastic bone formation peripherally and vascular invasion.3
The histological diagnosis is confirmed on immunohistochemistry. CD68, which is also expressed in epithelial and mesenchymal tumors such as atypical fibroxanthoma,6 is detected in the cytoplasm of the multinucleated cells. Tartrate-resistant acid phosphatase and smooth muscle actin are also positive, but CD45, protein S100, desmin, and lysozyme are negative, producing an immunophenotypic profile identical to that of giant cell tumors of bone.2 Additional tests demonstrate the extraosseus situation.3
The differential diagnosis should include mesenchymal tumors rich in osteoclast-like giant cells, such as the giant cell variant of malignant fibrous histiocytoma, plexiform fibrohistiocytic tumor, and extraskeletal osteosarcoma; these tumors have a more aggressive course. STGCTLMP must also be differentiated from atypical fibroxanthoma, an uncommon dermal tumor of uncertain histogenesis, considered by the majority of authors to be superficial variant of malignant fibrous histiocytoma, but with a better prognosis. This tumor typically presents as a solitary nodule in sun-exposed areas in elderly adults. Histologically, there is a predominance of spindle-shaped cells with large vesicular nuclei, associated with a variable number of giant cells, some of which are multinucleated, and polygonal cells with abundant eosinophilic cytoplasm.7 Other lesions rich in multinucleated giant cells include giant cell tumors of the tendon sheath and benign cutaneous fibrous histiocytoma.1
The prognosis is favorable if resection is complete, but local recurrence can occur after incomplete resection, as is seen with its osseous form. Lymph-node and lung metastases are very rare.4
We have reported a new case of STGCTLMP, a rare lesion that must be included in the differential diagnosis of soft tissue tumors rich in giant cells, as its clinical behavior, prognosis, and treatment differ significantly.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Almodovar-Real A, Aneiros-Fernández J, Ruiz-Villaverde R. Tumor de lento crecimiento en región frontal. Actas Dermosifiliogr. 2016;107:851–852.