A 72-year-old man was admitted to hospital with a chronic subdural hematoma; he had been on treatment with dexamethasone 12mg a day for the previous 3 months to prevent cerebral edema. During his stay, widespread subcutaneous nodules that had been present for 3 weeks were detected, associated with low-grade fever.
Physical ExaminationThe patient had multiple subcutaneous nodules in different areas of the body, but mostly affecting the trunk. They were hard to palpation and not fixed to the deep layers. Several of the nodules showed signs of inflammation (Fig. 1).
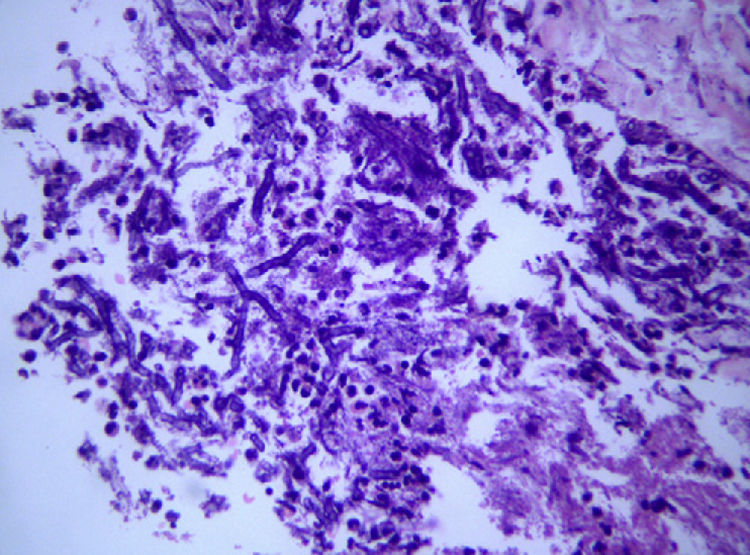
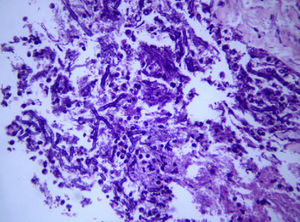
HistopathologyOne of the nodules was biopsied to obtain material for histology and the purulent material was drained. Hematoxylin-eosin staining revealed a dense inflammatory infiltrate in the deep dermis and the presence of septate hyphae with 45° branching (Fig. 2).
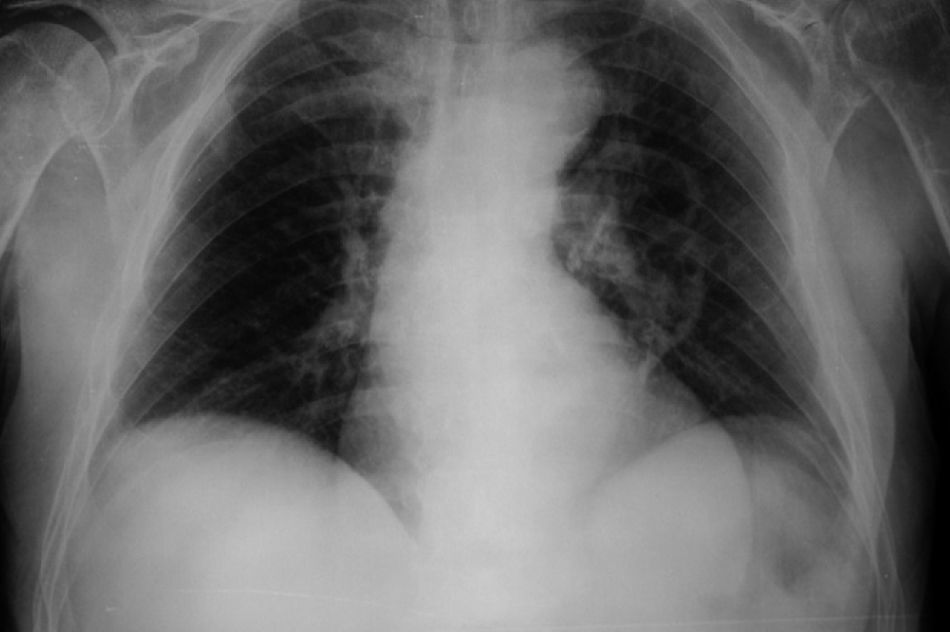
Additional TestsLaboratory tests showed leukocytosis with neutrophilia and the chest radiograph showed a cavitated lesion in the left parahilar region (Fig. 3). Chest computed tomography showed a well-circumscribed tumor measuring 5cm in diameter in the anterior segment of the left upper lobe, of heterogeneous density and with an air-fluid level. Fine-needle aspiration was performed but insufficient material was obtained for diagnosis. Blood cultures were negative.
What Is Your Diagnosis?
DiagnosisSecondary cutaneous aspergillosis.
Additional TestsCulture of the skin biopsy specimen and sputum were positive for Aspergillus fumigatus.
Clinical Course and TreatmentDespite intravenous treatment with caspofungin 50mg/24h and voriconazole 200mg/12h, the patient died on day 13 of admission.
CommentAspergillosis is an infection caused by Aspergillus species, the most common of which are Aspergillus flavus and A fumigatus. The infection tends to affect immunosuppressed patients as the main risk factors are neutropenia, corticosteroid therapy, and solid and hematological malignancies. Aspergillosis has also been associated with construction work or earth movements at or near hospitals due to the higher concentration of fungal spores in the environment.
Cutaneous aspergillosis has 3 clinical variants. The primary variant appears following direct inoculation of the fungus into the skin.1 The secondary, or hematogenous, variant occurs when the fungus travels from the lung to the skin via the bloodstream.2 Secondary aspergillosis accounts for just 4% of all cases of systemic aspergillosis.3 The third variant is the result of direct invasion by the fungus of the skin from an adjacent focus of infection, such as sinus infection. A flavus and A fumigatus are the most common causes of primary and secondary aspergillosis, respectively. Other, less common, causal agents are Aspergillus niger, Aspergillus terreus, and Aspergillus nidulans.
The diagnosis of cutaneous aspergillosis requires skin biopsy. Staining with periodic acid Schiff and methenamine silver reveals septate hyphae with uniform 45° branching. Cultures are useful for confirming diagnosis and identifying the species responsible for the infection. Blood cultures are negative in most cases. Histology together with chest radiographs and CT scans are essential for the diagnosis of primary lung infection. A sputum culture, however, is not very useful as it does not distinguish between lung colonization and invasive disease.
Treatments include intravenous voriconazole, posaconazole, amphotericin B, and caspofungin.4 Despite treatment, secondary cutaneous aspergillosis has an associated mortality of over 90%.5
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Masferrer E, Vidal D. Nódulos diseminados en un adulto inmunosuprimido. Actas Dermosifiliogr.2011;102:543-44.