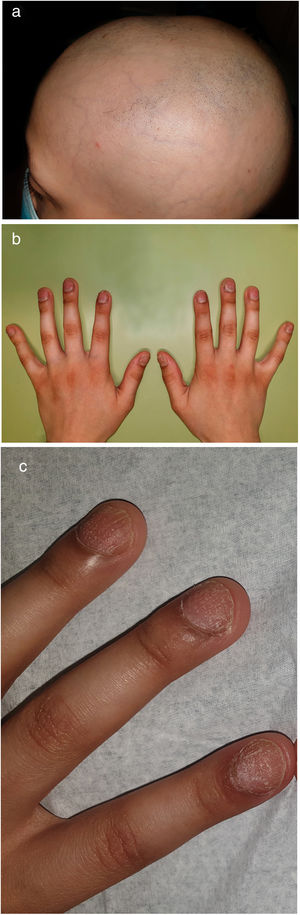
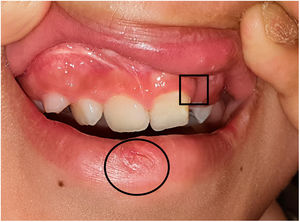
A 9-year-old Caucasian boy was referred to the outpatient Dermatology Department for alopecia and fingernail fragility, which had been notorious for the past nine months. On examination, there was multilocular alopecia with extensive confluent areas involving 70% of the scalp (Fig. 1(a)), with black dots and scattered exclamation mark hairs on trichoscopy, consistent with the diagnosis of alopecia areata. Eyebrows were also affected, especially the outer portion. Fingernail pitting and trachyonychia were evident on all digits (Fig. 1(b), (c)), with normal toe nails. In addition, a median lower lip pit was noted, and the patient had been previously submitted to the surgical correction of a cleft palate in early infancy (Fig. 2), which together define the diagnosis of Van der Woude Syndrome (VWS). Past medical history and physical examination were otherwise unremarkable. Namely, skin and limb abnormalities (such as popliteal pterygium, syndactyly, toe changes) or genitourinary malformations that could point toward Popliteal Pterygium Syndrome (PPS), an allelic variant of VWS, were absent. The existence of cleft lift/palate in the family members was denied by the parents. The patient was started on clobetasol 0.5mg/g lotion and minoxidil 5% solution, with a favorable response after one year (partial regrowth, with alopecia in 40% of the scalp). Genetic testing was positive for a heterozygous mutation in the interferon regulatory factor 6 (IRF6) gene, specifically the replacement of a T by A at position 178, resulting in the replacement of a tryptophan by an arginine at position 60 (c.178T>A (p.(Trp60Arg)), a previously undescribed variant.
VWS is a rare congenital genetic disorder which represents the most common form of syndromic orofacial cleft, and 2% of all cleft cases. It has an autosomal dominant inheritance of several different mutations in a single gene, namely the IRF6 gene, with high penetrance but variable phenotypic expression. Besides its varied expressivity, VWS has an allelic variant, the PPS Syndrome, which also results from mutations in the IRF6 gene, but presents with additional features besides congenital lip pits and orofacial abnormalities,1 which were not found in our patient.
The child was considered to be the index case in the family. In fact, 30–50% of VWS cases arise as de novo mutations.1 However, the presence of a mutation with reduced penetration could not be completely excluded, as genetic testing was not performed in the parents. There are approximately 170 different disease-causing mutations described in the IRF6 gene. Clinical phenotypes result from missense mutations, terminations, deletions, insertions, splicing site mutations, beyond others, but over 90% of IRF6 mutations are missense changes.1 Moreover, the same missense mutation has already been described to be responsible for both VWS and PPS.1 Nevertheless, as aforementioned, our patient phenotype was not compatible with PPS, and the identified mutation corresponds to a novel variant that so far has not been described.
IRF6 protein is related to the formation of connective tissue, namely of the head and the face. The role of IRF6 in epidermal proliferation was also demonstrated in humans in histopathological studies, which were performed in children with VWS who underwent surgical cleft palate correction. However, in opposition to PPS that presents with popliteal pterygium, there are no clinical skin or appendage changes so far described in association with VWS in humans (except for squamous cell carcinoma associated with chronic inflammation of the lip pits).2 Studies in mice have also shown that IRF6 is involved in keratinocyte proliferation and differentiation, and the mutant phenotype was highly similar to what was observed in repeated epilation (Er) mice, which show irregular hairloss.3 On the other hand, interferon (IFN) molecules (α,β,γ) are well-established players in alopecia areata physiopathology4 and interferon regulatory factors (IRF) are known to play a role in IFN-driven disease.5 Although other IRF besides IRF6 are frequently implicated, the pleiotropic effects of these pathways raise awareness for a possible non-coincidental co-occurrence of VWS and AA, and it should be matter of future investigation. Furthermore, studies have suggested a cooperative role of p63 and IRF6 in orofacial development in mice and humans,6 and mutations in TP63 gene cause a range of ectodermal dysplasias that include hair and nail abnormalities. Although these differ from alopecia areata, the link between IRF6 ant TP63 should merit further interest.
The present case describes a new IRF6 mutation, although the experimental design lacks a direct functional test. It also raises awareness for a potential undescribed association between a common hair disorder and a rare genetic syndrome. Thus, it specifically sparks further interest in understanding the complex pathophysiological interplay on the involved pathways. Furthermore, it highlights the importance of Dermatologists in addressing the need for multidisciplinary endeavor of these syndromes.
Conflicts of interestThe authors declare that they have no conflicts of interest.