The Wound-QoL is a validated and feasible questionnaire for measuring disease-specific health-related quality of life in chronic wounds, originally developed for use in German.
The objective of this study was to translate the Wound-QoL for use in clinical care and in clinical trials in Spain and to validate this version.
Materials and methodsTwo independent fourth- and back translations of the Wound-QoL from the original German version were conducted, followed by an expert consensus of the resulting versions. After refinement, the final tool was piloted in N = 10 patients and then used in the validation study.
ResultsA total of 115 patients were recruited. Mean age was 69.5 (SD 14.5) years, 60.0 % were female. The Spanish version of Wound-QoL showed high internal consistency (Cronbach’s alpha > 0.8 in all scales). Factor analysis resulted in the same scales as the original version. There were satisfactory distribution characteristics of the global score and the subscales. Construct validity and convergent validity with other outcomes (generic QoL, healing rate) were satisfactory. The vast majority of patients considered the Wound-QoL a simple and feasible tool. Mean time needed for completing the questionnaire was 5 minutes. Overall, 99.1 % of the participants found it easy to understand the questions and 94.7 % stated that the questionnaire suits the personal situation.
ConclusionsThe Spanish version of the Wound-QoL shows good validity in clinical practice. It can be recommended for use in clinical routine and trials.
El Wound-QoL es un cuestionario validado para medir la calidad de vida en pacientes con heridas crónicas, que fue desarrollado originalmente para su uso en alemán. El objetivo de este estudio fue traducir el cuestionario Wound-QoL para su uso en la práctica clínica y estudios de investigación en España, así como validar esta versión.
Materiales y métodosSe realizaron dos traducciones independientes del Wound-QoL, directa e inversa, a partir de la versión original en alemán, seguidas de un consenso de expertos sobre las versiones resultantes. Después de su perfeccionamiento se realizó un estudio piloto y posteriormente el estudio de validación.
ResultadosSe incluyó un total de 115 pacientes. La edad media fue de 69,5 (DE 14,5) años, de los cuales el 60.0% eran mujeres. La versión española del Wound-QoL mostró una excelente consistencia interna (índice alfa de Cronbach > 0.8 en todas las escalas). El análisis factorial dio como resultado las mismas escalas que la versión original. Se objetivaron características satisfactorias de la distribución de la puntuación global y de las subescalas. La validez de constructo y la validez convergente con otros resultados (calidad de vida genérica, tasa de curación) fueron satisfactorias. La gran mayoría de los pacientes consideraron que el cuestionario era una herramienta sencilla y factible.
ConclusionesLa versión española del Wound-QoL muestra una excelente validez en la práctica clínica. Por lo tanto, puede ser recomendada para su uso tanto en la rutina clínica como en los ensayos.
Assessment of health-related quality of life (HRQoL) has become a key component of managing chronic wounds since it reflects patient perspective of disease and treatment1–5. Thus, quality of life (QoL) instruments have been introduced in clinical care6–10, quality management11–14 and clinical trials15,16. Several questionnaires have been validated and tested for use such as the Nottingham Health Profile, the Cardiff Wound Impact Schedule17, the Würzburg Wound Score18 and the Freiburg Life Quality Assessment for wounds (FLQA-w)19. Recently, a multinational study developed and approved an instrument deriving from the three validated questionnaires and presented data on several types of wounds20. This questionnaire named Wound-QoL resulted in a shorter, better to apply and well accepted questionnaire by the patients4. Moreover, it appeared that the questionnaire provided enhanced validation characteristics, too20.
In the meantime, the Wound-QoL has been linguistically validated into several languages, including English, German, French, Italian, Dutch, Swedish, Polish and Danish according to international guidelines for patient-reported outcomes (PRO) instrument development21. Beyond the formal translation process, a Spanish version was now tested regarding its operating characteristics and psychometric properties for clinical use. In order to conduct rigorous cross-cultural research to evaluate outcomes from new treatments and generalisation of observed treatment effects beyond national borders, operating characteristics between the original German and Spanish samples were inspected.
The objective of this study was to translate the Wound-QoL for use in clinical care and in clinical trials in Spain and to validate this version.
MATERIAL AND METHODSStudy design and sampleFirst, a validated desk-based translation process was conducted, followed by a prospective, longitudinal non-interventional validation study in a cohort of patients with chronic wounds of the lower extremities. For the longitudinal study, patients were examined and completed questionnaires at baseline (T1) and after a follow-up period of two to three months (T2).
Patients with leg ulcers of various underlying causes were recruited in the dermatology departments of five Spanish University Hospitals. Inclusion criteria were an active chronic wound of the lower extremity, age ≥ 18 years and the capability to understand and fill in a Spanish questionnaire. Patients were only included after informed consent. The study was approved by the Comité Ético de Investigación Clínica del Hospital General Universitario Gregorio Marañón code “Wound-PRO”, on July 27, 2016. The license holders of the Wound-QoL also agreed on the adaption and validation.
Instruments used in the validation studyThe Wound-QoL questionnaire consists of 17 questions i.e. items. Each item is scored on a five-point Likert scale from 0 = not at all to 4 = very much. The mean rating of all questions results in the global score. Additionally, the three subscales everyday-life, body and psyche were determined in the original version of the Wound-QoL22. Fourth and back-translations of the original German Wound-QoL questionnaire were conducted following international guidance15. Briefly, the original German version was submitted to two Spanish native speakers who independently translated it into Spanish. These two versions were retranslated into German by two further German native speakers. The resulting two German versions were then compared with the original version and a semantic discussion on any deviation was conducted itemwise. This discussion included the original first author of the questionnaire, two physicians and psychologists familiar both with German and Spanish language and a linguist. After refining the Spanish version, a feasibility test was conducted in 10 patients from Spain. The objective of this test was to analyse if the patients feel comfortable with the questionnaire and understand the questions in the same way. We also wanted to find out how long it takes to complete the questionnaire under routine conditions. The questionnaire appeared to show no problems in terms of understanding and feasibility. A content adaption was not necessary. Fig. 1 shows the Spanish version of the Wound-QoL that was used in this validation study.
General patient data on socioeconomic and clinical background were obtained following a specific assessment of the wound condition based on a standard case report
Besides the Spanish version of the Wound-QoL, the following questionnaires were used:
- •
EuroQoL five dimensions questionnaire (EQ-5D): a generic instrument reflecting health condition and quality of life in a validated Spanish version23
- •
Pain: numerical rating scales (NRS) from 0–1024
- •
The three visual analogue scales (VAS) included in the FLQA-w quality of life assessment, a validated, widely used specific quality of life questionnaire for wounds which was translated into Spanish the same way as the WoundQoL (independent translation/backtranslation)25
Due to the lack of recommendations on a priori sample size calculations in validation studies26, the size of the study population was determined based on previous experiences and corresponds to other Wound-QoL validation studies27,28.
Item distribution characteristics such as mean, standard deviation (SD), percentage of items at the lower (floor effects) and the higher end (ceiling effects) were inspected. For internal consistency Cronbach’s alpha was measured. Scores above 0.70 were interpreted as acceptable29. Explorative factor analysis was conducted to test for structural validity. Difference in scores between T1 and T2 were tested using Wilcoxon signed-rank test. To test for responsiveness and convergent validity, the Wound-QoL scores were correlated with the EQ-5D and FLQA-w (Spearman’s correlation). All analyses were conducted using SPSS version 23 (IBM, Armonk, NY, USA).
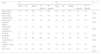
RESULTSBaseline characteristicsIn the five centres, a total of 115 patients were recruited, including 45 (39.1 %) with venous leg ulcers, four (3.5 %) with mixed leg ulcers and four (3.5 %) with arterial leg ulcers (Table 1). Mean age was 69.5 (SD 14.5) years (median 73, min 28 - max 97), 60.0 % were female. Mean observation time was 9.6 (SD 6.6) weeks. Mean wound size at T1 was 18.9 (SD 36.1) cm², and 1.9 (SD 8.0) cm² at T2 (p < 0.001). Overall, 78 (67.8 %) of the wounds showed complete healing, 110 (95.7 %) an improvement of more than 10 % which was considered relevant.
Demographic and clinical characteristics of study participants at baseline (N = 115)
| Mean | SD | |
|---|---|---|
| Age (years) | 69.5 | 14.5 |
| Wound duration (months) | 13.7 | 27.8 |
| Wound size (cm²) | 18.9 | 36.1 |
| n | % | |
|---|---|---|
| Sex | ||
| Male | 46 | 40.0 |
| Female | 69 | 60.0 |
| Employment | ||
| Yes | 13 | 11.3 |
| No | 102 | 88.7 |
| Wound etiology | ||
| Pressure | 5 | 4.3 |
| Venous | 45 | 39.1 |
| Arterial | 4 | 3.5 |
| Mixed | 4 | 3.5 |
| Burn | 1 | 0.9 |
| Tumoral | 2 | 1.7 |
| Traumatic | 16 | 13.9 |
| Post-surgical | 13 | 11.3 |
| Radiodermitis | 1 | 0.9 |
| Diabetic foot | 3 | 2.6 |
| Martorell | 15 | 13.0 |
| Others | 6 | 5.2 |
| Total | 115 | 100.0 |
Mean Wound-QoL at T1 was 1.9 (SD 1.0) and 0.8 (SD 0.9) at T2 (p < 0.001), mean FLQA-w health state concerning the wound was 5.1 (SD 2.7) at T1 and 8.1 (SD 2.1) at T2 (p < 0.001) (Table 2). VAS pain reduced from 4.9 (SD 3.4) to 0.9 (SD 1.7) (p < 0.001).
Results of HRQoL measurement using Wound-QoL, FLQA-w scales (scale 0–10) and pain (NRS, scale 0–10) at baseline (T1) and follow-up (T2)
| Score | T1 | T2 | p* | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Median | 1st quartile | 3rd quartile | Mean | SD | Median | 1st quartile | 3rd quartile | ||
| Wound-QoL, global score | 1.9 | 1.0 | 1.8 | 1.1 | 2.8 | 0.8 | 0.9 | 0.4 | 0.1 | 1.3 | < 0.001 |
| Wound-QoL, subscale body | 1.6 | 1.2 | 1.4 | 0.6 | 2.6 | 0.4 | 0.8 | 0.2 | 0.0 | 0.4 | < 0.001 |
| Wound-QoL, subscale psyche | 2.5 | 1.2 | 2.8 | 1.6 | 3.4 | 1.2 | 1.2 | 0.8 | 0.2 | 2.2 | < 0.001 |
| Wound-QoL, subscale everyday-life | 1.7 | 1.3 | 1.7 | 0.5 | 2.8 | 0.8 | 1.1 | 0.2 | 0.0 | 1.0 | < 0.001 |
| FLQA-w, generally | 6.1 | 2.4 | 6.0 | 5.0 | 8.0 | 7.3 | 2.1 | 7.0 | 6.0 | 9.0 | < 0.001 |
| FLQA-w, concerning the wound | 5.1 | 2.7 | 5.0 | 4.0 | 7.0 | 8.1 | 2.1 | 9.0 | 7.0 | 10.0 | < 0.001 |
| FLQA-w, quality of life | 5.5 | 2.6 | 5.0 | 4.0 | 7.0 | 7.6 | 2.0 | 8.0 | 7.0 | 9.0 | < 0.001 |
| Pain, VAS | 4.9 | 3.4 | 5.0 | 2.0 | 8.0 | 0.9 | 1.7 | 0.0 | 0.0 | 1.0 | < 0.001 |
The Wound-QoL global score in the Spanish version showed high reliability with Cronbach’s alpha > 0.80 in all scales. There were satisfactory distribution characteristics of the global score and the subscales. At T1, 0.9 % had the lowest and the highest possible global score each. At T2, 18.3 % had the lowest possible and 0.9 % the highest possible global score. For the subscales the percentage of patients with the lowest possible score ranged between 2.6 % and 12.2 % at T1 and between 20.9 % and 48.7 % at T2. The percentage of the highest possible score in the subscales was between 7.8 % and 15.7 % at T1 and between 0.9 % and 2.6 % at T2.
Structural validityIn the explorative factor analysis, N = 115 patients who completed the Wound-QoL at T1 visit were included. Three factors with an eigenvalue > 1 were found, explaining 71.0 % of the overall variance. All items loaded on the intended components and the subscales body (items #1 to #5), psyche (items #6 to #10) and everyday-life (items #11 to #16) could be confirmed.
Convergent validity and responsivenessConvergent validity with other instruments (Table 3) and responsiveness were satisfactory (Table 4).
Convergent validity with other instruments at baseline (T1) and follow-up (T2)
| Convergent validity of Wound-QoL global score with | T1 | T2 | |
|---|---|---|---|
| EQ-5D-3L score | r | -0.586 | -0.434 |
| p | < 0.001 | < 0.001 | |
| n | 111 | 109 | |
| EQ-VAS | r | -0.148 | -0.245 |
| p | 0.114 | 0.008 | |
| n | 115 | 115 | |
| FLQA-w health state, generally | r | -0.155 | -0.255 |
| p | 0.099 | 0.006 | |
| n | 115 | 115 | |
| FLQA-w health state, concerning the wound | r | -0.507 | -0.376 |
| p | < 0.001 | < 0.001 | |
| n | 115 | 115 | |
| FLQA-w health state, quality of life | r | -0.441 | -0.294 |
| p | < 0.001 | 0.001 | |
| n | 115 | 115 | |
| Pain (VAS) | r | 0.710 | 0.315 |
| p | < 0.001 | 0.001 | |
| n | 115 | 115 | |
r, correlation coefficient; p, two-tailed significance/Spearman’s correlation; EQ-5D, EuroQoL five dimensions questionnaire; EQ-5D-3 L, EuroQoL five dimensions three level questionnaire; FLQA-w, Freiburg Life Quality Assessment for wounds; QoL, quality of life; VAS, visual analogue scale.
Responsiveness: correlation of change in Wound-QoL global score with change in other scores
| Parameter | Correlation with change (difference T2-T1) in Wound-QoL global score | ||
|---|---|---|---|
| r | p | n | |
| EQ-5D* | 0.576 | < 0.001 | 107 |
| EQ-VAS* | 0.150 | 0.111 | 115 |
| Pain* | 0.605 | < 0.001 | 115 |
| FLQA-w health state, generally* | 0.186 | 0.046 | 115 |
| FLQA-w health state, concerning the wound* | 0.557 | < 0.001 | 115 |
| FLQA-w health state, quality of life* | 0.388 | < 0.001 | 115 |
| Wound size reduction [%] | 0.317 | < 0.001 | 115 |
*difference T2-T1.
r, correlation coefficient; p, two-tailed significance/Spearman’s correlation; EQ-5D, EuroQoL five dimensions questionnaire; EQ-VAS, EuroQoL visual analogue scales; FLQA-w, Freiburg Life Quality Assessment for wounds; QoL, quality of life.
The Wound-QoL was considered a simple and feasible tool by the vast majority of patients. Mean time needed for completely answering was 5.2 (SD 6.4) minutes at T1 and 5.5 (SD 3.6) at T2. Overall, 99.1 % of participants found it easy to understand the questions and 94.7 % stated that the questionnaire suits the personal situation.
DISCUSSIONAssessment of PRO is an essential component of management for chronic wounds1. Patients have a variety of quality of life impairments, which results in very individual treatment needs that need to be assessed and included in the treatment plan2,5. Measurement of HRQoL as a key construct in the PRO concept has been recommended by most authorities and medical societies in wound care24,30. The condition-specific HRQoL instrument Wound-QoL was developed and validated for such measurements both in clinical trials and in routine care3,4,20.
The aim of this study was to validate a Spanish version of the Wound-QoL for language validity as well as for psychometric validity in the same project. The procedures for both validation steps followed international standards. Patients were selected in routine care, thus providing a broad sample of healthcare in wound centres in Spain.
Limitations of the current study relate to the fact that the patients were only recruited in a limited number of centres. Thus, a selection bias cannot be excluded. However, we chose patients in real-world settings of different clinics. Thus, there is no evidence that the selection will impact the validation properties. Furthermore, the instrument has not been changed in items and thus may not meet all areas of burden in the Spanish population. However, for the sake of comparability on an international level, the items need to be kept in the same manner. Furthermore, we have not observed any elevated rates of missing items or objections in the pre-test, which would signal reduced applicability in Spanish.
Overall, the Spanish Wound-QoL showed good psychometric properties that resemble the characteristics of the original version20. Floor and ceiling effects were low for T1. For T2, higher floor effects were found, which can be interpreted as a positive effect of treatment on HRQoL impairment and may thus indicate good responsiveness of the Wound-QoL to clinical improvement. Moreover, patients reported a great level of understanding and accepting the questionnaire. The time for answering the questions was around five minutes and only few data were missing.
CONCLUSIONSThe Spanish version of Wound-QoL is a valid and feasible tool with high patient acceptance to assess HRQoL in clinical care and in clinical trials in Spain. Since the current translation and validation process happened in Spain, further adaptations for other regions like Latin America need to be considered.
Conflict of InterestM. Augustin is the licence holder of the Wound-QoL. The authors otherwise do not have any conflict of interest.
We thank the study centres and their clinical staff for excellent support. We also gratefully acknowledge our team for support in publication management, Mario Gehoff, Pia Dahlhoff and Sabine Ahrendt.
Please cite this article as: Conde Montero E, Sommer R, Augustin M, Blome C, Cabeza Martínez R, Horcajada Reales C, et al. Validación de la versión española del cuestionario Wound-QoL. Actas Dermosifiliogr. 2021;112:44–51.