Chondrodermatitis nodularis helicis (CNH) is a benign inflammatory disease that affects the skin and cartilage of the helix and, less frequently, the antihelix. Intense pain on touching the affected area is reported by many patients with CNH, necessitating treatment. The etiology of CNH is unknown. However, it has been proposed that prolonged pressure on the atrial and perichondrial cartilage, an anatomical region with little protective subcutaneous cellular tissue, may result in local ischemia followed by transepithelial removal of degenerated material. Consequently, many authors consider CNH a form of perforating dermatosis.1 Risk factors include chronic actinic damage, exposure to low temperatures, and repeated local trauma.2 Treatment is challenging. Several therapeutic approaches, with varying cure rates, are described. We present 2 cases of CNH treated successfully with 2% topical diltiazem, a therapeutic option not described to date.
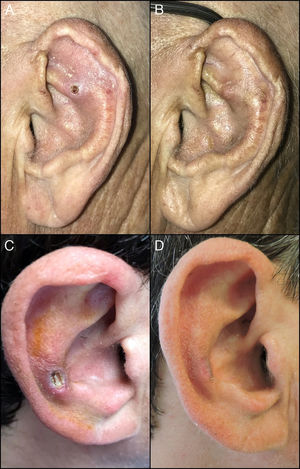
The first patient was a 74-year-old man who was seen for an erythematous nodule with central ulceration on the left antihelix (Fig. 1A). The lesion was painful to the touch and had appeared 4 months earlier. The second patient was a 46-year-old man with a history of chronic hepatitis C virus infection and parenteral drug addiction who was seen for a painful nodule with severe ulceration on the right antihelix (Fig. 1C). The lesion had appeared 6 months earlier and had not responded to corticosteroids or topical antibiotic treatment. In both cases, a clinical diagnosis of CNH was established and the patients were treated with an extemporaneous preparation of 2% diltiazem gel applied 3 times per day for 3 months (Table 1). No other concurrent treatments were administered during this period. By the end of the treatment period both patients showed marked improvements in the clinical appearance of the lesions and reported almost complete disappearance of the pain (Figs. 1B and 1D). No adverse effects associated with the procedure were observed.
There are a range of therapeutic options for CNH, including cryotherapy, scraping, devices to protect the ear from external pressure, topical or intralesional corticosteroids, carbon dioxide laser, photodynamic therapy with methyl-aminolevulinate,3 and nitroglycerin administered at different concentrations either topically or via a transdermal patch. Cure rates of up to 92% have been reported in patients treated with 2% nitroglycerin gel, the most common adverse effect of which was transient headache (17% of patients).4,5 Comparable cure rates and markedly better tolerance have been reported in patients treated with 0.2% nitroglycerin.6 Surgical procedures, of which several are described,8,9 offer cure rates of up to 82%.7
Diltiazem acts by selectively blocking calcium channels in muscle, inducing vasodilation. Oral diltiazem is used to treat arterial hypertension and angina pectoris, and as an antiarrhythmic agent. In CNH, topical diltiazem has an effect similar to that of topical nitroglycerin, inducing relaxation of the arteriolar smooth muscle, restoring local blood flow, and reversing ischemia in cartilage. The low dose of diltiazem administered in topical formulations results in absorption of a very small quantity of the drug, likely reducing the probability of systemic adverse effects.
In general surgery, topical diltiazem has been used successfully for many years for the treatment of chronic anal fissure. In this context, diltiazem has shown greater clinical efficacy than nitroglycerin in randomized controlled trials, and almost no adverse effects.10
We have carried out an exhaustive review of the literature and found no existing reports describing the use of topical diltiazem to treat CNH. Further research will be needed to determine whether the use of other excipients (e.g., oil/water emulsion instead of gel) increases the therapeutic efficacy of topical diltiazem. A limitation of this report is that it consists of only 2 clinical cases. Nonetheless, because topical diltiazem shows good efficacy, is well tolerated, and has a known mechanism of action, we feel that it should be considered as a novel therapeutic option for CNH.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: de Quintana-Sancho A, Carnero-González L, González-Pérez R, Drake-Monfort M. Utilidad del diltiazem tópico al 2% en la condrodermatitis nodular del hélix: descripción de 2 casos. Actas Dermosifiliogr. 2019;110:251–253.