The patient was a clinically stable 54-year-old woman who had been diagnosed with Takayasu arteritis 15 years earlier and was receiving treatment with 5mg of prednisone daily and 20mg of methotrexate weekly. The patient came to our department for assessment of asymptomatic skin lesions that had appeared exclusively on her elbows in the previous 6 months.
Physical ExaminationPhysical examination revealed multiple mildly erythematous papular lesions measuring 2mm in diameter, each with central umbilication, distributed symmetrically on both elbows (Fig. 1).
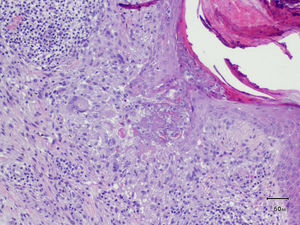
HistopathologyA punch biopsy of one lesion showed an inflammatory infiltrate in the superficial dermis containing histiocytes, several multinucleated giant cells, and lymphocytes expressing T and B immunohistochemical markers, without significant atypia or the presence of lymphocytes in the epidermis. Collagen degeneration was present, with a discrete mucin deposit. Elimination of a material consistent with degenerated collagen through epidermal interruptions was observed in certain areas of the lesion (hematoxylin-eosin, original magnification ×100) (Fig. 2).
What Is Your Diagnosis?
DiagnosisPerforating granuloma annulare.
Clinical Course and TreatmentThe patient was informed that the process was benign and treatment was started with topical methylprednisolone. A slight improvement in the lesions was achieved after several weeks.
CommentPerforating granuloma annulare (GA) is a rare variant of GA (occurring in 3%-5% of cases) that was first described by Calnan1 in 1951 and later by Owens and Freeman2 in 1971. The most common site is the limbs in children and young adults. Perforating GA has been reported in association with diabetes mellitus (especially in generalized cases), tuberculosis, rheumatoid arthritis, human immunodeficiency virus infection, tattoo application, and as Wolf's isotopic response after a herpes zoster infection.3
The etiology and pathogenesis of perforating GA are not fully understood, although it is believed that this entity could be related to a delayed hypersensitivity reaction mediated by helper T cells in the presence of an exogenous antigen. Unlike other forms of GA, perforating GA lesions are located in the most superficial portion of the dermis due to the transepidermal elimination of degenerated collagen.
The clinical presentation of perforating GA consists of skin-colored or slightly erythematous papules measuring 1-5mm, with central umbilication. The papules can be scattered or grouped forming annular lesions, as in classic granuloma annulare.
The differential diagnosis should include various entities. Acquired perforating dermatosis is the most common type of perforating disease, occurring in up to 10% of patients on hemodialysis; lesions typically appear on the extensor surfaces of the limbs and the clinical course is marked by self-resolving flares.4 In contrast, perforating GA follows a more chronic clinical course. Reactive perforating collagenosis is a rare familial disorder that first appears during childhood. As in perforating GA, the perforating material in reactive perforating collagenosis is collagen. In elastosis perforans serpiginosa, however, the perforating material consists of elastic fibers. The lesions consist of keratotic papules with a serpiginous distribution, affecting the neck, face, and flexural areas.
Follicular mycosis fungoides can manifest as papules centered on a follicle, which can be mistaken for the central umbilication seen in perforating GA, although histology shows a dense perifollicular infiltrate of atypical T cells, occasionally with involvement of the follicular epithelium, in addition to specific immunohistochemical characteristics. Follicular mycosis fungoides most frequently affects the head and neck, unlike perforating GA, which usually affects the limbs. In follicular mucinosis, the lesions tend to group in inflammatory plaques, sometimes causing alopecia, and can be either primary or secondary to a hematologic neoplasm, generally mycosis fungoides.
Given the autoimmune context of our patient, erythema elevatum diutinum was also considered in the differential diagnosis. This entity presents as erythematous brownish or purpuric papules or plaques on the extensor surfaces of the limbs and is characterized histologically by vasculitis with progressive concentric perivascular fibrosis.
Various treatments have been used in perforating GA, including topical corticosteroids or calcineurin inhibitors, imiquimod, intralesional corticosteroids, cryotherapy, and surgical excision, all with unsatisfactory results.5
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Lloret-Ruiz C, Barrado-Solís N, Quecedo-Estébanez E. Pápulas umbilicadas en los codos en una paciente con una vasculitis sistémica. Actas Dermosifiliogr. 2018;109:353–354.