The cellular neurothekeoma is a rare benign tumor of uncertain histogenesis.1,2 It was first thought to be the same as nerve sheath myxoma, but it is now known to be a different entity. The tumor appears in young women in the first 3 decades of life as a single papular or nodular lesion, of pale erythematous, pink or normal skin color. It arises on the head or neck. Histologically it is a nonencapsulated tumor formed of epithelioid and spindle-shaped cells, occasionally with poorly-defined margins. It develops in the dermis and in the subcutaneous cellular tissue and can extend down to the muscle plane. Occasionally, a degree of cellular atypia has been described, though this does not appear to affect the prognosis. The treatment of choice is surgery; recurrence is related to involvement of the surgical margins.
In recent years there has been an increase in the use of imaging studies in dermatology, not only as diagnostic tools but also to complete the preoperative workup for tumors.3–5 Dermatologic high-frequency ultrasound has shown the greatest development.
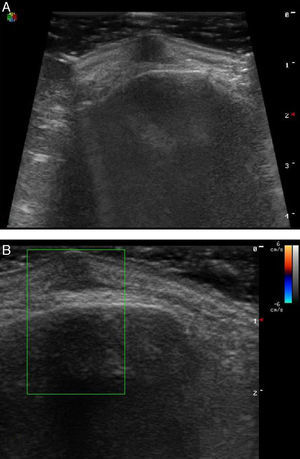
We present the case of a woman of 51 years of age, with a past medical history of fibromyalgia on treatment with paracetamol and diazepam. She was seen for a lesion in the left supraciliary region that had appeared 2 years earlier and had grown progressively. The lesion produced local pain. Physical examination revealed a clearly delimited, hard subcutaneous tumor with no changes in the overlying skin. The lesion was more palpable than visible. Skin ultrasound showed a clearly delimited hypoechoic lesion of 7.51×5.62mm, with no posterior acoustic enhancement or shadow; the lesion was located in the dermis and reached the muscle plane but did not affect the bone (Fig. 1A). Doppler ultrasound showed no increased vascularity within the lesion or at its margins (Fig. 1B). Histopathology was compatible with a cellular neurothekeoma with cellular atypia. It was decided to perform complete excision of the lesion, which was found to reach the muscle plane. The patient has been followed up in outpatients for 3 months and has presented no clinical signs of recurrence.
High-frequency skin ultrasound was introduced recently to dermatology and it has been used as a technique to complement physical examination.3–5 Ultrasound has certain advantages compared with other imaging studies (computed tomography [CT] and magnetic resonance [MRI]) in the field of neoplastic skin disease: it is a rapid and noninvasive technique that can be performed in the outpatient clinic, avoiding delays, and it offers a complete image of the lesion in real time; it distinguishes between the layers of the skin and skin or nail lesions of less than 3mm5; it is less costly4,5; it does not involve ionizing radiation, and can therefore be used in children, pregnant women, and patients with pacemakers5; and, as with CT or MRI, it provides information on the anatomy of the region, thus being of considerable assistance when planning surgery.3–5 However, further research is still needed to consolidate the technique and to create a library of ultrasound patterns and nomenclature common to the different disease processes.
Despite the above, there are few references in the literature on the use of imaging studies in the workup for cellular neurothekeoma,6–8 and none of these has used ultrasound. CT shows neurothekeoma as a well-defined, round or oval, hypodense or isodense lesion.6,7 The MRI image is isointense or hypointense in T1 and hyperintense in T2.6–8 Kamo et al.8 used MRI in the preoperative workup of a cellular neurothekeoma with poorly-defined borders in the nasal region of a young patient and reported that it can be useful in cases of poorly defined lesions. Finally, positron emission tomography with fluorodeoxyglucose shows a homogeneous increase in metabolic uptake in the lesion.6
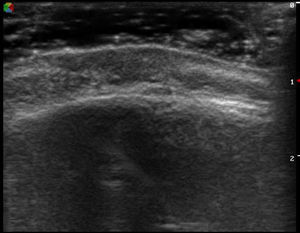
In our case, dermatologic high-frequency ultrasound enabled certain clinically common tumors to be ruled out (Table 1). In addition, it revealed that it was not a vascular or malignant lesion as, in addition to the infiltrative features of the lesion, there would have had to be evidence of increased vascularity of the lesion; bone involvement was also ruled out, which helped when planning surgery. Recently we have also had the opportunity to use ultrasound to evaluate a microcystic adnexal carcinoma in the same anatomic region and with a similar clinical presentation. That lesion presented as a hypoechoic tumor with infiltrating borders, but in contrast to the neurothekeoma, there were also hyperechoic spots (Fig. 2), corresponding to the corneal cysts described in the histological study.
Ultrasound differential diagnosis of tumor lesions.
| Skin Tumors | Ultrasound Description |
|---|---|
| Epidermal cyst | Dermal or subdermal tumor with variable interior pattern (homogeneous, heterogeneous) and posterior enhancement and lateral oblique shadows. It may show a drainage channel to the surface (punctum) as a hypoechoic line. It is not usually vascular |
| Lipoma | Subcutaneous tumor of variable echogenicity (it typically shows parallel hyperechoic lines), with poor vascularity. Compression is different to the adjacent fat |
| Pilomatrixoma | Dermal or subdermal tumor with a hypoechoic border (halo sign) and with a hyperechoic interior due to calcifications that produce an acoustic shadow. Doppler reveals vascularity |
| Dermoid cyst | Well-defined, hypoechoic tumor adherent to deeper planes and that does not show posterior enhancement |
| Dermatofibroma | Poorly defined, hypoechoic dermal tumor that does not usually present visible blood vessels |
| Plexiform neurofibroma | Lesions with a hypoechoic periphery and hyperechoic center |
| Cellular neurothekeomaa | Clearly defined, hypoechoic dermal tumor with no posterior enhancement or acoustic shadow. No increased vascularity |
| Microcystic adnexal carcinoma | Hypoechoic tumor with infiltrating borders and containing hyperechoic spots |
In conclusion, we have presented the ultrasound image of a cellular neurothekeoma located in the left ciliary region of a 51-year-old woman. Although histopathology continues to be the gold standard for the definitive diagnosis, and further research is necessary to establish a common ultrasound pattern of the neurothekeoma, we consider dermatologic high-frequency ultrasound to be a noninvasive and rapid diagnostic tool that helps to distinguish this tumor from other subcutaneous lesions and that can define the lesion preoperatively.
Please cite this article as: Aguado Lobo M, Echeverría-García B, Álvarez-Garrido H, Borbujo J. Neurotequeoma celular: descripción ecográfica. Actas Dermosifiliogr. 2015;106:522–524.