We present a 7-year-old girl with no past history of interest, who was seen for an asymptomatic lesion that had arisen in the right axilla 3 months earlier and had grown progressively, but that had remained stable after a cycle of cryotherapy in her health center 2 months earlier. Examination revealed a well-defined oval papule in the right axilla. The papule was of yellowish color centrally and more erythematous peripherally. No drainage orifice was present and no material was emitted when pressure was placed on the lesion (Fig. 1).
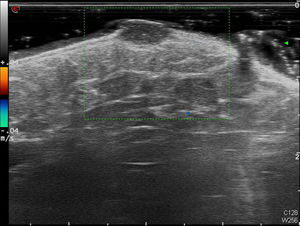
Color Doppler ultrasound (Esaote MyLabClass C with an 18MHz transducer) was performed, showing a well-defined, homogeneous, hypoechoic lesion in the dermis, measuring 6.5×3.5mm, and that depressed the subcutaneous cellular tissue (Fig. 2). No posterior enhancement or lateral shadow was observed. Color Doppler showed no flow within the lesion.
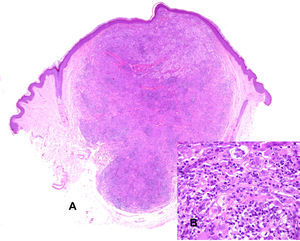
We performed complete excision of the lesion. Histopathology study revealed a diffuse histiocytic proliferation that occupied the full thickness of the dermis (Fig. 3A). The lesion was formed of cells with isomorphic oval nuclei and eosinophilic cytoplasm and foam cells, some of which were multinucleated, including occasional Touton-type cells (Fig. 3B). These cells were accompanied by numerous lymphocytes. No epidermotropism was observed. The diagnosis was xanthogranuloma.
A, A diffuse histiocytic proliferation occupies the full thickness of the dermis. Hematoxylin and eosin, original magnification×20. B, At higher power, the proliferation is seen to be formed of cells with isomorphic oval nuclei and eosinophilic cytoplasm, together with foam cells, some of which are multinucleated, including occasional Touton-type cells. Hematoxylin and eosin, original magnification×400.
Juvenile xanthogranuloma (JXG) is a benign histiocytic tumor characterized by being most common in the first 2 decades of life. Various classifications place this lesion in the non-Langerhans cell histiocytoses, together with other diseases such as disseminated xanthoma, diffuse eruptive histiocytosis, benign cephalic histiocytosis, and sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease).
JXG is the most common histiocytic disease of childhood,1 though its incidence may be underestimated due to the indolent, asymptomatic nature of these solitary lesions and their tendency to resolve spontaneously.
Clinically, it presents as yellowish papulonodular lesions in the skin and other organs, but it is not associated with metabolic disorders. It is the most common form of non-X histiocytosis and shows no racial or sex differences. Two clinical forms are recognized, both typically asymptomatic. The papular form with firm reddish or yellowish lesions of 2 to 5mm in diameter, located in the skin or rarely in the mucosas; and the less common, nodular form, which develops as an isolated or small number of round, brownish-red or yellowish lesions of 1 to 2cm in diameter. The 2 forms can coexist and can arise at any of the sites affected by this disease: lung, heart, gastrointestinal tract, central nervous system, adrenal glands, pituitary gland, bone, bone marrow, kidney, eyes.
The differential diagnosis of JXG when it presents as a solitary lesion, as in our patient, should include Spitz nevus, cystic lesions, and certain adnexal tumors, such as pilomatrixoma.
The definitive diagnosis of JXG is made on histopathology, which, in early lesions, shows a monomorphic infiltrate of histiocytes that contain no lipids and that can occupy the full thickness of the dermis, or at least the upper half of the dermis. Mature lesions contain foam cells and Touton-type giant cells, located particularly in the superficial dermis and at the border of the infiltrate, and fibrosis may be observed. Lymphocytes, neutrophils, and eosinophils may sometimes also be seen. Immunohistochemistry shows that the histiocytes in the infiltrate usually express CD68, CD163, Factor XIIIa, and CD4 and are negative for protein S-100,3,4 which facilitates their differentiation from Langerhans cell histiocytosis and Rosai-Dorfman disease.
Although the definitive diagnosis of JXG is histological, we consider that ultrasound can be a useful noninvasive diagnostic tool. The ultrasound findings in our patient were very similar to those of an earlier description of the ultrasound image of JXG in an adult, which showed a lesion in the dermis with no posterior enhancement or lateral shadow.5
The sonographic differential diagnosis of JXG should include other vascular lesions such as infantile hemangioma, in which greater vascularity is usually observed on Doppler and more marked epidermal alterations are present, induced by the underlying lesion.5
The ultrasound image of JXG can be differentiated from epidermal and other cysts because those cystic lesions are usually anechoic or hypoechoic with anechoic bands.6 Tumors that arise from the hair matrix, such as pilomatrixomas, present sonographically as hypoechoic lesions with different degrees of internal echogenicity, producing a posterior acoustic shadow.7
Solivetti et al.2 described 5 ultrasound images of pilomatrixomas that varied from a completely calcified lesion, in which only the posterior acoustic shadow was observed (type1) to one with a pseudoneoplastic, hypoechoic appearance, with increased vascularity on Doppler (type5). The ultrasound features of basal cell carcinoma (BCC) differ from those of JXG in that BCC is a hypoechoic lesion that contains hyperechoic spots within its substance.8,9Table 1 summarizes the ultrasound characteristics of other tumors and lesions that are common in childhood.10
Ultrasound Features of Lesions Common in Childhood.
| Juvenile Xanthogranuloma | Pilomatrixoma | Infantile Hemangioma | Dermoid Cyst | Dermatofibroma | |
|---|---|---|---|---|---|
| Gray scale | Homogeneous, hypoechoic, dermal | Five types described.2 Hyperechoic areas. Posterior acoustic shadow | Hypoechoic, formed of a more or less homogeneous stroma (more stroma than channels) | Deep hypoechoic lesion with linear hyperechoic images internally | Homogeneous, with poorly defined borders, dermal |
| Color Doppler | No vascularity | No vascularity except type 52 | Abundant vascularity | No vascularity | Occasionally vascular |
We have presented a patient with JXG that was excised surgically and we have correlated the clinical and histopathological features with the ultrasound findings on 3 images of the lesion.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Martínez-Morán C, Echeverría-García B, Tardío JC, Borbujo J. Imagen ecográfica de xantogranuloma juvenil. Actas Dermosifiliogr. 2017;108:683–685.