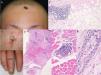
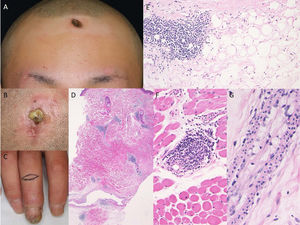
A 24-year-old male was referred to our hospital, complaining of recalcitrant ulcers on the forehead and scalp. Physical examination showed well-demarcated ulceration and depressed scars on the forehead, scalp and upper arm (Fig. 1A, B). In addition, he had swollen and cold fingers with ulceration of the tip of the third finger with nail fold extension (Fig. 1C). He noticed Raynaud’s phenomenon and morning stiffness one year previously. Antinuclear antibodies (1:640, nucleolar and homogeneous), and positive anti-Scl-70 antibodies (16 U/mL; normal <10) were detected in the serum, whereas antibodies against centromere, RNA polymerase III, SS-A, SS-B, DNA, ds-DNA, cardiolipin, and Sm were all within normal limits. A biopsy specimen taken from the forehead revealed fibrosis of the lower dermis and subcutaneous tissues, focal infiltration of mononuclear cells in the lower dermis and subcutaneous fat tissues, and hyaline fat degeneration (Fig. 1D). Furthermore, perivascular mononuclear cell infiltration was observed in the muscle tissues (Fig. 1E). Xanthomatous cells were detected in the dermis, which were positive for CD68. Alcian blue stain revealed mucin deposition in the dermis. Of note, foam cells were detected within the blood vessels in the lower dermis (Fig. 1G). Examination by direct immunofluorescence showed linear deposition of IgM in the epidermal basement membrane. A second biopsy specimen from the finger showed thickened collagen bundles in the dermis. A third biopsy from the forearm showed edematous dermis with slightly thickened collagen bundles in the lower dermis. Although detailed examination denied pulmonary, renal and esophageal involvement, the symptoms of the patient fulfilled the 2013 classification criteria of systemic sclerosis proposed by American College of Rheumatology/European League against Rheumatism.1 Oral prednisolone (PSL) (30 mg/day) was started along with intravenous administration of alprostadil. The ulcer was epithelialized six months later. Thereafter, PSL was gradually tapered, and in turn, dapson (50 mg/d) was started. He is well-controlled under 8-10 mg/d oral PSL, without recurrence of ulcers.
Ulcerative lesions on the forehead (A) and scalp (B), along with swollen fingers and nailfold bleeding (C). Histological features showing focal lymphohistiocytic infiltration and hyaline fat necrosis in the lower dermis to the subcutis (D, E). Lymphocytic infiltration was observed in the muscle layers (F). Foam cells were detected in the vessels (G).
Lupus erythematosus profundus (LEP) is a subtype of chronic cutaneous LE with or without systemic lupus erythematosus (SLE). Additionally, LEP is rarely seen in patients with connective tissue diseases other than SLE. Association between LEP and systemic sclerosis (SSc) is extremely rare, and only a few cases have been reported to date.2 Association with LEP and SSc is extremely rare, and thus the etiology of the present case is unclear. The present case suffered from SSc, and detailed examination denied SLE and mixed connective tissue disease (MCTD). However, it was interesting to observe overlapping conditions of scleroderma and LEP in our case. He developed sclerosis of the upper extremities, but without organ involvement. LEP was developed on the forehead, scalp, and upper extremity. A recent report reviews 20 cases of lupus panniculitis of the scalp, which involved the parietal (70%), frontal (45%), temporal (40%), occipital (30%), and vertex (10%) regions.3 Ulcer was observed in 10%.
To date, only a few cases of ulcerative LEP have been reported,4,5 and microangiopathic processes such as segmental fibrinoid vascular necrosis, small vessel thrombosis, and dense angiocentric lymphocyte infiltrates have been suggested. Ishiguro et al. speculated that intractable ulcers occurred as a result of necrobiotic changes in the subcutaneous tissues caused by vascular changes.5 On the other hand, xanthomatous reaction was detected in the fibrotic tissue of LEP.6 In the present case, vasculitis was not observed but foam cells were detected in the dermis as well as within the blood vessels. It was speculated that xanthomatous cells were induced by phagocytosis of lipid peroxides caused by macrophage-derived oxygen radicals following destruction of sebaceous glands initiated by immune complex deposition,7 which may have induced circulation abnormalities and also tissue damages. Moreover, cellular infiltrates were observed not only in the subcutaneous tissues but also in the muscle layers, and thus those tissue damages may have led to the ulceration of LEP in this case.
Please cite this article as: Mori T, Ito T, Kikuchi N, Yamamoto T. Lupus eritematoso profundo ulcerativo en un paciente con esclerosis sistémica cutánea limitada. Actas Dermosifiliogr. 2021. https://doi.org/10.1016/j.ad.2019.10.016