Osler-Weber-Rendu disease, otherwise known as hereditary hemorrhagic telangiectasia (HHT), is characterized by the presence of epistaxis and multiple mucocutaneous telangiectases in association with arteriovenous malformations affecting different organs, including the lungs, the gastrointestinal system, and the central nervous system. The prevalence of the disease varies, with rates ranging from 1 case per 5000 people to 1 case per 8000 people. HHT is an autosomal dominant disorder with high penetrance. Most patients have mutations in the endoglin (ENG) or activin receptor-like kinase I (ACVRL1) genes. ENG and ACVRL1 mutations affect the signaling of transforming growth factor β, which is a cytokine involved in angiogenesis.1,2 A mutation in the SMAD4 gene has also been described in a small proportion of patients with HHT, who may have associated juvenile polyposis syndrome.3
HHT is diagnosed on the basis of the Curaçao criteria, which include epistaxis (spontaneous or recurrent), multiple mucocutaneous telangiectases in characteristic locations, visceral lesions (gastrointestinal, pulmonary, hepatic, or cerebral arteriovenous malformations), and a diagnosis of HHT in at least 1 first-degree relative. The diagnosis is considered definitive if 3 or more of these criteria are met, possible if 2 criteria are met, and unlikely if fewer than 2 criteria are met.
Mucocutaneous telangiectases are the most evident sign of HHT. Apart from being cosmetically bothersome, these lesions can cause bleeding and have a considerable impact on quality of life in 27% of cases. Skin lesions are uncommon in childhood and tend to appear after the second decade. Although numerous studies have described the use of lasers to treat various types of facial telangiectases (e.g., idiopathic telangiectases, Civatte poikiloderma, rosacea), little has been published on their use in the treatment of telangiectases in patients with HHT. In this study, we describe our experience with the use of a long-pulse Nd:YAG laser to treat mucocutaneous manifestations of HHT.
Nine patients referred to the dermatology department at Hospital Universitario Cruces in Baracaldo, Spain, received long-pulse Nd:YAG laser treatment for HHT-related telangiectases between January 2012 and December 2014. The patients’ characteristics are summarized in Table 1. All the lesions were treated with a Cynergy long-pulse Nd:YAG laser (Cynosure), which emits monochromatic light with a wavelength of 1064nm. A skin cooling system with air flow levels of between 5 and 7 (Cryo 5, Zimmer Medizinsysteme GmbH) was used to protect the skin during treatment.
Clinical Characteristics of Patients, Laser Settings, and Treatment Results.
| Patient | Sex | Age, y | Location of Lesions | Gene Involved | No. of Laser Sessions; Settingsa | Improvement (% Clearanceb) | Level of Satisfactionc | Level of Paind |
|---|---|---|---|---|---|---|---|---|
| 1 | Woman | 40 | Face Fingers | ACVRL1 | 7; Nd:YAG (5-20-115) | 4 | 10 | 5 |
| 2 | Woman | 62 | Face Tongue | ACVRL1 | 4; Nd:YAG (5-15-135) | 3 | 10 | 7 |
| 3 | Woman | 60 | Face Fingers | ACVRL1 | 1; Nd:YAG (5-25-145) | 4 | 10 | 5 |
| 4 | Woman | 40 | Face | ACVRL1 | 1; Nd:YAG (5-20-120) | 4 | 9 | 1 |
| 5 | Man | 63 | Face Tongue | ACVRL1 | 1; Nd:YAG (5-15-125) | 3 | 10 | 1 |
| 6 | Man | 63 | Face Tongue | ACVRL1 | 1; Nd:YAG (5-20-125) | 4 | 10 | 1 |
| 7 | Woman | 68 | Face Fingers Tongue | ENG | 1; Nd:YAG (5-20-120) | 4 | 5 | 6 |
| 8 | Man | 48 | Face | ENG | 1; Nd:YAG (3-15-100) | 1 | 1 | 2 |
| 9 | Woman | 55 | Tongue | ACVRL1 | 3; Nd:YAG (5-20-135) | 4 | 10 | 6 |
Sedation with nitrous oxide (Entonox) was necessary in just 2 cases. In our experience, lesions located on the finger pulp are particularly painful. In 1 patient with lesions affecting the tongue, we used a topical anesthetic spray (lidocaine, Xilonibsa) to numb the oral mucosa. The rest of the patients tolerated the treatment well without local anesthesia.
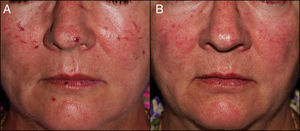
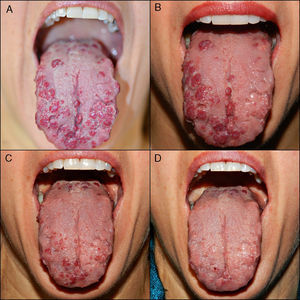
The treatment achieved considerable clearance of both skin (Fig. 1) and mucosal (Fig. 2) lesions in few sessions (mean, 2.2 sessions; range, 1-7 sessions), and there were no notable adverse effects such as scarring, persistent purpura, or dyschromia. Patient #2 experienced posttreatment bleeding that was resolved by compression. The best outcomes were observed with the following laser settings: a 5-mm spot size, a pulse time of 15 and 25ms, and a mean fluence of 127.5J/cm2 (range, 115-145J/cm2). As a precaution, in patients with lesions of the posterior tongue, we treated just one side of the tongue per session. The patients experienced postoperative swelling, but there were no signs of dyspnea or dysphagia. As postoperative treatment, we recommended an antiseptic mouthwash and oral prednisone at a dose of 0.5mg/kg for 3 days to reduce swelling. The worst outcome was observed for patient #8, who was treated with a spot size of 3mm and a fluence that was probably insufficient. We suggested undergoing a second session, but the patient decided not to, as the treatment had been for cosmetic purposes only.
A, Multiple telangiectases, with episodes of spontaneous bleeding, on the tongue of patient #9. B, Result of 1 treatment session, in which the left dorsum and lateral surface of the tongue were treated. Note the difference with respect to the right, untreated side. C, Result after 2 sessions, with treatment of the whole surface of the tongue. D, Result after 3 treatment sessions. Note the excellent clearance achieved.
Numerous types of lasers have been described in the treatment of mucocutaneous telangiectases in HHT, namely, a pulsed KTP laser (532nm), an Nd:YAG laser (1064nm), a diode laser (810nm), and a pulsed dye laser.4–7 There have also been reports of cases treated with argon and carbon dioxide lasers, although these offer little specificity for the wavelengths of hemoglobin.8,9
In the case of pulsed dye lasers, more sessions have been found to be necessary to achieve clearance of telangiectases in patients with HHT than in those without. This is possibly because of the aberrant structure of blood vessels or abnormal vascular remodeling in HHT.5
Fernández-Jorge et al.10 described the combined use of an intense pulsed light laser and a long-pulse Nd:YAG laser to treat telangiectases in 3 patients with HHT. All of the patients experienced good cosmetic outcomes and a reduced frequency of bleeding episodes.
Nd:YAG laser therapy is an effective treatment for mucocutaneous telangiectases in patients with HHT. In our series, excellent results were obtained with few sessions and no remarkable adverse effects. However, due to the natural course of the disease, patients should be followed and new lesions retreated as necessary.
Please cite this article as: de Quintana-Sancho A, Díaz-Ramón JL, Acebo-Mariñas E, Cánovas-Fernández A. Tratamiento de las manifestaciones mucocutáneas en la telangiectasia hemorrágica hereditaria con láser pulsado Nd:YAG (1.064nm). Actas Dermosifiliogr. 2016;107:171–173.