An otherwise healthy 50-year-old woman consulted for pruritic skin lesions on her left foot that had first appeared 2 years previously. The lesions had not improved after treatment with oral and topical corticosteroids and antifungal agents.
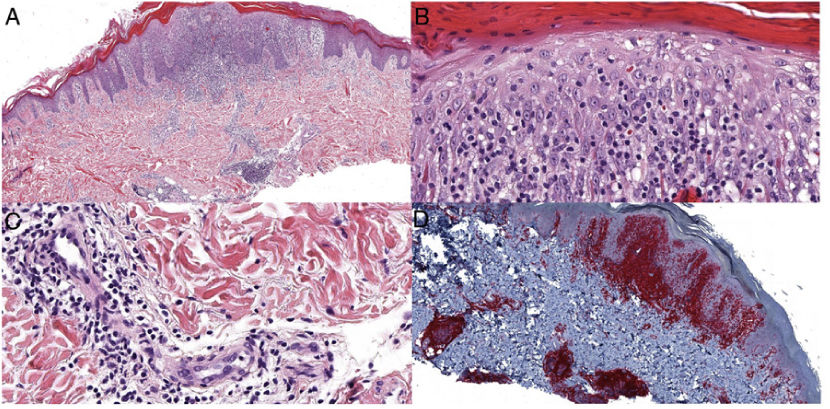
Physical ExaminationThe physical examination revealed multiple erythematous-desquamative papules on and between the toes of her left foot (Fig. 1). No further lesions were identified on the rest of her skin. No pathological locoregional enlarged lymph nodes were present.
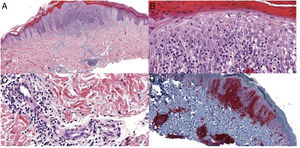
HistopathologyBiopsy revealed a superficial band-like lymphoid infiltrate and a deep infiltrate surrounding the glands and eccrine ducts. Changes resulting from syringometaplasia and marked epidermotropism were also visible (Fig. 2 A-C). Immunohistochemistry was intensely positive for CD3 and CD4 (Fig. 2 D), weakly positive for CD8, and negative for CD30. T-cell receptor gene rearrangement was monoclonal.
The remaining additional tests revealed the following: glucose, 91 mg/dL; urea, 36 mg/dL; creatinine, 0.59 mg/dL; aspartate aminotransferase, 11 IU/L; alanine aminotransferase, 10 IU/L; alkaline phosphatase, 72 IU/L; γ-glutamyl transferase, 12 IU/L; total proteins, 7.7 g/L; lactate dehydrogenase, 185 U/L; chloride, 100 mmol/L; sodium, 139 mmol/L; potassium, 4.5 mmol/L; β2-microglobulin, 1.65 mg/L; leukocytes, 9900/μL (normal formula); hemoglobin, 13.6 g/dL; mean corpuscular volume, 91.9 fL; and platelets, 174 000/μL. Computed tomography of the thorax, abdomen, and pelvis revealed normal findings.
What is your diagnosis?
DiagnosisSyringotropic mycosis fungoides.
Clinical Course and TreatmentTreatment was started with topical psoralen–UV-A (8-methoxypsoralen 0.1% o/w emulsion) 3 times per week in combination with clobetasol propionate cream 0.05% once daily. After 3 months of treatment, the lesions resolved, except in those areas that were less exposed to sunlight, such as the interdigital spaces (Fig. 3).
CommentMycosis fungoides is the most common primary cutaneous lymphoma and a classic mimicker of other skin conditions. While multiple clinical, pathological, and clinicopathological variants have been described, the only ones recognized in the latest classification of cutaneous lymphomas of the World Health Organization (WHO) (2016) are folliculotropic mycosis fungoides, pagetoid reticulosis, and granulomatous slack skin syndrome. Syringotropic mycosis fungoides is a very infrequent clinicopathological variant; in other words, it has distinctive clinical and histopathologic characteristics1. Given that this condition can be confused with other chronic skin conditions, diagnosis is challenging and requires a high degree of suspicion.
Clinically, mycosis fungoides can be generalized or localized, with a predilection for palms and soles, in the form of patches and/or erythematous-desquamative papules and plaques. Owing to adnexal involvement, these can occur with alopecia, anhidrosis, or follicular accentuation, similar to the folliculotropic variant, from which it may be clinically indistinguishable, except for the anatomical distribution of the lesions. Moreover, classic mycosis fungoides lesions can appear on other areas of the body.
Histologically, the condition is characterized by a superficial band-like infiltrate of atypical lymphocytes, as well as a deep infiltrate, which is more prominent around the eccrine glands. Concomitant involvement of the follicle is observed in 75% of cases2. The characteristics of the infiltrate, together with the finding of syringometaplasia, help to differentiate histologically with respect to the folliculotropic variant3. Similarly, other classic characteristics of mycosis fungoides are often present, for example, epidermotropism. However, the clinical-histopathological correlation is essential when attempting to confirm the diagnosis of this uncommon presentation.
The differential diagnosis should include other clinical pictures such as dyshidrotic eczema, contact dermatitis, and perniosis, in which the differentiating characteristic, in addition to the absence of epidermis and syringotropism, is the presence of lymphocytic vasculitis. Furthermore, it is important to differentiate this condition from the abovementioned folliculotropic MF, since the syringotropic version has an indolent course with a better prognosis. The condition known as syringolymphoid hyperplasia is currently considered a type of syringotropic mycosis fungoides2.
In addition to traditional approaches to mycosis fungoides, various therapies have been proposed for the solitary, or localized, forms of syringotropic mycosis fungoides, including psoralen–UV-A and local radiotherapy, with generally favorable responses reported4. Owing to the depth of the tumor infiltrate, treatments targeting the skin may not be effective5.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Castiñeiras González J, Sánchez Sambucety P, Rodríguez Prieto MÁ. Pápulas acrales resistentes al tratamiento. Actas Dermosifiliogr. 2022;113:83–84.