Sensitive scalp is sensitive skin located on the scalp. Sensitivity is considered primary in the absence of an associated scalp disorder and secondary when caused by conditions such as psoriasis, seborrheic dermatitis, and atopic dermatitis.
The clinical manifestations of primary sensitive scalp are subjective. Common presenting symptoms are burning, itching, trichodynia, and dysesthesia, often coinciding with hair loss. Clinically, the skin appears normal or red. An objective diagnosis based on laboratory or histologic findings is not possible. Triggers may be endogenous (e.g., stress and emotional or psychopathological disturbances) or exogeneous (e.g., topical products and cosmetics). Treatment must be individualized. Options include pimecrolimus, hydration with hyaluronic acid, and mesotherapy with plasma rich in growth factors.
El cuero cabelludo sensible es una piel sensible de localización especial. Puede ser primario, cuando se presenta sin enfermedad del cuero cabelludo, y secundario, cuando es atribuible a procesos como psoriasis, dermatitis seborreica, dermatitis atópica y otros.
Las manifestaciones clínicas de la forma primaria son subjetivas. El escozor, el picor, la tricodinia y las sensaciones disestésicas son el motivo de consulta, muy a menudo coincidiendo con alopecia. Clínicamente la piel del cuero cabelludo puede ser normal o eritematosa. No hay datos de laboratorio o histológicos específicos para un diagnóstico objetivo. Los factores desencadenantes son endógenos, como el estrés y las alteraciones emocionales y psicopatológicas, o ambientales, como los tópicos inadecuados y los cosméticos. El tratamiento debe ser personalizado, incluyendo pimecrolimus, la hidratación con ácido hialurónico y la mesoterapia con plasma rico en factores de crecimiento.
Sensitive scalp is difficult to classify.1 Some consider it a manifestation of a specific skin disease, whereas others consider it to be a clinical entity in and of itself.
The controversy surrounding the existence or not of sensitive scalp as a disease can be better understood if we compare it to that surrounding sensitive skin in its day2,3 and which was eventually resolved with the 2017 publication of a study providing a consensus-based definition reached using the Delphi methodology and carried out by a group of European experts at the International Forum for the Study of Itch. The definition read as follows: “A syndrome defined by the occurrence of unpleasant sensations (stinging, burning, pain, pruritus, and tingling sensations) in response to stimuli that normally should not provoke such sensations. These unpleasant sensations cannot be explained by lesions attributed to any skin disease. The skin can appear normal or be accompanied by erythema. Sensitive skin can affect all body locations, especially the face.”
This statement resolved the controversy once and for all, leaving sensitive skin classed as a stand-alone and independent syndrome that can affect various areas of the skin, including the scalp.4
DefinitionSensitive scalp is sensitive skin at a specific site. The consensus-based definition of sensitive skin4 states this implicitly when it says that the condition can affect various areas of the skin. This is stated explicitly in other studies, such as that of Saint-Martory et al.,5 whose analysis of 400 individuals with a mean age of 40 years recruited at a dermatology clinic and a cosmetic clinic revealed that 85% had sensitive skin on the face and that 70% had sensitive skin at other sites, as follows: hands (58%), feet (34%), neck (27%), trunk (23%), back (21%), and scalp (36%), which is the site that interests us here.
We can classify sensitive scalp into 2 types6:
- •
Primary, which manifests in isolation or alongside alopecia (any type).
- •
Secondary, which occurs alongside a skin disease of the scalp such as seborrheic dermatitis, psoriasis, atopic dermatitis, and contact dermatitis.
The current study addresses primary sensitive scalp.
Epidemiological DataThe prevalence of sensitive scalp can be deduced from studies analyzing the prevalence of sensitive skin that refer to sensitive scalp. The studies include that of Willis et al.,7 who found a prevalence of 25% in the general population, and that of Misery et al.,2 who found a prevalence of 70%.
All the studies agree on the greater frequency of sensitive scalp in women, which is 10–30% greater than in men,8 and some report that women perceive reactions affecting the skin more intensely than men.9
No notable statistical evidence is available with respect to age and race. The differences that can be observed in clinical practice between races are likely due more to psychosocial and cultural factors, such as lifestyle, hygiene, and pollution than to genetic factors.10,11
Clinical ManifestationsThe clinical manifestations of sensitive scalp include 4 parameters:
- 1.
High subjective sensitivity.
- 2.
Healthy or erythematous skin.
- 3.
Occurrence or nonoccurrence alongside alopecia (any type).
- 4.
Frequent psychological comorbidity.
- 1.
High subjective sensitivity is the basic clinical criterion and the reason why the patient attends the clinic in most cases complaining of stinging, itching, trichodynia, or other abnormal sensations.
- •
In general, the term stinging is closely associated with the emotional component. Unlike pruritus, which leads to scratching, or pain, which is accompanied by despondency and sadness, stinging leads to uncertainty and anxiety, the need for movement, and avoidance of friction. It usually improves with fresh air and cold water.
- •
Pruritus of the scalp has a considerable impact on patient quality of life.12 Scratching becomes a necessity that disrupts concentration and well-being. Pruritus in a person with sensitive scalp does not usually lead to erosions and other lesions that result from scratching.
- •
Trichodynia (“hair pain”) is a painful sensation on the scalp.13 Affected patients report that it appears when they comb their hair, change their parting, and, sometimes, spontaneously. Many patients are somewhat embarrassed when they complain because they doubt that they really feel the pain and find their perception a little strange, since they have never heard of anyone else experiencing this sensation. Trichodynia can affect the whole scalp or specific areas coinciding with bald patches of any type and intensity. Such were the findings of Willimann and Trüeb14 in 2002. These authors reported that of a total of 403 patients they examined with alopecia, 20% of women and 9% of men complained of hair pain, irrespective of its cause and activity. Much more recently, in 2021, although consistent with the previous report, Askin et al.15 reported data on 249 patients from a trichology unit, of whom 35.7% claimed to have experienced trichodynia. The pain was more intense in women and in cases of cicatricial alopecia. As for the origin of trichodynia, many authors associate the symptoms with psychological factors such as depression and anxiety,16 sleep disorders, and stress.17 One study that brings together all these characteristics (association with alopecia of any type, female predominance, association with stress) was that by Kanti et al.,18 where women receiving chemotherapy or tamoxifen for breast cancer reported the appearance of trichodynia and pruritus with onset and duration of hair loss. This psychopathological nature of the symptom is supported by the fact that there were no analytical abnormalities indicative of a metabolic change or deficiency.19,20 Similarly, there are no histological data proving peribulbar follicular inflammation, a hypothesis that was put forward some years ago but has never been proven.21
- •
- 2.
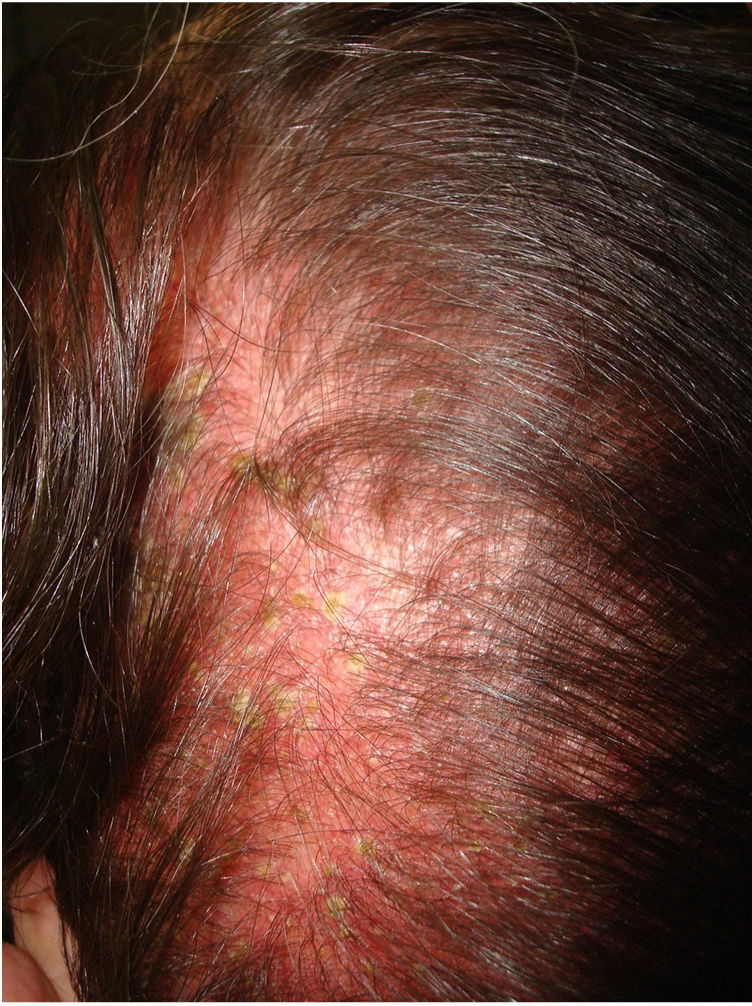
The skin of a person with sensitive scalp may be normal in appearance (Fig. 1) or characterized by more or less intense erythema (Fig. 2). In 1987, Thestrup-Pedersen et al.22 considered erythema to be a basic finding, albeit with a descriptive name—red scalp—and described characteristics that were identical to those we now consider as being sensitive scalp. When examined using a dermatoscope, sensitive scalp is formed by dilated capillaries and telangiectasias, with no other specific findings. The vascular patterns are those of healthy skin, for example, interfollicular simple red loops and arborizing red lines. The finding of other abnormalities corresponds to the accompanying alopecia, if present. The finding of telangiectasias and high subjective sensitivity is sufficient reason for some authors to consider sensitive scalp a type of erythematotelangiectatic rosacea with an unusual location, which may even improve with oral tetracyclines.23 However, the absence of other manifestations of rosacea has led this hypothesis to be rejected. Some studies on sensitive skin report a decrease in the thickness of the epidermis and disruption of the skin barrier. This finding could also be attributed to sensitive scalp.24
- 3.
Sensitive scalp may occur alongside some types of alopecia. As mentioned above,14 alopecia, or more frequently telogen effluvium and androgenetic alopecia, often co-occurs with sensitive scalp, especially if it is associated with trichodynia. In addition, the type or intensity of alopecia is not associated with the intensity of the signs and symptoms of sensitive scalp. However, it is often alopecia that draws attention to the scalp, thus enhancing the subjective perception of sensitivity.15
- 4.
Psychological comorbidity is common in sensitive scalp, especially when the condition is associated with trichodynia (see above). This association has been demonstrated in various psychological evaluations of patients with sensitive scalp, the findings being anxiety, depression, stress, and emotional dysregulation.25–28 Furthermore, the effects of the symptoms of sensitive skin on quality of life could lead to psychopathological abnormalities that were not initially present.25
The true pathophysiology of the process remains uncertain. One theory points to hyperreactivity of the cutaneous nerves, mainly in the case of sensitive scalp with trichodynia.29 Similarly, consistent with the etiology and pathogenesis of sensitive skin, various authors30–32 believe that activation of the transient receptor potential cation channel subfamily V member 1 expressed in nerve endings, keratinocytes, and cells of the immune system triggers release of substance P and other neuropeptides in the skin, leading to subjective symptoms.
TriggersAs in sensitive skin, sensitive scalp can involve a series of triggers that are both endogenous (mainly stress) and exogenous (environment). A typical example of the latter is hair products, since many formulations contain irritants. Even so, it is difficult to determine which is responsible for onset or worsening of sensitive scalp. Thus, in 2021, Brenaut et al.33 published the results of a study of 133 women (mean age, 41 years), of whom 74% reported having sensitive scalp. However, no differences were observed with respect to hair products, except for more frequent use of conditioner in patients with sensitive scalp.
Another exogenous factor to be considered is topical treatments, both for the accompanying alopecia34 (minoxidil) and for sensory symptoms (corticosteroids), which, in many cases, the patient has already taken when consulting. It is also important to take physical procedures such as phototherapy into account.
DiagnosisGiven the limited cutaneous manifestations of sensitive scalp, diagnosis is based on the clinical history, which should record hygiene habits, cosmetics, treatments, factors considered triggers by the patient,35 the result of the physical examination (normal or erythema), and trichoscopy.
Misery et al.36 proposed a new scale, the 3 S questionnaire, for evaluating the intensity of symptoms in sensitive scalp. The questionnaire makes it possible to differentiate between patients with mildly sensitive, sensitive, and very sensitive scalp.
Differential DiagnosisIt is first necessary to distinguish between primary sensitive scalp and secondary sensitive scalp, which always involves lesions on the scalp and, possibly, other areas.
It is also necessary to differentiate between sensitive scalp and scalp dysesthesia associated with lichen simplex chronicus,37 as well as other conditions38 caused by nerve injury, impingement, or irritation, such as trigeminal trophic syndrome, or zoster-associated trigeminal first branch pain.
Lastly, multiple chemical sensitivity, for which no clear diagnostic evidence has yet become available, should be taken into account in some cases.
TreatmentTreatment is summarized in Table 1.
Treatment of Primary Sensitive Scalp.
| 1- Eliminate hair products and topical treatments |
| 2- Specific hair hygiene for sensitive scalp |
| 3- Systemic treatment |
| a. Short oral corticosteroid cycle (prednisone, 0.5mg/kg/d for 7 days and rapid tapering over a further 7 days)a |
| b. Gabapentin (300mg/24h) or pregabalin (75mg/24h) |
| 4- Topical treatment |
| a. Pimecrolimus cream 10mg/g once daily |
| b. Hyaluronic acid for the scalp once or twice daily with an interval of at least 1h before application of pimecrolimus |
| 5- Mesotherapy with platelet-rich plasma tailored to the individual |
The initial approach to sensitive scalp should attempt to eliminate or diminish the triggers, mainly hair products and topical treatments, including mechanical devices and exfoliants, which should be replaced by cleansing products with amphoteric surfactants or soft anions and no common sensitizing agents, cutaneous sensory nerve-mediated vasodilators, or aromas.39 They may contain hydrating elements with proven biocompatibility such as glycerin and hyaluronic acid and relipidizing agents such as vegetable oil or ceramides.3,6,26 Patients receiving topical minoxidil for alopecia can switch to oral minoxidil if there are no contraindications.40
In the fairly common case of a patient who has received relatively long-term therapy with topical corticosteroids, thus favoring telangiectasias and thinning of the epidermis, a cycle of oral corticosteroids should be administered in order to eliminate topical treatment without a rebound effect. Such an approach should be taken in line with usual practice, taking into account contraindications and possible adverse effects. Two weeks’ therapy is generally sufficient, with a continued dose of 0.5mg/kg/d during the first week and rapid tapering during the second.
If the subjective symptoms—stinging, trichodynia, and pruritus—are intense, oral gabapentin can be added, starting at 300mg/d, or pregabalin, at 75mg every 12h. The dose and frequency can be increased if necessary.
The implicit neurogenic inflammation can be controlled, and inflammatory mediators and sensory neuropeptides neutralized, with topical pimecrolimus, a calcineurin inhibitor that acts on TRPV1. The drug should be administered as a cream at 10mg/g once daily.6,41
The integrity of the horny layer can be restored by maintaining the scalp hydrated with hyaluronic acid light-texture formulations administered once or twice daily with an interval of at least 1h before application of pimecrolimus. Below, we provide an example of a transparent fluid gel formulation:
- -
Sodium hyaluronate (more stable than the acid) from 0.1% to 0.5%.
- -
Glycerin 5%.
- -
Hydroxypropyl methylcellulose (cellulose derivative) 1.5%.
- -
Phenonip XB (preservative) 0.6%.
- -
Tween 20 (surfactant) 1%.
- -
Purified water (qs) 100mL.
Mesotherapy with growth factor-rich plasma has several uses and few risks. Some studies have shown it to be effective in multiple cutaneous conditions for improving the skin barrier and reducing its reactivity in alopecia,42 and, specifically, erythema and telangiectasia,43 as in sensitive scalp. We have administered mesotherapy monthly, with tailored intervals according to the response. Outcome is favorable.
Many of these recommendations can also be applied in secondary sensitive scalp, bearing in mind the accompanying peculiarities of the disease. While research on sensitive scalp may yet bear much fruit,44 we believe that management is much simpler if based on the guidelines proposed here.
Conflicts of InterestThe authors declare that they have no conflicts of interest.