A 68-year-old man was examined in our unit due to a long history of intensely pruritic skin lesions on the submandibular angle, scalp, and forearms. He also showed painful novel lesions on the oral, esophageal, and ocular mucosa.
Physical examinationOn examination, erythematous and crusted plaques, approximately 1cm in diameter, were seen on the submandibular region, scalp, and forearms, with poorly defined and excoriated borders (Fig. 1). Additionally, oral ulcers were seen on the palate and buccal mucosa (Fig. 2). At ocular level, the patient showed symblepharon in both eyes without corneal involvement.
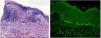
HistopathologyHistopathological examination revealed the presence of subepidermal blistering, along with a predominantly mononuclear infiltrate and fibrosis (Fig. 3A). Direct immunofluorescence studies confirmed the presence of linear deposits of immunoglobulin G, C3, and fibrinogen at the basement membrane (Fig. 3B).
Other supplementary testsOral endoscopy identified several irregularly shaped fibrinous erosions and esophageal stenosis 15cm away from the dental arch. Lab test results, including autoimmune studies with anti-skin antibodies, turned out normal or negative. The Western blot with a hemidesmosome-rich fraction tested positive for IgG vs integrin beta 4. Finally, the in-depth study conducted to rule out any association with malignancy showed no significant pathological findings.
What is your diagnosis?
DiagnosisCicatricial pemphigoid (CP).
Disease progression and therapyThe patient was treated with pulses of methylprednisolone, IV immunoglobulins, cyclophosphamide, and rituximab, which resulted in complete resolution of the skin and mucosal lesions. He experienced a relapse in the oral region, which was treated with dapsone, oral prednisone, and 0.01% triamcinolone acetonide in orabase ointment, which led to the remission of these lesions. However, it was necessary to discontinue this therapy and replace it with sulfasalazine due to the appearance of toxicoderma and anemia. Five months later, the patient remains clinically stable with no new skin or mucosal lesions.
CommentCP is part of a heterogeneous group of blistering diseases of mucous membranes, and less commonly of the skin, mediated by autoantibodies vs proteins located at the dermoepidermal junction.1 Its onset typically occurs between the ages of 60 and 80 years. Its incidence ranges from 1 to 2 cases per million people per year, with no predilection for any specific geographic location or race.1,2 The clinical course of CP is intermittent, with periods of remission and relapse. It often affects the oral mucosa, ocular conjunctiva, skin, pharynx, external genitalia, nasal mucosa, larynx, anus, and esophagus.3 One of the most dreaded complications of this disease is the onset of scarring that can cause significant morbidity through an impaired function of the organs involved.
Numerous antigens located in the hemidesmosomes of the dermoepidermal junction have been identified as targets of autoantibodies in these patients. These antigens include BP180 and BP230 proteins, laminin 332, type VII collagen, and alpha 6 and beta 4 subunits of integrins. Selective involvement of different antigenic targets results in varying clinical expression and, therefore, a different spectrum of disease severity.4
Due to the clinical presentation of CP, the differential diagnosis should include various diseases involving blisters and scarring during their course, among these, the predominantly cutaneous variant of the Brunsting-Perry cicatricial pemphigoid, as initially observed in our patient.5 However, later on, the lesions extended to other sites, resulting in mucous membrane pemphigoid (MMP).
Treatment depends on the severity and location of the lesions. Current evidence recommends a multidisciplinary therapeutic approach involving consensus and collaboration among different specialists based on the patient's organ involvement. Commonly used drugs include potent topical corticosteroids, oral and IV corticosteroids, dapsone, doxycycline, mycophenolate mofetil, azathioprine, methotrexate, cyclophosphamide, IV immunoglobulins, and rituximab.6